儿童脊柱侧弯矫正术需在俯卧位进行,胸廓和腹部受压,会影响患儿的呼吸和循环系统功能,导致胸廓和肺的顺应性降低,心排血量降低[1-3];同时,在该手术体位下,患儿有时需将头部转向一侧,对婴幼儿而言,头部的旋转会使患儿静脉引流受损[4];以上因素均会影响患儿的脑灌注。有研究表明,患儿围手术期脑灌注降低与术后中枢神经系统并发症密切相关[5]。局部脑氧饱和度(regional cerebral oxygen saturation,rScO2)主要采用近红外光谱(near-infrared spectroscopy,NIRS)法监测大脑局部区域的混合血氧饱和度,可提供大脑氧供需平衡实时信息,并间接反映脑血流[6-7]。目前临床上关于儿童俯卧位手术局部脑氧饱和度变化的研究并不多见。本研究旨在观察儿童脊柱侧弯矫正术中体位改变对rScO2的影响,进一步探讨改善患儿脑保护,提高麻醉安全的方法。
材料与方法 一、临床资料收集2019年3月至2019年5月在首都医科大学附属北京儿童医院行脊柱侧弯矫正术的44例患儿作为研究对象。病例纳入标准为:①年龄3~14岁;②脊柱侧弯类型为先天性或特发性;③Cobb's角>40°,侧弯节段位于T3以下;④ASA分级Ⅰ~Ⅲ级;⑤手术时长≥2 h。排除标准:①有颈椎病病史;②患有先天性颈动脉血管病(先天性狭窄或畸形);③伴有先天性心脏病;④T3及T3以上节段脊柱侧弯患儿。本研究纳入的44例患儿中,男童23例,女童21例,年龄3~14岁,平均身高(126.52±24.02)cm,平均体重(29.46±15.70)kg,ASA分级Ⅰ~Ⅲ级,手术时长≥2 h。
二、麻醉方法患儿入室后常规监测心电图(electrocardiogram,ECG)、脉搏血氧饱和度(pulse oxygen saturation,SpO2)、心率(heart rate,HR)、平均动脉压(mean arterial pressure,MAP)和脑电双频指数(bispectral index,BIS)。麻醉诱导前将脑氧饱和度监测仪的传感器贴于患儿双侧前额眉弓上1~2 cm,两侧传感器间距1~2 cm,持续监测患儿左右侧脑氧饱和度。麻醉诱导采用静脉诱导,舒芬太尼0.5 μg/kg、丙泊酚3 mg/kg、罗库溴铵0.6 mg/kg、阿托品0.01 mg/kg。麻醉诱导后监测呼气末二氧化碳分压(end tidal carbon dioxide partial pressure,PetCO2),行桡动脉穿刺监测有创动脉压。麻醉维持采用静脉持续泵入丙泊酚6~10 mg·kg-1·h-1,瑞芬太尼0.2~0.4 μg·kg·min。吸入氧浓度为70%,潮气量为8~10 mL/kg,调整呼吸频率使PetCO2维持在35~45 mmHg,术中将BIS值控制在40~60范围内以保证合适的麻醉深度。
三、观察指标记录患儿吸入纯氧前(T0,基线)、麻醉诱导插管后(T1)、俯卧位前5 min(T2)、俯卧位后5 min(T3)、俯卧位后15 min(T4)、俯卧位后30 min(T5)、俯卧位后45 min(T6)、俯卧位后60 min(T7)、俯卧位后75 min(T8)、俯卧位后90 min(T9)、俯卧位后105 min(T10)、俯卧位后120 min(T11)双侧rScO2值、MAP、HR、SpO2和PetCO2值。吸入纯氧前、麻醉诱导插管后、俯卧位前5 min以及俯卧位后每间隔5 min记录1次患儿的SBP、DBP、HR、SpO2和PetCO2值。记录出血量和输血补液量,记录手术时间和麻醉时间。
四、统计学方法应用SPSS24.0统计学软件对数据进行分析。为了避免未知不对称性(左右大脑前循环)对脑氧饱和度结果的影响,该研究分别分析了左右两侧的rScO2值。符合正态分布的计量资料以均数±标准差(x±s)表示,不符合正态分布的计量资料以中位数和四分位数间距表示。采用配对t检验用来比较左右两侧rScO2值,仰卧位转俯卧位后各时间点的所有观察指标的比较采用单因素方差分析,与T0或T2时间点观察指标的比较采用Dunnett-t检验。以P<0.05为差异有统计学意义。
五、伦理审查该研究经首都医科大学附属北京儿童医院伦理委员会批准(伦理编号:2019 -15),所有患儿父母在手术前均签署书面知情同意书。
结 果 一、各观察时点左右两侧rScO2值比较本研究分别比较了患儿左右两侧rScO2,经配对t检验表明左右两侧rScO2无明显差异(P>0.05)(表 1)。
|
|
表 1 各观察时间点左右两侧rScO2比较(x±s) Table 1 Comparison of rScO2 between left versus right side at each observation timepoint(x±s) |
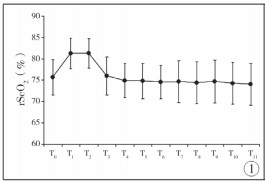
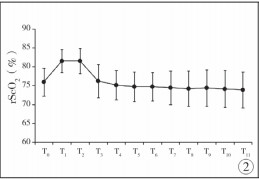
根据Dunnett-t检验分析可知,患儿由仰卧位转为俯卧位后,每一观察时点左右两侧脑氧饱和度值均低于仰卧位水平(P<0.01),俯卧位后2 h内,左侧rScO2由翻身前的81.30%下降至74.05%(图 1),右侧rScO2由翻身前的81.52%下降至73.86%(图 2),具体见表 1。
|
Download:
|
| 图 1 俯卧位前后各观察时间点左侧脑氧饱和度的改变 Fig. 1 Changes of left cerebral oxygen saturation before and after prone position at different timepoints | |
|
Download:
|
| 图 2 俯卧位前后各观察时间点右侧脑氧饱和度的改变 Fig. 2 Changes of right cerebral oxygen saturation before and after prone position at different timepoints | |
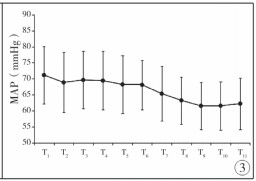
患儿俯卧位前后各观察时点的MAP、HR、SpO2、PetCO2值见表 2。根据Dunnett-t检验分析可知,MAP在T3、T4、T5、T6和T7 5个观察时间点与T2相比无明显差异(P>0.05), T8、T9、T10和T11 4个时间点与T2相比有明显降低(P < 0.05)(图 3);患儿HR、SpO2及PetCO2在T3至T11 9个观察时间点与T2时间点相比均无明显差异(P>0.05)。
|
|
表 2 俯卧位前后各观察时间点HR、MAP、SpO2、PetCO2值(x±s) Table 2 Values of HR, MAP, SpO2 and PetCO2 before and after prone position at different timepoints(x±s) |
|
Download:
|
| 图 3 俯卧位前后各观察时间点MAP的改变 Fig. 3 Changes of MAP before and after prone position at different timepoints | |
rScO2代表局部脑氧饱和度,采用近红外光谱技术进行监测,可连续、实时提供大脑氧供需平衡信息[8]。在脑代谢恒定的情况下,rScO2可准确反应脑血流,因此rScO2的监测对术中可能发生脑缺血的患儿具有重要意义,该技术已广泛应用于成人及小儿外科。在成人领域有研究表明,术中rScO2 <65%的患者神经系统并发症发生率明显增加,患者术中rScO2降低与其术后认知功能障碍及住院时间延长有关[9-11]。
在整个麻醉过程中,从预充氧开始到手术结束,吸入氧浓度均>21%,为了消除吸入氧浓度对本项研究的影响,考虑用俯卧位前5 min的rScO2值代替吸纯氧前rScO2值,将其作为脑氧饱和度的基线值,然后将其与俯卧位后rScO2值进行对比。研究结果表明,儿童脊柱侧弯矫正术中,患儿由仰卧位转为俯卧位后2 h内,每一观察时点的rScO2值均低于仰卧位水平。有文献表明,患儿术中rScO2降低与动脉血压及呼气末二氧化碳下降有关[12, 13]。但在本项研究中,T3~T7 5个时间点,患儿的MAP、HR、SpO2及PetCO2与T2时间点相比并无统计学差异,MAP、HR、SpO2及PetCO2始终居于稳定水平。因此,T3~T7 5个时间点rScO2的降低可能与手术中体位改变有关,患儿由仰卧位转为俯卧位后,会引起rScO2的下降,这与Deiner等[14]的研究结果一致。俯卧位时,患儿胸廓和腹部受压,静脉回流减少,尤其在正压通气下,回心血量进一步减少,心输出量降低,脑血流量下降[15];同时,由于该项研究入组的病例为T3以下节段脊柱侧弯的患儿,患儿俯卧位时头部均摆向一侧,头部旋转造成颈部静脉回流受阻,颅内压增高,脑灌注压与平均动脉压和颅内压有关,颅内压升高时,脑灌注降低,这会导致患儿rScO2降低[16-17]。
Babakhani等[18]研究发现,在俯卧位下行腰椎手术的成人患者由仰卧位转为俯卧位后,双侧rScO2呈现先降低后回升的趋势,在俯卧位90 min后,rScO2逐渐回升至仰卧位水平,且rScO2的降低伴随着血压、心率的下降,rScO2的回升伴随血压、心率的升高。但是,本研究发现患儿由仰卧位转为俯卧位后的1 h内(T3~T7),血压、心率无明显改变,患儿双侧rScO2始终低于仰卧位水平(T2),这可能与小儿新陈代谢速率快,脑氧摄取率高,体位改变对小儿生理及脑灌注造成的影响更大有关。同时,由于该研究只观察了俯卧位后2 h内rScO2的变化特征,俯卧位2 h后rScO2是否可因患儿自身调节功能的改善而发生回升有待进一步探讨。因此,对于俯卧位下行脊柱侧弯矫正术的患儿,应尽量选择头部正中位进行手术,尽可能缩短患儿俯卧位时间,同时维持血流动力学的稳定,避免发生较大的血流动力学波动和脑灌注压的降低,将rScO2维持在较高水平。
研究表明,术中低脑氧饱和度与小儿心脏术后神经功能障碍有关[19]。围术期低脑组织氧合指数(tissue oxygenation index, TOI)会导致患儿ICU停留时间延长,术后气管插管时间延长[20];同时,Gomez-Pesquera[21]的最新研究也发现,小儿非心脏手术中rScO2较基线值降低不超过20%术后发生不良行为改变的概率也会大大增加(根据PHBQ量表进行评价),术中脑氧饱和度的轻度降低也可能对患儿术后造成不良影响。因此,术中在手术体位不可改变的情况下,及时调整MAP、HR、SpO2、PetCO2等因素,尽量将脑氧饱和度维持在正常水平。该研究的局限性是没有对所研究患儿进行术后随访观察,故无法得出儿童先天性脊柱侧弯矫正术中rScO2降低对患儿术后神经系统功能的影响,术中rScO2的降低是否会增加患儿术后神经系统不良反应的发生率,需继续进行更深一步的探讨和研究。
综上所述,患儿术中脑氧饱和度降低与手术体位密切相关,俯卧位会使患儿rScO2降低,因此应尽量缩短患儿俯卧位时间,与外科医生做好沟通,在不影响手术的前提下,俯卧位时尽量选择头部正中位进行手术,减少对颈部血管的压迫。同时,对行此类手术的患儿,更应加强术中脑氧饱和度的监测,保证患儿脑组织正常氧供应。
| 1 |
Kato S, Yoshitani K, Kubota Y, et al. Effect of posture and extracranial contamination on results of cerebral oximetry by near-infrared spectroscopy[J]. J Anesth, 2017, 31(1): 103-110. DOI:10.1007/s00540-016-2275-1. |
| 2 |
Aristokleous N, Seimenis I, Georgiou GC, et al. The Effect of Head Rotation on the Geometry and Hemodynamics of Healthy Vertebral Arteries[J]. Ann Biomed Eng, 2015, 43(6): 1287-1297. DOI:10.1007/s10439-015-1340-5. |
| 3 |
曹隽, 张学军, 曾骐, 等. Nuss手术治疗漏斗胸患儿合并特发性脊柱侧弯的临床研究[J]. 临床小儿外科杂志, 2019, 18(1): 21-25. DOI:10.3969/j.issn.1671-6353.2019.01.004. Cao J, Zhang XJ, Zeng Q, et al. Clinical study of correcting scoliosis plus pectus excavatum with Nuss procedure in children[J]. J Clin Ped Sur, 2019, 18(1): 21-25. DOI:10.3969/j.issn.1671-6353.2019.01.004. |
| 4 |
Skowno J, Vutskits L, McGowan F, et al. Staying away from the edge-cerebral oximetry guiding blood pressure management[J]. Paediatr Anaesth, 2015, 25(7): 654-655. DOI:10.1111/pan.12698. |
| 5 |
Kussman BD, Wypij D, Laussen PC, et al. Relationship of intraoperative cerebral oxygen saturation to neurodevelopmental outcome and brain magnetic resonance imaging at 1 year of age in infants undergoing biventricular repair[J]. Circulation, 2010, 122(3): 245-254. DOI:10.1161/CIRCULATIONAHA.109.902338. |
| 6 |
Andersen JD, Baake G, Wiis JT, et al. Effect of head rotation during surgery in the prone position on regional cerebral oxygen saturation A prospective controlled study[J]. Eur J Anaesthesiol, 2014, 31(2): 98-103. DOI:10.1097/EJA.0000000000000028. |
| 7 |
Adler AC, Stayer SA. The Insight From Foresight:Near-Infrared Spectroscopy in Cyanotic Congenital Heart Disease[J]. Anesth Analg, 2017, 125(1): 18-19. DOI:10.1213/ANE.0000000000002154. |
| 8 |
肖婷, 禹二友, 朱义, 等. 二氧化碳气腹对小儿腹腔镜手术期间无创脑氧饱和度的影响[J]. 临床小儿外科杂志, 2018, 17(4): 317-320. DOI:10.3969/j.issn.1671-6353.2018.04.017. Xiao T, Yv EY, Zhu Y, et al. Effects of carbon dioxide insufflation on regional cerebral oxygenation during laparoscopy in children[J]. J Clin Ped Sur, 2018, 17(4): 317-320. DOI:10.3969/j.issn.1671-6353.2018.04.017. |
| 9 |
Olbrecht VA, Skowno J, Marchesini V, et al. An international, multicenter, observational study of cerebral oxygenation during infant and neonatal anesthesia[J]. Anesthesiology, 2018, 128(1): 85-96. DOI:10.1097/ALN.0000000000001920. |
| 10 |
Ballard C, Jones E, Gauge N, et al. Optimised anaesthesia to reduce post operative cognitive decline (pocd) in older patients undergoing elective surgery, a randomised controlled trial[J]. PLoS One, 2012, 7(6): e37410. DOI:10.1371/journal.pone.0037410. |
| 11 |
Casati A, Fanelli G, Pietropaoli P, et al. Continuous monitoring of cerebral oxygen saturation in elderly patients undergoing major abdominal surgery minimizes brain exposure to potential hypoxia[J]. Anesth Analg, 2005, 101(3): 740-747. DOI:10.1213/01.ane.0000166974.96219.cd. |
| 12 |
Razlevice I, Rugyte DC, Strumylaite L, et al. Assessment of risk factors for cerebral oxygen desaturation during neonatal and infant general anesthesia:an observational, prospective study[J]. BMC Anesthesiology, 2015, 16(1): 107. DOI:10.1186/s12871-016-0274-2. |
| 13 |
Ki SH, Rhim JH, Park JH, et al. Quantitative analysis of the effect of end-tidal carbon dioxide on regional cerebral oxygen saturation in patients undergoing carotid endarterectomy under general anaesthesia[J]. Br J Clin Pharmacol, 2018, 84(2): 292-300. DOI:10.1111/bcp.13441. |
| 14 |
Deiner S, Chu I, Mahanian M, et al. Prone position is associated with mild cerebral oxygen desaturation in elderly surgical patients[J]. PLoS One, 2014, 9(9): e106387. DOI:10.1371/journal.pone.0106387. |
| 15 |
冯芳, 胡西贝, 韩明明, 等. 目标导向液体治疗对脊柱侧弯矫形手术患者术中局部脑氧饱和度和术后并发症的影响[J]. 临床麻醉学杂志, 2019, 35(4): 319-322. DOI:10.12089/JCA.2019.04.002. Feng F, Hu XB, Han MM. Effects of goal-directed fluid therapy on intraoperative regional cerebral oxygen and postoperative complications in patients undergoing spinal scoliosis surgery[J]. J Clin Anesthesio, 2019, 35(4): 319-322. DOI:10.12089/JCA.2019.04.002. |
| 16 |
Pesek M, Kibler K, Easley RB, et al. The upper limit of cerebral blood flow autoregulation is decreased with elevations in intracranial pressure[J]. Neurosurgery, 2014, 75(2): 163-170. DOI:10.1227/NEU.0000000000000367. |
| 17 |
Kooi EMW, Verhagen EA, Elting JWJ, et al. Measuring cerebrovascular autoregulation in preterm infants using near-infrared spectroscopy:an overview of the literature[J]. Expert Rev Neurother, 2017, 17(8): 801-818. DOI:10.1080/14737175.2017.1346472. |
| 18 |
Babakhani B, Heroabadi A, Hosseinitabatabaei N, et al. Cerebral Oxygenation Under General Anesthesia Can Be Safely Preserved in Patients in Prone Position[J]. J Neurosurg Anesthesiol, 2017, 29(3): 291-297. DOI:10.1097/ANA.0000000000000319. |
| 19 |
Hoffman GM, Brosig CL, Mussatto KA, et al. Perioperative cerebral oxygen saturation in neonates with hypoplastic left heart syndrome and childhood neurodevelopmental outcome[J]. J Thorac Cardiovasc Surg, 2013, 146(5): 1153-1164. DOI:10.1016/j.jtcvs.2012.12.060. |
| 20 |
Suemori T, Skowno J, Horton S, et al. Cerebral oxygen saturation and tissue hemoglobin concentration as predictive markers of early postoperative outcomes after pediatric cardiac surgery[J]. Paediatr Anaest, 2016, 26(2): 182-189. DOI:10.1111/pan.12800. |
| 21 |
Gomez-Pesquera E, Poves-Alvarez R, Martinez-Rafael B, et al. Cerebral Oxygen Saturation and Negative Postoperative Behavioral Changes in Pediatric Surgery:A Prospective Observational Study[J]. J Pediatr, 2019, 208: 207-213. DOI:10.1016/j.jpeds.2018.12.047. |
 2020, Vol. 19
2020, Vol. 19


