2. 海南省妇女儿童医学中心(海南省儿童医院),海口 570312;
3. 上海市浦东新区浦南医院神经外科,上海 200125;
4. 上海市浦东新区三林社区卫生服务中心,上海 200120;
5. 上海交通大学医学院附属上海儿童医学中心分子诊断实验室,上海 200127
2. Hainan Women and Children's Medical Center (Hainan Children's Hospital), Haikou 570312, China;
3. Department of Neurosurgery, Shanghai Punan Hospital of Pudong New Area, Shanghai 200125, China;
4. Shanghai Sanlin Community Health Service Center of Pudong New Area, Shanghai 200120, China;
5. Molecular Diagnostics Laboratory, Shanghai Children's Medical Center, Shanghai Jiao Tong University School of Medicine, Shanghai 200127, China
软骨发育不全(achondroplasia,ACH) 也称胎儿型软骨营养障碍,是由于软骨内骨化缺陷导致的一种先天性发育异常,主要影响长骨生长,是短肢侏儒症的最常见形式。ACH最早由Parrot于1878年正式命名并系统描述,是常染色体显性遗传性疾病。其发病机制与成纤维细胞生长因子受体-3(fibroblast growth factor receptor 3,FGFR-3)基因跨膜区的点突变密切相关,80%~90%的病例为散发,大多数患儿父母正常,此机制最早由Shiang于1994年提出[1]。
ACH患儿可能具有脑积水、颈髓脑干压迫、椎管狭窄(颈椎和腰椎)、脊髓空洞症、胸腰椎后突畸形及颈椎不稳等神经系统改变[2]。本研究回顾性分析2015年5月至2019年9月海南省妇女儿童医学中心(海南省儿童医院)及上海市浦东新区浦南医院收治的3例软骨发育不全合并脑积水患儿诊疗经过,并复习相关文献,总结该病的临床表现、诊断方式及治疗方法,供临床参考。本研究通过海南医科大学第一附属医院伦理委员会审核批准(2025-KYL-115)。
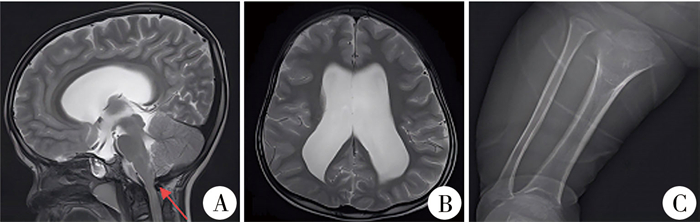
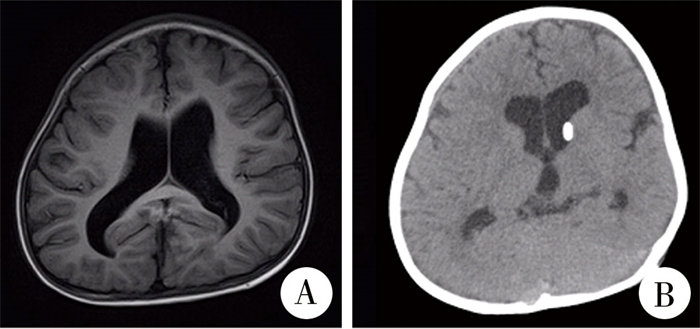
资料与方法 一、临床资料患儿A,女性,6岁,身高70 cm,头围54 cm,因“头围增大、四肢短小”入院。影像学检查提示侧脑室扩大,下肢胫腓骨短,干骺端膨大(图 1)。未监测到睡眠呼吸暂停现象。枕骨大孔表面积1.12 cm2[枕骨大孔表面积=枕骨大孔长度(即枕骨大孔前后缘中点之间的距离)×枕骨大孔宽度(即枕骨大孔最大侧弯点之间的距离)× π/4)][3]。Wanebo等[4]在研究中测得枕骨大孔平均表面积为(8.20±1.00)cm2,本研究以此为标准判断枕骨大孔狭窄。
|
图 1 软骨发育不全合并脑积水患儿A头颅MRI及下肢胫腓骨X线平片 Fig.1 Cranial MRI and lower-limb tibia-fibula X-ray plain film of Patient A with ACH complicated by hydrocephalus 注 A:枕骨大孔缩窄,延髓有卡压;B:侧脑室显著扩大;C:下肢胫腓骨短,干骺端膨大 |
采取靶向基因高通量测序(测序数据使用美国SoftGenetics公司MutationSurveyorⓇ软件进行分析。阳性为在FGFR3基因9号外显子区域发现一个杂合的错义突变c.1138G>A,p.Gly380Arg,提示存在FGFR3基因突变,诊断为遵循常染色体显性遗传的FGFR3基因突变所致软骨发育不全。
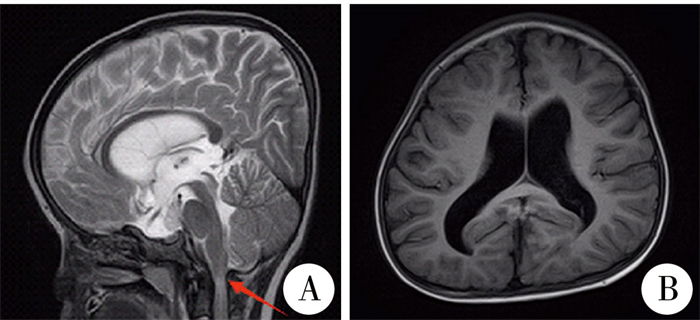
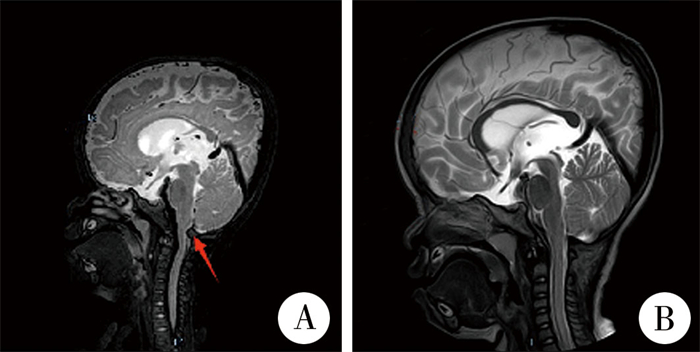
患儿B,女性,2岁,身高56 cm,头围49.7 cm,因“四肢短小、进行性头围增大”入院。影像学检查提示侧脑室显著扩大,未监测到睡眠呼吸暂停现象,枕骨大孔表面积0.82 cm2,提示枕骨大孔缩窄,卡压延髓(图 2)。靶向基因高通量测序提示FGFR3基因突变。
|
图 2 软骨发育不全合并脑积水患儿B的头颅MRI检查结果 Fig.2 Cranial MRI findings of Patient B with ACH complicated by hydrocephalus 注 A:枕骨大孔缩窄,延髓有卡压;B:侧脑室显著扩大 |
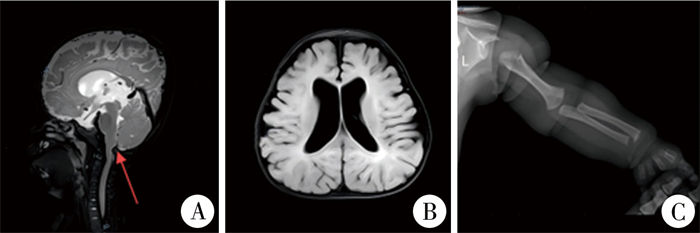
患儿C,女性,8月龄,身高65 cm,头围45 cm,因“四肢短小、进行性头围增大”入院。影像学检查提示侧脑室扩大,监测到睡眠呼吸暂停现象,枕骨大孔表面积0.50 cm2,提示枕骨大孔明显缩窄,卡压延髓,肱骨及尺桡骨粗短,以肱骨明显,干骺端增宽(图 3)。靶向基因高通量测序提示FGFR3基因突变。
|
图 3 软骨发育不全合并脑积水患儿C头颅MRI及左侧肱骨和尺桡骨X线平片 Fig.3 Cranial MRI and left humerus and radius-ulna X-ray plain films of Patient C with ACH complicated by hydrocephalus 注 A:枕骨大孔明显缩窄,延髓明显卡压;B:侧脑室显著扩大,脑指数3.1;C:左侧肱骨及尺桡骨粗短,以肱骨明显,干骺端增宽,尺桡骨干骺端略呈喇叭状,骨皮质增厚 |
患儿A和患儿B采取脑室腹腔分流术。取左侧颞顶小切口,切开各层,暴露硬膜,硬膜穿刺后置入Codman抗感染管。患儿A颅内压为22 cmH2O (1 cmH2O=0.098 kPa)、患儿B颅内压为16 cmH2O。脑脊液(cerebrospinal fluid, CSF)均引流通畅。脑室端接可调压阀,阀门远端接分流管腹腔端,由通条经皮下引至腹部剑突下小切口,置入腹腔,压力均设置为10 cmH2O。
患儿C采取神经内窥镜下三脑室造瘘术+后颅窝减压术。枕下开颅切除枕骨大孔后环及寰椎后环,切除颈延髓部后缘异常增厚的纤维韧带环,充分减压,避免切开硬脑膜;于右额冠状缝前1.0 cm、中线旁开1.0 cm处取横切口,置入神经内窥镜,于第三脑室底电凝开窗球囊扩张直径至0.6 cm,见下方桥前池、基底动脉及脑干,退出神经内窥镜,隧道填塞,骨瓣复位固定。
三、文献检索方法检索1989—2023年PubMed、万方医学网、中国知网中公开发表的文献,中文检索词为“软骨发育不全合并脑积水”、“脑积水”、“软骨发育不全”。英文检索词为“achondroplasia complicated by hydrocephalus”、“hydrocephalus”、“achondroplasia complicated”。文献纳入标准:软骨发育不全合并脑积水的病例报告或临床研究型文献。排除标准:①文献报告数据不全,资料不齐;②信件、会议摘要或同一数据来源的文献。
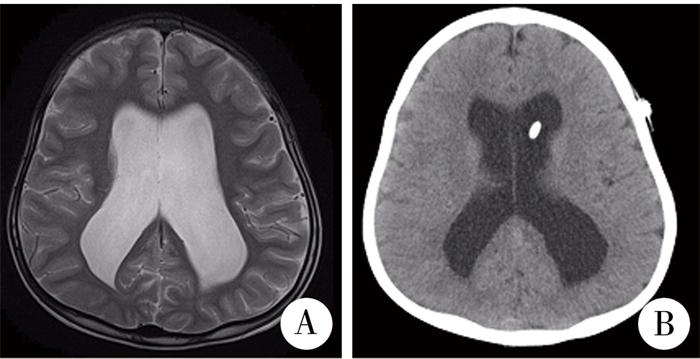
结果3例患儿术后均经止血、抗感染、营养神经等治疗后顺利康复,出院时无一例发生明显并发症,均随访1年,复查头颅MRI显示脑积水明显好转,见图 4至图 6。
|
图 4 软骨发育不全合并脑积水患儿A术前及术后1年头颅MRI对比 Fig.4 Preoperative and 1-year postoperative cranial MRI comparison of Patient A with ACH complicated by hydrocephalus 注 A:术前头颅MRI;B:术后1年头颅MRI显示脑积水明显好转 |
|
图 5 软骨发育不全合并脑积水患儿B术前和术后1年头颅MRI对比 Fig.5 Preoperative and 1-year postoperative cranial MRI comparison of Patient B with ACH complicated by hydrocephalus 注 A:术前头颅MRI;B:术后1年头颅MRI显示脑积水明显好转 |
|
图 6 软骨发育不全合并脑积水患儿C术前和术后1年头颅MRI对比 Fig.6 Preoperative and 1-year postoperative cranial MRI comparison of Patient C with ACH complicated by hydrocephalus. 注 A:术前头颅MRI;B:术后1年头颅MRI显示脑指数3.3,脑积水无进展,枕骨大孔无狭窄 |
共获得相关ACH合并脑积水且符合纳排标准文献13篇,其中英文文献11篇、中文文献2篇(表 1),报道ACH合并脑积水患儿81例,其中6例通过靶向基因高通量测序结合影像学检查确诊,75例经影像学检查确诊。81例中,4例单纯随访观察,28例行脑室腹腔分流术,12例行枕骨大孔减压术,35例行第三脑室造瘘术,1例行颈静脉孔扩大减压术,4例行绕过颈静脉孔血管搭桥术。患儿随访过程中均恢复良好,脑室大小稳定。
| 表 1 既往文献报道软骨发育不全合并脑积水患儿临床资料 Table 1 Clinical data of children with ACH complicated by hydrocephalus reported in the literature |
|
|
ACH合并脑积水患儿病程呈缓慢、持续性进展,如头围增大、四肢短小[18]。少数患儿在婴儿期可能出现阵发性、间断性颅内压增高,导致哭闹、呕吐、嗜睡、前囟张力高、视力障碍等,症状通常间断发生。与其他脑积水患儿相比,头皮静脉怒张在ACH患儿中更常见,可能原因是颈静脉孔狭窄导致静脉部分受压,继而颅内压升高,形成侧支循环,头皮静脉血流增多;另有文献报道2%~5%的ACH合并脑积水患儿1岁以内并发枕骨大孔及颅颈交界处狭窄,可出现猝死[19]。
ACH合并脑积水的特点是FGFR3基因突变引起软骨内骨化缺陷、软骨结合过早关闭,导致颈静脉孔、枕骨大孔、胸廓入口狭窄和后颅窝容积减少[2]。在此基础上靶向基因高通量测序可根据FGFR3基因突变诊断软骨发育不全。X线检查可以显示典型的长骨短缩、干骺端增宽、椎体发育不良等特征。骨盆X线片常显示髂骨翼方形化、髋臼顶水平化等改变。MRI及CT可用于明确脑室扩大情况,尤其是侧脑室以及枕骨大孔是否狭窄[8]。此外,三维CT重建技术可以提供更直观的骨骼畸形信息,更有助于手术规划和预后评估。
ACH合并脑积水的治疗尚有争议。文献报道ACH合并脑积水的发病率为15%~50%,约5%的患儿需要手术干预,进展性脑积水多发生在婴儿期,2岁以后由于代偿机制形成(如颅内外静脉侧支循环建立),患儿脑室内脑脊液处于代偿状态而不表现出颅内高压症状和体征[20]。因此,保守派学者认为这是一种自限性状态,无需干预。本组3例患儿属于进展性过程,笔者总结经验如下:①尽管多数患儿脑室大小和颅内压均在正常范围,但仍需随访,包括神经系统症状、体征及影像学评估;随访频率1岁以内每3个月1次,1岁以上6个月1次,2岁以后趋于稳定,可1年1次。②若患儿头围进行性增大、头皮静脉曲张,头颅CT或MRI提示侧脑室逐渐增大,提示脑积水进展,需要积极手术干预。③若患儿头围快速增大伴前囟突出、落日征、精神和食欲不振,监测颅内压升高,提示脑积水严重,应立即手术治疗。
脑室腹腔分流术:为治疗交通性脑积水的经典手术[2]。Welter在1936年提出,并于1980年由Friedman和Mickle通过血管造影证实ACH合并脑积水患儿常伴有颈静脉孔狭窄,导致颅内静脉窦压力升高,影响脑脊液的吸收与循环,导致交通性脑积水[2];此外,ACH合并脑积水患儿由于并发胸廓畸形、胸廓入口狭小,可压迫颈内静脉致静脉压力升高,影响脑脊液回流而引起交通性脑积水。本组病例A、病例B延髓轻度卡压,第四脑室无明显扩张,未监测到睡眠呼吸暂停现象,证明狭窄的枕骨大孔未导致第四脑室出口梗阻,故采用脑室腹腔分流术。脑室腹腔分流术后可能出现阻塞、感染及术后神经功能缺损[15, 21]。在儿童脑积水专家共识中强推荐采取高压力抗虹吸或可调压脑室-腹腔分流管[22]。另外,抗生素浸渍涂层、银离子涂层和水凝胶涂层的分流管在预防感染方面有一定效果。
枕骨大孔减压术[8]:Dandy[23]于1921年首次观察到ACH合并脑积水患儿后颅窝容积狭小,导致小脑扁桃体下疝、基底池循环受阻、导水管狭窄和第四脑室出口闭塞,从而引起梗阻性脑积水。Cohn[24]通过尸检,首次发现ACH患者的枕骨大孔是狭窄的,后续研究证实ACH合并脑积水患儿常伴有枕骨大孔狭窄,这种狭窄压迫第四脑室出口造成梗阻性脑积水,狭窄的枕骨大孔压迫脑干是患儿早期死亡的主要原因。部分ACH合并脑积水患儿,由于枕骨大孔狭窄压迫脑干、延髓,常伴有呼吸功能紊乱,尤其是睡眠呼吸暂停综合征,严重者可出现截瘫或猝死。多导睡眠图(polysomnography,PSG)有助于监测夜间睡眠呼吸暂停症状的严重程度并判定手术指征和指导手术。2014年,Mukherjee等[9]回顾了单中心11年间8例ACH合并脑积水患儿实施枕骨大孔减压术的资料,结果显示脑积水症状及脑脊液循环明显改善,此手术可能的并发症为脑脊液漏、脑脊液及伤口感染、减压不充分等。
神经内镜三脑室造瘘术(endoscopic third ventriculostomy,ETV)[11、14-15]:2005年Etus等[13]首次将ETV应用于ACH合并脑积水,术后症状明显改善,无并发症。2012年Swift[10]的资料回顾分析了3例ACH并发脑积水患儿行枕骨大孔减压术,术后脑积水无明显改善,再次行神经内镜第三脑室造瘘术,术后随访6.5年,脑室缩小,症状改善。本组病例C若只行枕骨大孔减压术,可能出现减压不充分,故采用神经内窥镜下第三脑室造瘘术联合后颅窝减压术,术后随访1年脑积水无进展,枕骨大孔处无狭窄,导水管通畅。
其他外科治疗方法如颈静脉孔扩大减压术及绕过颈静脉孔的血管搭桥术,均为单个病例报道有效,临床应用较少[16-17]。
综上所述,ACH合并脑积水临床主要表现为头围异常增大及四肢短小,结合影像学检查和靶向高通量基因测序,能准确诊断;虽然ACH并发脑积水发病率不高,但一旦进展需早期外科干预,以缓解颅内高压,同时减轻头颅畸形进展。临床常用治疗方法包括脑室腹腔分流术和(或)枕骨大孔减压术和(或)神经内镜三脑室造瘘术。我们认为术前应仔细评估,根据病情进展、影像学特征及变化选择最佳手术方式,术后应密切随访。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 刘辰源负责文献检索,钟家斐、龚良、王剑、刘辰源负责数据收集,顾硕、刘辰源负责研究结果分析与讨论,刘辰源负责论文撰写,顾硕负责研究设计及全文知识性内容的审读与修正
| [1] |
Shiang R, Thompson LM, Zhu YZ, et al. Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia[J]. Cell, 1994, 78(2): 335-342. DOI:10.1016/0092-8674(94)90302-6 |
| [2] |
Legare JM. Achondroplasia[M/OL]//Adam MP, Feldman J, Mirzaa GM, et al. GeneReviews®[Internet]. Seattle: University of Washington, 2023: 1993-2025[Retrieved December 20, 2022]. https://www.ncbi.nlm.nih.gov/books/NBK1152/.
|
| [3] |
Avci E, Dagtekin A, Ozturk AH, et al. Anatomical variations of the foramen magnum, occipital condyle and jugular tubercle[J]. Turk Neurosurg, 2011, 21(2): 181-190. DOI:10.5137/1019-5149.JTN.3838-10.1 |
| [4] |
Wanebo JE, Chicoine MR. Quantitative analysis of the transcondylar approach to the foramen magnum[J]. Neurosurgery, 2001, 49(4): 934-943. DOI:10.1097/00006123-200110000-00027 |
| [5] |
沈明, 宠宁, 刘培嫦, 等. 软骨发育不全合并脑积水一例的基因诊断及处理[J]. 北京医学, 1999, 21(5): 278. Shen M, Chong N, Liu PC, et al. Gene diagnosis and management of one case of achondroplasia with hydrocephalus[J]. Beijing Med J, 1999, 21(5): 278. DOI:10.3969/j.issn.0253-9713.1999.05.023 |
| [6] |
徐金, 王杭州, 陈民, 等. 软骨发育不全伴脑积水5例诊治分析并文献复习[J]. 中国临床神经外科杂志, 2021, 26(4): 233-236. Xu J, Wang HZ, Chen M, et al. Diagnosis and treatment of achondroplasia patients associated with hydrocephalus (report of 5 cases and literature review)[J]. Chin J Clin Neurosurg, 2021, 26(4): 233-236. DOI:10.13798/j.issn.1009-153X.2021.04.004 |
| [7] |
Yamashita S, Matsumoto Y, Tamiya T, et al. Disappearance of hemifacial spasm after ventriculoperitoneal shunting in a patient with achondroplasia-case report[J]. Neurol Med Chir (Tokyo), 2005, 45(2): 104-107. DOI:10.2176/nmc.45.104 |
| [8] |
Miyamoto J, Tatsuzawa K, Sasajima H, et al. Usefulness of phase contrast cine mode magnetic resonance imaging for surgical decision making in patients with hydrocephalus combined with achondroplasia.Case report[J]. Neurol Med Chir (Tokyo), 2010, 50(12): 1116-1118. DOI:10.2176/nmc.50.1116 |
| [9] |
Mukherjee D, Pressman BD, Krakow D, et al. Dynamic cervicomedullary cord compression and alterations in cerebrospinal fluid dynamics in children with achondroplasia: review of an 11-year surgical case series[J]. J Neurosurg Pediatr, 2014, 14(3): 238-244. DOI:10.3171/2014.5.PEDS12614 |
| [10] |
Swift D, Nagy L, Robertson B. Endoscopic third ventriculostomy in hydrocephalus associated with achondroplasia[J]. J Neurosurg Pediatr, 2012, 9(1): 73-81. DOI:10.3171/2011.10.PEDS1169 |
| [11] |
Shoda K, Ohe N, Sasai H, et al. Endoscopic third ventriculostomy for hydrocephalus in a patient with achondroplasia: a case report and literature review[J]. Childs Nerv Syst, 2021, 37(12): 3907-3911. DOI:10.1007/s00381-021-05129-4 |
| [12] |
Rekate HL. Pathogenesis of hydrocephalus in achondroplastic dwarfs: a review and presentation of a case followed for 22 years[J]. Childs Nerv Syst, 2019, 35(8): 1295-1301. DOI:10.1007/s00381-019-04227-8 |
| [13] |
Etus V, Ceylan S. The role of endoscopic third ventriculostomy in the treatment of triventricular hydrocephalus seen in children with achondroplasia[J]. J Neurosurg, 2005, 103(3 Suppl): 260-265. DOI:10.3171/ped.2005.103.3.0260 |
| [14] |
Kim J, Patel VJ, El Ahmadieh TY, et al. Hydrocephalus in achondroplasia: efficacy of endoscopic third ventriculostomy[J]. J Neurosurg Pediatr, 2022, 29(3): 268-275. DOI:10.3171/2021.9.PEDS21242 |
| [15] |
Akinnusotu O, Isaacs AM, Stone M, et al. Neurosurgical management of cervicomedullary compression, spinal stenosis, and hydrocephalus in pediatric achondroplasia: a systematic review[J]. J Neurosurg Pediatr, 2023, 32(5): 597-606. DOI:10.3171/2023.6.PEDS23162 |
| [16] |
Lundar T, Bakke SJ, Nornes H. Hydrocephalus in an achondroplastic child treated by venous decompression at the jugular foramen.Case report[J]. J Neurosurg, 1990, 73(1): 138-140. DOI:10.3171/jns.1990.73.1.0138 |
| [17] |
Steinbok P, Hall J, Flodmark O. Hydrocephalus in achondroplasia: the possible role of intracranial venous hypertension[J]. J Neurosurg, 1989, 71(1): 42-48. DOI:10.3171/jns.1989.71.1.0042 |
| [18] |
Merker A, Neumeyer L, Hertel NT, et al. Growth in achondroplasia: Development of height, weight, head circumference, and body mass index in a European cohort[J]. Am J Med Genet A, 2018, 176(8): 1723-1734. DOI:10.1002/ajmg.a.38853 |
| [19] |
Tofts L, Das S, Collins F, et al. Growth charts for Australian children with achondroplasia[J]. Am J Med Genet A, 2017, 173(8): 2189-2200. DOI:10.1002/ajmg.a.38312 |
| [20] |
Pauli RM. Achondroplasia: a comprehensive clinical review[J]. Orphanet J Rare Dis, 2019, 14(1): 1. DOI:10.1186/s13023-018-0972-6 |
| [21] |
Junaid M, Ahmed M, Rashid MU. An experience with ventriculoperitoneal shunting at keen's point for hydrocephalus[J]. Pak J Med Sci, 2018, 34(3): 691-695. DOI:10.12669/pjms.343.14081 |
| [22] |
中华医学会神经外科分会小儿神经外科学组. 中国儿童脑积水外科治疗及并发症处理专家共识(2022)[J]. 中华小儿外科杂志, 2023, 44(10): 869-873. Group of Pediatric Neurosurgery, Committee of Neurosurgery, Chinese Medical Association. Chinese expert consensus on surgery and complication management of hydrocephalus in children (2022)[J]. Chin J Pediatr Surg, 2023, 44(10): 869-873. DOI:10.3760/cma.j.cn421158-20220429-00317 |
| [23] |
Dandy WE. Hydrocephalus in chondrodystrophy[J]. Johns Hopkins Hosp Bull, 1921, 32: 5-10. |
| [24] |
Hashmi SS, Gamble C, Hoover-Fong J, et al. Multicenter study of mortality in achondroplasia[J]. Am J Med Genet A, 2018, 176(11): 2359-2364. DOI:10.1002/ajmg.a.40528 |
 2025, Vol. 24
2025, Vol. 24


