先天性巨结肠(Hirschsprung disease, HD)是常见的先天性消化道疾病之一,多于新生儿期发病,先天性巨结肠相关性小肠结肠炎(Hirschsprung-associated enterocolitis, HAEC)是HD致死的主要影响因素[1-3]。新生儿HD行根治手术难度大,大多先予保守治疗改善症状后再行择期手术,但部分病例狭窄段挛缩严重、病变肠管较长,扩肛、回流灌肠不能有效控制HAEC的反复发生,导致部分喂养困难、营养不良的患儿不得不先实施肠造瘘手术。为减轻患儿多次手术的痛苦,缩短治疗周期,减少费用,本研究对HD患儿进行了长期留置肛管的技术创新,现探讨其安全性和有效性。
资料与方法 一、研究对象回顾性分析江西省儿童医院新生儿外科2019年1月至2023年1月收治的80例HD患儿临床资料。病例纳入标准:①根据病史、体格检查、钡剂灌肠及直肠黏膜抽吸活检病理结果诊断为HD,包括病变累及乙状结肠远端的常见型以及病变累及乙状结肠中近端、降结肠甚至横结肠的长段型;②于本院行巨结肠根治手术,能定期复诊接受随访。排除标准:①合并新生儿坏死性小肠结肠炎、先天性肠旋转不良、神经缺陷、Down综合征等其他先天畸形;②确诊HD后因肠坏死、肠穿孔、感染中毒性休克而行急诊肠造瘘术;③失访。本研究经江西省儿童医院伦理委员会审核批准(JXSETYY — YXKY — 20220296),患儿家属均知情同意。
二、研究方法按照术前保守治疗期辅助通便方式的不同,分为研究组(长期留置肛管)和对照组(行灌肠、扩肛)。根据HD分型,研究组分为常见型组(A组,n=21)和长段型组(C组,n=11),对照组亦分为常见型组(B组,n=33)和长段型组(D组,n=15)。将四个亚组配为两对(A组&B组/C组&D组),比较各组性别、出生体重、首次就诊日龄、行根治术时日龄、手术方式、HAEC发生率、肠造瘘率、行根治术时体重、手术时间、切除病变肠管长度、术后标本扩张段最大直径、病理标本肠壁炎症、术后并发症、住院时间及住院费用。
三、操作方法选取20~24号乳胶双腔导尿管用作肛管,根据患儿体重予以不同型号的肛管留置(3 kg以下选用20号,3~4 kg选用22号,4 kg以上选用24号),操作均在患儿清醒状态下进行。
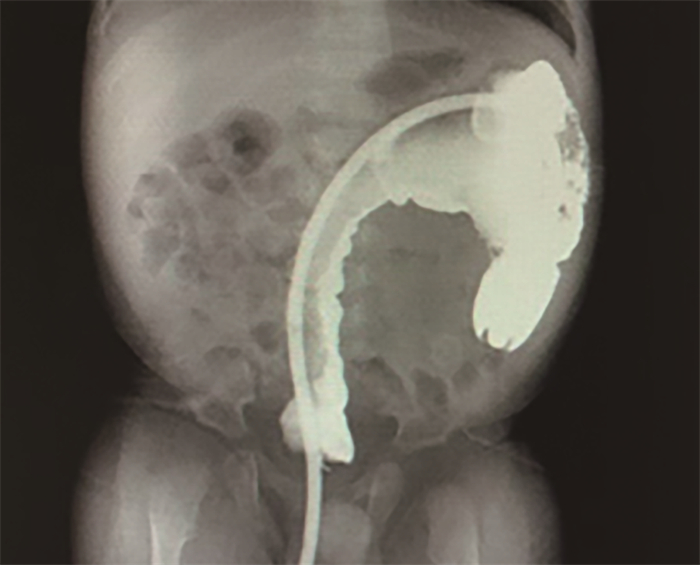
常见型HD可将肛管充分润滑,缓慢将其插入肛门,轻轻旋转插入,依据置管前大肠造影判断导管进入长度(15~20 cm),肛管过狭窄段3 cm后注入10 mL生理盐水球囊固定,于肛门外用蝶形胶布固定于臀部,外接引流袋(图 1)。长段型HD可在胃肠机造影室辅助下放置肛管,充分润滑后缓慢插入肛门,通过腹部触诊避免肛管在肠腔内折角打卷,忌暴力,逐步置入达到狭窄段长度后即刻注入造影剂明确肛管位置,并排除肠穿孔(图 2)。肛管过狭窄段3 cm后注入10 mL生理盐水球囊固定,接引流袋外固定。每日用温生理盐水冲管2次,保持肛管通畅,防止堵管。如堵管可经肛管予以灌肠疏通,无法疏通可自行更换肛管;如肛门口肛管周围有大便排出,可轻柔扶持肛管防止脱出,清水清洗肛周粪便及管壁,烘干后胶布固定;如肛管脱出,可予以缓慢送回,再次胶布固定,若完全脱出则重新置管。

|
图 1 使用留置肛管治疗先天性巨结肠相关小肠结肠炎的患儿外观 Fig.1 Appearance of a child treated with an indwelling anal tube for congenital megacolon-associated enterocolitis |
|
图 2 先天性巨结肠在造影机辅助下留置肛管情况 Fig.2 Retained rectal tube in Hirschsprung disease under fluoroscopy guidance |
分别于术后1、3、6、12、24、36个月对患儿进行复查,观察术后并发症的发生情况,包括肠梗阻、HAEC及吻合口狭窄。
五、统计学处理采用SPSS 27.0进行统计学分析。服从或近似服从正态分布的定量数据以x±s表示,采用两独立样本t检验进行组间比较。无序分类变量用例(%)表示,采用χ2检验或Fisher精确概率法进行组间比较。P < 0.05为差异具有统计学意义。
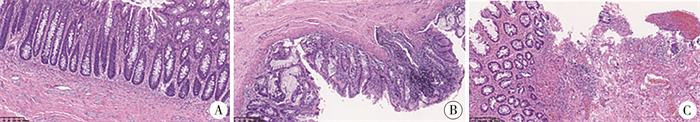
结果研究组与对照组首次就诊日龄、出生体重、根治术日龄、性别、手术方式差异无统计学意义(P>0.05)。A、B两组根治术时体重、造瘘发生率、手术持续时间、切除病变肠管长度、病理标本肠壁炎症发生率、术后并发症、住院天数、住院费用差异无统计学意义(P>0.05)。C、D两组根治术时体重、手术时间、切除病变肠管长度差异无统计学意义(P>0.05)。A、B两组HAEC发生率、结肠扩张段最大直径差异有统计学意义(P<0.05),C、D两组HAEC发生率、造瘘发生率、扩张段最大直径、病理标本肠壁炎症(图 3)发生率、术后并发症、住院天数、住院费用差异有统计学意义(P < 0.05)。见表 1、表 2。
|
图 3 先天性巨结肠术后病理标本 Fig.3 Observation of inflammatory conditions in intestinal wall of Hirschsprung disease postoperative pathological specimen via HE staining 注 A: 正常黏膜;B: 黏膜炎症细胞浸润,隐窝炎;C: 黏膜层可见较多炎症细胞浸润,溃疡形成(HE染色,×100) |
| 表 1 A组、B组HD患儿临床资料比较 Table 1 Comparison of basic information between Group A and Group B HD patients |
|
|
| 表 2 C组、D组HD患儿临床资料比较 Table 2 Comparison of basic information between Group C and Group D HD patients |
|
|
HD患儿根治手术的时机是影响其预后的重要因素。Kastenberg等[4]研究表明,HD新生儿延迟手术时间有利于肛管和括约肌的发育,可降低术后HAEC和大便失禁的风险。Westfal等[5]研究发现在2月龄前手术,术后出现污粪、吻合口狭窄、吻合口瘘的概率较高。等待手术的保守期治疗原则是辅助排气排便,预防HAEC的发生,这对低体重的新生儿、小婴儿尤其重要。灌肠、扩肛等手段在大部分常见型HD中可以取得良好效果,能够达到合适的手术条件。但仍有部分长段型和反复发生HAEC的常见型HD使用这些常规方法效果欠佳,原因多为灌肠管置入长度不够、灌肠液不足或未充分引流,导致患儿在保守期出现贫血、营养不良甚至巨结肠危象,最终不得不接受肠造瘘术[6]。
国内外学者均报道长段型HD术前放置肛管可预防HAEC、避免肠造瘘,但存在病例较少、肛管留置时间短、基层医院难以开展小婴儿肠镜等问题,且暂无常见型HD中留置肛管的报告[7-9]。本研究结果显示,术前HAEC发生率明显降低、结肠扩张段直径明显减小。虽然我们建议患儿留置肛管24 h,但有部分常见型HD患儿家属因“见症状控制良好、忌讳孩子生病为他人所知、肛管材料缺失”等主观或客观因素,自行拔管或脱管后暂不会再插管,待腹胀加重或其他原因解除后再行留置肛管,导致依从度不够。在常见型HD中,留置肛管操作简便、无明显并发症,具有临床治疗优势,可以增加手术安全性,尤其是对常规手段症状控制不佳、HAEC反复发作的病例,但有待后续进一步验证。本研究长段型HD患儿中,研究组术后并发症发生率、结肠扩张直径和肠壁炎症率明显降低,这都是术前肠炎完全缓解、结肠功能受损减少的表现,良好的术前管理、顺利的自然康复也可减少患儿因并发症或分期手术而导致的住院费用和住院时间增加。值得一提的是,研究组中不论长段型HD还是常见型HD, 结肠的扩张程度虽都明显减轻,但两组切除肠管长度却无显著差异,我们认为这和术者习惯有关,在常见型HD手术中,为取得理想的手术效果,较扩张的肠管也会予以切除,长段型则因肠管吻合张力问题,部分较扩张段亦选择了保留。肛管材质的选取应综合考量,材质粗硬可能损伤肠管,甚至导致肠穿孔;材质细软则难以通过结肠弯曲,容易在肠腔内折角打卷,引流过程中也易发生堵管。本研究采用20~24号乳胶双腔导尿管作为肛管,其头端顺滑可通过结肠弯曲,自带球囊可固定在扩张段,侧孔粗大,方便进行结肠灌洗,置入长度可达40 cm,即使狭窄段达到横结肠亦可满足需求。
本研究的局限性在于每个患儿家庭的肛管留置实际践行情况都存在差异,而保守治疗的效果取决于多种因素,包括对患儿家长的宣教质量、长期持续随访和患儿家长的依从性。因此,未来需要进一步扩大研究样本,积累更多的病例及建立多中心合作,继续积累操作经验,完善操作细节,必要时优化措施,对该技术进行客观评价,为其经验的总结和推广提供更多证据,以便向基层医疗机构推广。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 刘智文负责研究的设计、实施和审阅文稿;成子矜、丁宁负责检索文献、统计数据、数据分析;丁宁起草文稿
| [1] |
Pini Prato A, Rossi V, Avanzini S, et al. Hirschsprung's disease: what about mortality?[J]. Pediatr Surg Int, 2011, 27(5): 473-478. DOI:10.1007/s00383-010-2848-2 |
| [2] |
Gosain A, Frykman PK, Cowles RA, et al. Guidelines for the diagnosis and management of Hirschsprung-associated enterocolitis[J]. Pediatr Surg Int, 2017, 33(5): 517-521. DOI:10.1007/s00383-017-4065-8 |
| [3] |
Elhalaby EA, Teitelbaum DH, Coran AG, et al. Enterocolitis associated with Hirschsprung's disease: a clinical histopathological correlative study[J]. J Pediatr Surg, 1995, 30(7): 1023-1027. DOI:10.1016/0022-3468(95)90334-8 |
| [4] |
Kastenberg ZJ, Taylor MA, Durham MM, et al. Perioperative and long-term functional outcomes of neonatal versus delayed primary endorectal pull-through for children with Hirschsprung disease: a pediatric colorectal and pelvic learning consortium study[J]. J Pediatr Surg, 2021, 56(8): 1465-1469. DOI:10.1016/j.jpedsurg.2021.04.024 |
| [5] |
Westfal ML, Okiemy O, Chung PHY, et al. Optimal timing for Soave primary pull-through in short-segment Hirschsprung disease: a meta-analysis[J]. J Pediatr Surg, 2022, 57(4): 719-725. DOI:10.1016/j.jpedsurg.2021.07.007 |
| [6] |
王吉, 李智. 先天性巨结肠非手术治疗研究进展[J]. 临床小儿外科杂志, 2022, 21(2): 186-190. Wang J, Li Z. Recent advances of non-surgical treatment of Hirschsprung's disease[J]. Journal of Clinical Pediatric Surgery, 2022, 21(2): 186-190. DOI:10.3760/cma.j.cn101785-202104064-016 |
| [7] |
Mochizuki K, Shinkai M, Kitagawa N, et al. Continuous transanal decompression for infants with long-and total-type Hirschsprung's diseases as a bridge to curative surgery: a single-center experience[J]. Surg Case Rep, 2017, 3(1): 42. DOI:10.1186/s40792-017-0318-y |
| [8] |
李萍, 汪健, 黄顺根, 等. 经肛门导管持续引流和间隙灌洗用于新生儿长段型巨结肠的治疗和术前准备[J]. 中国血液流变学杂志, 2010, 20(2): 282-283, 304. Li P, Wang J, Huang SG, et al. Transanal catheter fixation and simple frequent tube washouts in long segment-type Hirschsprung's disease[J]. Chin J Hemorheol, 2010, 20(2): 282-283, 304. DOI:10.3969/j.issn.1009-881X.2010.02.041 |
| [9] |
李颀, 孔赤寰, 张震, 等. 经肠镜放置减压管后腹腔镜一期根治术治疗长段型先天性巨结肠[J]. 中华小儿外科杂志, 2018, 39(12): 889-894. Li Q, Kong CH, Zhang Z, et al. Endoscopic placement of decompression tube for long-segment Hirschsprung's disease[J]. Chin J Pediatr Surg, 2018, 39(12): 889-894. DOI:10.3760/cma.j.issn.0253-3006.2018.12.003 |
 2024, Vol. 23
2024, Vol. 23


