2. 苏州大学附属儿童医院骨科, 苏州 215000
2. Department of Orthopedics, Affiliated Children's Hospital, Soochow University, Suzhou 215000, China
颅内动脉瘤在儿童中不常见,发病率为0.5% ~4.6%,其中创伤性颅内动脉瘤(traumatic intracranial aneurysm, TICA)占10% ~39%,明显高于成人[1-4]。TICA一旦破裂,后果严重,病死率达50%[5]。然而,儿童TICA的真实患病率及自然史(自发消退、生长和破裂)目前尚不清楚[6]。本研究回顾性分析苏州大学附属儿童医院收治的2例TICA患儿临床资料,并检索国内外主要数据库中儿童TICA相关文献,对TICA的临床特征及诊治流程进行分析,供临床参考。
资料与方法 一、本院病例收集情况2020年1月至2023年12月苏州大学附属儿童医院共收治TICA患儿2例,收集患儿受伤机制、首发症状、入院时头颅CT检查结果、是否伴有颅骨骨折,以及动脉瘤的部位、大小、形态、治疗方法、并发症及预后情况。本研究已通过苏州大学附属儿童医院伦理委员会审核批准(2024CS185)。患儿家属均知情并签署知情同意书。
二、文献检索方法以颅内动脉瘤、创伤为检索词,在中国知网、万方医学数据库检索;以检索式((((“Child”[Mesh]OR((child[Title/Abstract])OR(Children[Title/Abstract])))OR(“Pediatrics”[Mesh]))OR((“Infant”[Mesh])OR(Infants[Title/Abstract])))AND(((((“Intracranial Aneurysm”[Mesh]) AND (Intracranial Aneurysm[Title/Abstract]))OR(Aneurysms, Intracranial[Title/Abstract]))OR(IntracranialAneurysms[Title/Abstract])) OR (Brain Aneurysm[Title/Abstract]))在PubMed数据库中检索。检索日期均为1993年1月至2023年12月。文献纳入标准:①文献类型包括儿童TICA病例系列研究、病例报告。②文献内容涉及儿童TICA临床特点、治疗、预后及影像学特征等。③发表文献以中文或英文撰写。文献排除标准:文献仅有摘要而无全文;临床资料、影像学资料、预后或随访资料不全。
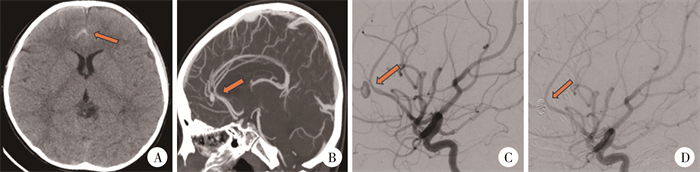
结果 一、本院收治病例情况病例一,男,7岁5个月,初次因交通事故致意识不清2 h入院,入院时格拉斯哥昏迷评分(Glasgow coma scale, GCS)10分,CT提示蛛网膜下腔出血(图 1A),未见骨折,予保守治疗后病情平稳,复查头颅MRI提示无明显异常,予出院。3周后无明显诱因出现头痛,后出现非喷射性呕吐8~9次,呕吐物为胃内容物。病程中无意识丧失、四肢抽搐、肌力障碍、光反射灵敏等现象。入院GCS评分12分。查体:神志清楚,精神萎靡,双瞳孔等大等圆,直径3 mm,对光反射灵敏,颈稍抵抗,肌力、肌张力正常,生理反射存在,病理反射未引出。辅助检查:头部CTA提示大脑前动脉瘤破裂出血(图 1B)。完善相关检查后行脑血管造影术加动脉瘤栓塞术(右侧大脑前动脉栓塞,图 1C、1D),术中见动脉瘤大小约2.9 mm×4.4 mm,术后患儿出现嗜睡、颈背部疼痛明显,复查头颅CT提示脑积水,予脑室- 腹腔分流术治疗。术后2个月随访无明显神经系统功能障碍,改良Rankin量表(modified Rankin Scale, mRS)评分为0~1分。目前患儿无明显神经系统功能障碍,mRS评分为0分。
|
图 1 病例一创伤性颅内动脉瘤患儿影像学检查组图 Fig.1 Imaging panels of a child with traumatic intracranial aneurysm 注 A:入院当天CT复查结果;B:伤后1个月CTA见大脑前动脉区动脉瘤;C:DSA下见右侧大脑前动脉A3段动脉瘤;D:介入栓塞获得成功 |
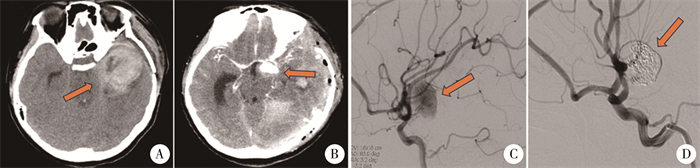
病例二,女,13岁5个月,因意识障碍伴呕吐3小时余入院。患儿3周前因脑肿瘤行手术治疗,术后患者一侧肢体偏瘫,mRS评分为2~3分。3周后突发意识障碍伴呕吐,入院GCS评分9分,急查头部CT提示左侧颞叶占位手术后、颅内多发出血灶(图 2A),行颅内血肿清除术加错位骨瓣成形术,术后恢复良好。术后15 d再次突发头痛、呕吐、意识障碍,GCS评分5分,头颅CTA提示左侧大脑中动脉假性动脉瘤(图 2A),予脑血管造影术加经导管颅内动脉瘤栓塞术、颅内血肿清除术(图 2C、2D),术中见假性动脉瘤约3 cm×4 cm,出院时一侧肢体偏瘫,mRS评分为2~3分。目前患儿仍然存在一侧肢体偏瘫,mRS评分为2~3分。
|
图 2 病例2创伤性颅内动脉瘤影像学检查组图 Fig.2 Imaging panels of another child with traumatic intracranial aneurysm 注 A:急诊入院时CT检查结果;B:CTA见左侧大脑中动脉假性动脉瘤;C:DSA下见左侧颈内动脉末端动脉瘤;D:介入栓塞获得成功 |
共纳入48篇文献(表 1)报道69例病例,患儿年龄(10.4±5.5)岁(0~17岁),男41例、女26例。最常见致病原因为交通事故(23/69,33.3%),其次为医源性损害(12/69,17.4%)。临床症状以意识障碍(26/69,37.7%)及头痛(16/69,23.2%)最常见。入院时初次头颅CT检查以蛛网膜下腔出血(38/69,55.1%)和颅内出血(27/69,39.1%)为主要表现。动脉瘤破裂比例较高(48/69,69.6%),大多数动脉瘤位于前循环(48/69,69.6%),以囊状为主(52/69,75.4%)。治疗方式上,介入治疗是最多见的选择(51/69,73.9%)。大部分治疗患儿预后良好(45/69,65.2%)
讨论就组织学而言,动脉瘤分为假性动脉瘤、真性动脉瘤和混合性创伤性动脉瘤[4, 7]。儿童创伤性动脉瘤以假性动脉瘤为主。创伤性颅内假性动脉瘤主要是由于钝性或穿透性颅脑外伤导致血管壁全层损伤,破裂处经周围组织包裹形成局部血肿,进而纤维机化,形成与血管壁相通的动脉瘤壁,可发生于颅内大血管或远端末梢血管[8]。本研究中文献回顾的69例TICA患儿多数为交通事故和高处坠落伤所致,动脉瘤损伤部位大部分位于前循环,尤以大脑前动脉段及颈内动脉段为多。
因TICA的位置、大小及与周围结构的关系,患儿临床表现各异。有症状的患儿主要表现为创伤后3周内头痛、癫痫发作、恶心、呕吐和意识水平下降等[8]。随着动脉瘤进展,可能导致明显的占位效应,表现为意识丧失或颅神经麻痹[9]。本院收治的病例2动脉瘤较大,发病时即出现明显的占位效应。
儿童创伤性动脉瘤的诊断主要依赖CT血管造影(computed tomography angiography, CTA)及数字减影血管造影(digital subtraction angiography, DSA),CTA因对小于3 mm动脉瘤的灵敏度有限,DSA被认为是目前诊断TICA的金标准[9-11]。有研究者建议,所有穿透性创伤患者在创伤性颅脑损伤(trau- matic brain, injurg, TBI)后2周应行DSA,以排除创
| 表 1 1993年1月至2023年12月期间文献报道的创伤性颅内动脉瘤患儿临床资料 Table 1 Clinical information of TICA children reported in the literature from January 1993 to December 2023 |
|
|
伤性动脉瘤[12-13]。deSouza等[14]建议针对所有出现神经或意识症状突然恶化的TBI患者进行DSA检查。有研究者认为,大多数穿透性TBI患者和严重钝性损伤患者需立即进行DSA检查,如初始结果为阴性,则至少间隔10 d应行第二次成像,以检测晚期形成的TICA[14-16]。Chen等[17]认为,尽管CTA的准确性低于DSA,但其耗时更少、成本更低,在儿童中可以无需麻醉或镇静进行,且可以纳入多发创伤患者的全身扫描进行筛查,因此对于低风险创伤性动脉瘤患者,无需使用DSA检查。综合既往文献,笔者认为DSA的选择应依据患儿创伤性动脉瘤风险程度适宜选择,一方面,儿童创伤性动脉瘤整体发病率相对不高,且危险因素相对集中;另一方面,DSA有创且价格昂贵,容易给患儿带来额外的经济负担。需行DSA检查的因素包括:①颌面部骨折、岩骨骨折和低格拉斯哥昏迷评分(GCS ≤ 6分)[18];②常规CT检查显示基底脑池或纵裂的蛛网膜下腔出血(subarachnoid hemorrhage, SAH)[9, 19];③症状突然继发性恶化[6];④穿透性创伤。笔者收治的2例患儿中,第1例初始CT检查显示存在大脑纵裂蛛网膜下腔出血,虽然患儿初期症状并不严重,但此时可能已出现血管损伤。第2例患儿神经症状突然加重,提示可能发生了动脉瘤破裂。
外科手术治疗效果相对彻底,复发率低,治疗费用相对较低。但对于部分创伤性动脉瘤,瘤颈相对薄弱,术中瘤颈撕脱,动脉瘤破裂出血的风险较高,手术夹闭具有一定挑战性[1]。血管内治疗目前已成为TICA的主流治疗方法,在文献回顾的69例患儿中,51例采取了介入治疗,包括栓塞、支架、覆膜支架以及近年来逐渐流行的血流导向技术,其中支架和覆膜支架在青少年和学龄儿童中的应用更为广泛,但对于婴幼儿,仍倾向于采取较传统的栓塞方法。
综上所述,儿童创伤性动脉瘤发病率较低,临床症状不典型,需结合患儿病史及辅助检查进行综合判断,以减少漏诊和降低误诊率。当然,这一发现是基于少数回顾性病例系列研究和个别病例报告,考虑到儿科患者的预期寿命较长,有必要进一步进行多中心、长期前瞻性研究,以探讨更合适的治疗方案。
利益冲突 所有作者均声明不存在利益冲突
作者贡献声明 孙景轩负责文献检索,杨天权负责论文设计,张荣庭,杨瑜豪负责数据收集,刘雨辰,杨海玲负责研究结果分析与讨论,孙景轩负责论文撰写;王杭州负责全文知识性内容的审读与修正
| [1] |
Livshits IM, Berdinov BF, Musa G, et al. Traumatic intracranial aneurysms (TICA) in children: a description of two clinical cases of successful treatment and review of literature[J]. Childs Nerv Syst, 2022, 38(11): 2063-2070. DOI:10.1007/s00381-022-05647-9 |
| [2] |
吴水华, 陈朝晖, 范双石, 等. 显微手术治疗2月龄婴儿颅内巨大动脉瘤1例并文献复习[J]. 临床小儿外科杂志, 2020, 19(6): 523-527. Wu SH, Chen ZH, Fan SS, et al. Microsurgery of infantile intracranial aneurysm in a 2-month-old child with a literature review[J]. J Clin Ped Sur, 2020, 19(6): 523-527. DOI:10.3969/j.issn.1671-6353.2020.06.012 |
| [3] |
李方成, 李军亮. 小儿脑血管疾病的诊断要点及外科治疗理念[J]. 临床小儿外科杂志, 2019, 18(9): 713-718. Li FC, Li JL. Essentials and concepts in the diagnosis and treatment of cerebrovascular diseases in children[J]. J Clin Ped Sur, 2019, 18(9): 713-718. DOI:10.3969/j.issn.1671-6353.2019.09.001 |
| [4] |
Eliava SS, Yakovlev SB, Pilipenko YV, et al. Unruptured asymptomatic brain aneurysms: modern approaches to the choice of surgical method and treatment outcomes[J]. Zh Vopr Neirokhir Im N N Burdenko, 2021, 85(6): 6-13. DOI:10.17116/neiro2021850616 |
| [5] |
Watridge CB, Muhlbauer MS, Lowery RD. Traumatic carotid artery dissection: diagnosis and treatment[J]. J Neurosurg, 1989, 71(6): 854-857. DOI:10.3171/jns.1989.71.6.0854 |
| [6] |
Dujardin CE, Cloft H, Wijdicks EFM. Brushing against the tentorium: traumatic pseudoaneurysm of the posterior cerebral artery[J]. Neurocrit Care, 2020, 33(2): 607-609. DOI:10.1007/s12028-019-00877-3 |
| [7] |
Larson PS, Reisner A, Morassutti DJ, et al. Traumatic intracranial aneurysms[J]. Neurosurg Focus, 2000, 8(1): e4. DOI:10.3171/foc.2000.8.1.1829 |
| [8] |
Holmes B, Harbaugh RE. Traumatic intracranial aneurysms: a contemporary review[J]. J Trauma, 1993, 35(6): 855-860. DOI:10.1097/00005373-199312000-00009 |
| [9] |
Hejrati N, Ebel F, Guzman R, et al. Posttraumatic cerebrovascular injuries in children.A systematic review[J]. Childs Nerv Syst, 2020, 36(2): 251-262. DOI:10.1007/s00381-019-04482-9 |
| [10] |
Cohen JE, Gomori JM, Segal R, et al. Results of endovascular treatment of traumatic intracranial aneurysms[J]. Neurosurgery, 2008, 63(3): 476-486. DOI:10.1227/01.NEU.0000324995.57376.79 |
| [11] |
Zheng YT, Lu Z, Shen JG, et al. Intracranial pseudoaneurysms: evaluation and management[J]. Front Neurol, 2020, 11: 582. DOI:10.3389/fneur.2020.00582 |
| [12] |
Kieck CF, de Villiers JC. Vascular lesions due to transcranial stab wounds[J]. J Neurosurg, 1984, 60(1): 42-46. DOI:10.3171/jns.1984.60.1.0042 |
| [13] |
Kumar M, Kitchen ND. Infective and traumatic aneurysms[J]. Neurosurg Clin N Am, 1998, 9(3): 577-586. DOI:10.1016/S1042-3680(18)30253-5 |
| [14] |
deSouza RM, Shah M, Koumellis P, et al. Subarachnoid haemorrhage secondary to traumatic intracranial aneurysm of the posterior cerebral circulation: case series and literature review[J]. Acta Neurochir (Wien), 2016, 158(9): 1731-1740. DOI:10.1007/s00701-016-2865-6 |
| [15] |
Bell RS, Vo AH, Roberts R, et al. Wartime traumatic aneurysms: acute presentation, diagnosis, and multimodal treatment of 64 craniocervical arterial injuries[J]. Neurosurgery, 2010, 66(1): 66-79. DOI:10.1227/01.NEU.0000361285.50218.A8 |
| [16] |
Aarabi B. Management of traumatic aneurysms caused by high-velocity missile head wounds[J]. Neurosurg Clin N Am, 1995, 6(4): 775-797. |
| [17] |
Chen XD, Liu Y, Tong HZ, et al. Meta-analysis of computed tomography angiography versus magnetic resonance angiography for intracranial aneurysm[J]. Medicine (Baltimore), 2018, 97(20): e10771. DOI:10.1097/MD.0000000000010771 |
| [18] |
Miller PR, Fabian TC, Croce MA, et al. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes[J]. Ann Surg, 2002, 236(3): 386-395. DOI:10.1097/01.SLA.0000027174.01008.A0 |
| [19] |
Adepoju A, Adamo MA. Posttraumatic complications in pediatric skull fracture: dural sinus thrombosis, arterial dissection, and cerebrospinal fluid leakage[J]. J Neurosurg Pediatr, 2017, 20(6): 598-603. DOI:10.3171/2017.6.PEDS16702 |
 2025, Vol. 24
2025, Vol. 24


