颈动脉海绵窦瘘(carotid-cavernous sinus fistula, CCF)是指颈内动脉海绵窦段或颈外动脉硬脑膜支与海绵窦之间形成异常的动静脉交通,导致与海绵窦之间出现异常分流[1-2]。依据发病病因,临床上将CCF分为创伤性和自发性两种类型,创伤性CCF的发病率高于自发性CCF[3-6]。目前介入栓塞术在CCF尤其儿童CCF治疗中的应用较少。湖南省儿童医院神经外科采取介入栓塞术治疗1例9岁2个月CCF患儿获成功,现结合文献复习,总结儿童CCF的临床特点及治疗经验。
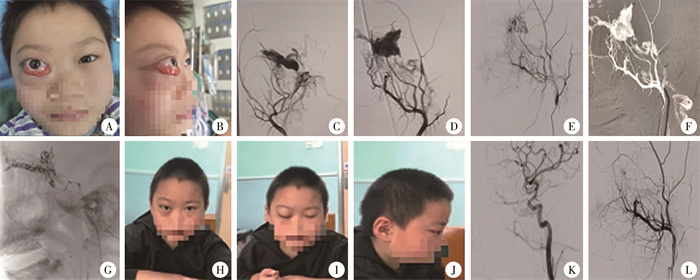
资料与方法 一、病例介绍患儿,男,9岁2个月,因右眼球进行性突出伴红肿18 d入院。头部计算机体层血管成像(CT angiography, CTA)及MRI检查提示右眼眶球后肌锥内血肿,右眼上静脉、右眼眶尖及外侧裂附件血管异常增粗,考虑血管畸形或硬脑膜动静脉瘘。体查:神志清楚,右眼球明显外凸,结膜明显充血外翻,右眼球外展受限(图 1A、1B),双瞳孔正常,双眼视力正常。全脑数字减影血管造影(digital subtraction angiography, DSA)显示:右侧上颌动脉多个分支经硬脑膜直接汇入海绵窦,海绵窦及眼静脉明显扩张(图 1C、1D),考虑右侧颈动脉海绵窦瘘(barrow C型)。
|
图 1 1例9岁2个月颈动脉海绵窦瘘患儿手术前、中、后眼部症状及复查图片 Fig.1 Perioperative ocular symptoms and follow-up images of a 110-month-old CCF boy 注 A:术前正位眼部照片;B:术前侧位眼部照片;C:经颈外动脉正位造影片;D:经颈外动脉侧位造影片;E:术中经微导管导丝路径图进入责任血管;F:弹簧圈放置后侧位显影;G:栓塞后颈外动脉侧位造影;H:术后右眼球正位;I:术后闭眼;J:术后右眼球侧位;K:术后右侧颈内动脉造影侧位片;L:术后右侧颈外动脉造影侧位片 |
术中分别穿刺右侧股静脉及股动脉,行右侧颈外动脉及右侧颈内静脉造影。后经右侧颈内静脉建立血管路径图,在路径图引导下静脉导管进入微导管及微导丝,经岩上窦、海绵窦至右侧眼静脉(图 1E),予弹簧圈栓塞眼静脉后退入海绵窦,用弹簧圈栓塞海绵窦。再次造影提示右侧眼静脉无明显显影(图 1F),海绵窦内少许显影。经动脉血管鞘上微导管及微导丝至右侧上颌动脉一粗大分支,微导管造影提示该分支仍有少许血管汇入海绵窦,将微导管置入动静脉瘘口处,注射栓塞剂,见海绵窦内残余空间被栓塞剂填满,再次行颈外动脉正侧位造影,见海绵窦及眼静脉无明显显影(图 1G)。
二、文献检索方法检索1980—2022年PubMed、Embase数据库中相关外文文献,检索词为“carotid-cavernous sinus fistula in children;embolization operation”;万方医学网、中国知网及中国生物医学文献服务系统中相关中文文献,检索词为“儿童颈动脉海绵窦瘘、介入栓塞手术”。文献纳入标准:①年龄<18岁;②确诊为自发性CCF或创伤性CCF;③治疗方式为介入栓塞术。排除标准:①文献数据不全、资料不齐;②同一数据来源文献;③年龄>18岁;④非介入栓塞治疗。
结果本例患儿出院时眼球活动及右眼突出症状好转。术后1年复查右眼突出红肿消失,(图 1H、1I、1J),复查脑血管造影提示右侧颈动脉海绵窦瘘无明显显影(如图 1K、1L)。根据患儿眼球症状及影像学表现,确定颈动脉海绵窦瘘已治愈。
本研究符合纳入和排除标准文献共6篇(表 1)[7-12],报道病例6例,年龄1个月21天至9岁2个月,临床症状均以眼部症状(如突眼、眼球活动障碍、上睑下垂等)为主,创伤性CCF 5例、自发性CCF 2例,均采用介入栓塞治疗。1例死亡,5例存活;5例存活患儿于1~12个月随访过程中,突眼症状均消失,眼球运动功能恢复正常。
| 表 1 儿童颈动脉海绵窦瘘介入栓塞术治疗相关文献报道情况 Table 1 Literature reports on interventional embolization treatment for pediatric CCF |
|
|
CCF分为自发性和创伤性两种。自发性CCF是由于激素、遗传或感染等因素造成颈动脉与海绵窦之间的异常分流[5-6]。创伤性CCF是由于头面部外伤导致鞍区骨折且鞍旁骨质凹凸不平、厚薄不一,继而导致颈动脉或其分支破裂,与海绵窦之间形成瘘道,是颅脑外伤的罕见并发症[13-14]。CCF临床分为4型[15]:①A型:多属于外伤性,瘘口常单一,盗血量大,瘘口多位于海绵窦的水平段和后升段;②B型:多属于自发性,为颈内动脉脑膜支海绵窦瘘,血流瘘口较多;③C型:颈外动脉脑膜支海绵窦瘘,具有瘘口小、分支多、供血动脉细小的特点;④D型:颈外动脉脑膜支海绵窦瘘,有多个漏口,低血流,瘘口小,分支多,供血动脉细小。本例患儿无外伤病史,为罕见的自发性CCF,且在完善DSA后可见颈外动脉的多个脑膜支供血,流量较小,符合Barrow C型,文献报道的6例中也只有1例自发性CCF,发病率较低。
目前对于儿童CCF的常用诊断方法有以下几种:①CTA可以获得初步的病变筛查,可以在无创情况下显示CCF的瘘口及相关引流静脉,但对于瘘口小、流量小的情况,以及存在骨质干扰,部分病情可能不能被发现; ②MRA:对于软组织的分辨率较高,根据三维血管重建能够清晰分辨颈内动脉及海绵窦的情况,且磁共振没有辐射,对于儿童而言是首选,但由于细小瘘口的分辨率原因及周围骨质所致伪影,对手术不能起明确指导作用;③DSA是诊断儿童CCF的金标准,能够全方位展现瘘口的部位、大小及周围血管之间的关系[16]。CCF患儿的临床症状是由于异常分流致海绵窦内压力升高所造成,表现为搏动性突眼、颅内连续性吹风样杂音、眼球表面血管怒张、眼外肌麻痹、视力下降、头痛、鼻出血[17-18]。往往此类患儿首诊于眼科或耳鼻喉科,本例患儿曾在眼科就诊,后完善DSA后明确诊断为CCF,并经讨论后决定采用介入栓塞术进行治疗。
目前儿童CCF有以下治疗方案:①单侧颈内动脉结扎术:此术式对于成人会造成不可逆的脑梗死甚至出现死亡,对于1岁内的婴幼儿可能有效,但暂无文献叙述。②开颅寻找瘘口并切除:由于此方法损伤较大,且术中对于止血的风险较大,目前也逐渐摒弃。③血管内介入栓塞术:介入栓塞术是一种新的诊断治疗技术,应用于成人较多,但随着现代医学技术的快速发展,这种技术越来越被广泛应用于儿童[19-20]。在检索的相关文献及本例患儿中,6例治愈,1例死亡。凌峻等[12]的报道中提及1例外伤性颅内动脉瘤伴双侧颈内动脉海绵窦瘘儿童经介入栓塞治疗后,出现大面积脑梗死,形成脑疝而死亡。由于该例同时合并颈内动脉假性动脉瘤,考虑在栓塞右侧动脉瘤时导致颈内动脉狭窄,继而出现大面积脑梗死,死亡原因可能与此有关。
不同分型的CCF采用介入栓塞治疗也有不同的路径及材料,目前最常用的介入治疗有以下方式:①可脱式球囊栓塞:此方式对于高流量的单个瘘口效果较好,且治愈率较高;②单纯使用弹簧圈栓塞:此方式风险高,瘘口可能不能完全堵塞,复发率较高,目前使用较少;③弹簧圈联合Onyx胶栓塞:对于瘘口较多且较小的CCF,此种方式较好,先填塞弹簧圈降低血流,随后使用Onyx胶继续封堵,能降低单纯使用Onyx胶所致的误栓塞静脉风险;④覆膜支架置入:此方式能够保证颈内动脉的完整性,治疗CCF较为适合,无论是多个瘘口或单个瘘口流量大,均能使用覆膜支架。但目前临床上对于儿童CCF使用较少,其远期疗效还存在疑问。本例患儿DSA检查可见颈外动脉脑膜支与海绵窦存在多个瘘口,且瘘口细小,供血动脉细小,属于Barrow C型,单纯经动脉途径难以完成栓塞,故予经静脉途径微弹簧圈联合Onyx胶栓塞。介入栓塞治疗CCF的目的是封闭颈内动脉或颈外动脉分支与海绵窦之间瘘口,恢复颈内动脉的正常解剖结构及海绵窦的正常静脉引流,从而改善患儿搏动性突眼、头痛等相关症状,患儿经介入栓塞治疗后症状均消失。
综上所述,儿童CCF的治疗宗旨是既处理瘘口又保证载瘘动脉的通畅,为了使CCF治疗达到良好的效果,需依靠相关CTA、MRA、DSA综合评估瘘口大小、数量、流量、载瘘动脉及引流静脉等情况,从而选择最优介入栓塞入路。介入栓塞治疗创伤小、效果满意、并发症少,是目前CCF的最佳治疗方案,但其在儿童中应用较少,将其应用于儿童CCF的救治还需要更多临床实践来评价。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 文献检索:张津维;论文设计:张津维;数据收集:张津维、陈朝晖、伍添、苏君;研究结果分析与讨论:张津维、陈朝晖、伍添、苏君、吴水华;论文撰写:张津维;全文知识性内容的审读与修正:吴水华
| [1] |
王跃飞, 祝源, 孟亮, 等. 复合技术治疗颈内动脉海绵窦段巨大动脉瘤破裂致颈动脉海绵窦瘘一例[J]. 中国脑血管病杂志, 2022, 19(7): 490-493. Wang YF, Zhu Y, Meng L, et al. Compound technology treatment for carotid-cavernous fistula caused by ruptured giant carotid artery aneurysm: a case report[J]. Chin J Cerebrovasc Dis, 2022, 19(7): 490-493. DOI:10.3969/j.issn.1672-5921.2022.07.008 |
| [2] |
罗叶芳, 何为民. 首诊于眼科的颈动脉海绵窦瘘36例临床分析[J]. 临床眼科杂志, 2022, 30(3): 225-229. Luo YF, He WM. Clinical analysis of 36 cases firstly diagnosed in ophthalmology department with carotid cavernous fistula[J]. J Clin Ophthalmol, 2022, 30(3): 225-229. DOI:10.3969/j.issn.1006-8422.2022.03.007 |
| [3] |
金洪泽, 吕中华, 刘伟, 等. 创伤性颈动脉海绵窦瘘合并假性动脉瘤和大脑中动脉闭塞一例[J]. 中华神经外科杂志, 2022, 38(1): 99-100. Jin HZ, Lyu ZH, Liu W, et al. A case of traumatic carotid cavernous sinus fistula combined with pseudoaneurysm and middle cerebral artery occlusion[J]. Chin J Neurosurg, 2022, 38(1): 99-100. DOI:10.3760/cma.j.cn112050-20210401-00159 |
| [4] |
朱灿敏, 张细六, 李强, 等. 以单纯急性视力下降为临床表现的自发性颈内动脉海绵窦瘘一例[J]. 中华全科医师杂志, 2020, 19(8): 741-742. Zhu CM, Zhang XL, Li Q, et al. Spontaneous carotid cavernous fistula with acute visual loss as clinical manifestation in an elderly patient[J]. Chin J Gen Pract, 2020, 19(8): 741-742. DOI:10.3760/cma.j.cn114798-20191126-00851 |
| [5] |
夭志刚, 周念, 严兵, 等. 介入栓塞联合开放手术治疗外伤后儿童肾恶性横纹肌样瘤破裂1例[J]. 临床小儿外科杂志, 2022, 21(7): 692-694. DOI: 10.3760/cma.j.cn101785-202002060-019. Yao ZG, Zhou N, Yan B, et al. Interventional embolization plus open surgery in the treatment of traumatic rupture of malignant rhabdoid tumor of kidney in children: one case report[J]. DOI: 10.3760/cma.j.cn101785-202002060-019. |
| [6] |
王大宝, 张霞, 胡炜. 介入栓塞术及颅内夹闭术对动脉瘤性蛛网膜下腔出血的影响[J]. 医学研究杂志, 2022, 51(9): 89-92. Wang DB, Zhang X, Hu W. Effects of interventional embolization and intracranial clipping on aneurysmal subarachnoid hemorrhage[J]. J Med Res, 2022, 51(9): 89-92. DOI:10.11969/j.issn.1673-548X.2022.09.019 |
| [7] |
Morais BA, Yamaki VN, Caldas JGMP, et al. Post-traumatic carotid-cavernous fistula in a pediatric patient: a case-based literature review[J]. Childs Nerv Syst, 2018, 34(3): 577-580. DOI:10.1007/s00381-017-3668-7 |
| [8] |
Wajima D, Nakagawa I, Park HS, et al. Successful coil embolization of pediatric carotid cavernous fistula due to ruptured posttraumatic giant internal carotid artery aneurysm[J]. World Neurosurg, 2017, 98: 871.e23-871.e28. DOI:10.1016/j.wneu.2016.11.137 |
| [9] |
Pang D, Kerber C, Biglan AW, et al. External carotid-cavernous fistula in infancy: case report and review of the literature[J]. Neurosurgery, 1981, 8(2): 212-218. DOI:10.1227/00006123-198102000-00011 |
| [10] |
Lin CJ, Luo CB, Chang FC, et al. Combined transarterial, transvenous, and direct puncture of the cavernous sinus to cure a traumatic carotid cavernous fistula[J]. J Clin Neurosci, 2009, 16(12): 1663-1665. DOI:10.1016/j.jocn.2009.02.026 |
| [11] |
Yu JL, Guo YB, Wu ZX, et al. Traumatic arteriovenous fistula between the extracranial middle meningeal artery and the pterygoid plexus: a case report and literature review[J]. Interv Neuroradiol, 2017, 23(1): 90-96. DOI:10.1177/1591019916673584 |
| [12] |
凌峻, 杨少春, 邱传珍, 等. 儿童外伤性颈内动脉动脉瘤伴双侧颈内动脉海绵窦瘘一例并文献复习[J]. 赣南医学院学报, 2018, 38(4): 395-397, 399. Ling J, Yang SC, Qiu CZ, et al. Traumatic intracranial aneurysm and cavernous fistula in children: a report of 1 case and literature review[J]. J Gannan Med Univ, 2018, 38(4): 395-397, 399. DOI:10.3969/j.issn.1001-5779.2018.04.024 |
| [13] |
黄芳, 国宁. 颈内动脉海绵窦瘘50例围术期综合护理[J]. 齐鲁护理杂志, 2014, 20(14): 63-64. Huang F, Guo N. Comprehensive perioperative care for 50 cases of internal carotid artery cavernous sinus fistula[J]. J Qilu Nurs, 2014, 20(14): 63-64. DOI:10.3969/j.issn.1006-7256.2014.14.029 |
| [14] |
李桂林, 王斌, 高俊, 等. 表现为脑神经麻痹的自发性颈内动脉海绵窦瘘1例[J]. 中国微侵袭神经外科杂志, 2008, 13(11): 525. Li GL, Wang B, Gao J, et al. A case of spontaneous cavernous sinus fistula of the internal carotid artery presenting as cerebral nerve palsy[J]. Chin J Minim Invasive Neurosurg, 2008, 13(11): 525. |
| [15] |
Barrow DL, Spector RH, Braun IF, et al. Classification and treatment of spontaneous carotid-cavernous sinus fistulas[J]. J Neurosurg, 1985, 62(2): 248-256. DOI:10.3171/jns.1985.62.2.0248 |
| [16] |
Sumdani H, Aguilar-Salinas P, Avila MJ, et al. Carotid cavernous fistula treatment via flow diversion: a systematic review of the literature[J]. World Neurosurg, 2021, 149: e369-e377. DOI:10.1016/j.wneu.2021.02.015 |
| [17] |
Al Saiegh F, Velagapudi L, Jabbour P. Transvenous Onyx embolization of a type D carotid-cavernous-fistula: operative video[J]. World Neurosurg, 2021, 156: 11. DOI:10.1016/j.wneu.2021.08.107 |
| [18] |
赵旺淼, 葛春燕, 张万增, 等. 动静脉联合入路Onyx胶栓塞创伤性颈动脉海绵窦瘘术中大量鼻出血一例[J]. 中华创伤杂志, 2020, 36(11): 1054-1056. Zhao WM, Ge CY, Zhang WZ, et al. A case of massive rhinorrhage during traumatic carotid cavernous sinus fistula embolisation by combined arteriovenous approach with Onyx gel[J]. Chin J Trauma, 2020, 36(11): 1054-1056. DOI:10.3760/cma.j.cn501098-20200716-00507 |
| [19] |
吴亮, 冯大勤, 周传凯, 等. 双球囊技术在外伤性颈动脉海绵窦瘘治疗中应用探讨[J]. 介入放射学杂志, 2021, 30(9): 866-869. Wu L, Feng DQ, Zhou CK, et al. Discussion on the application of dual-balloon technique in treating traumatic carotid-cavernous fistula[J]. J Interv Radiol, 2021, 30(9): 866-869. DOI:10.3969/j.issn.1008-794X.2021.09.002 |
| [20] |
Gu J, Yan M, Fan WJ, et al. Transvenous embolization of carotid cavernous fistula through inferior petrosal sinus with detachable coils and ethylene vinyl alcohol copolymer[J]. J Vis Exp, 2020(159): e59435. DOI:10.3791/59435 |
 2024, Vol. 23
2024, Vol. 23


