1984年徐达传等[1]首次报道了股前外侧穿支皮瓣的解剖学研究。同年,Song等[2]报道了以旋股外侧动脉降支发出肌间隔穿支的股前外侧皮瓣。之后,股前外侧穿支皮瓣逐渐成为修复重建外科领域的常用皮瓣之一,被称为“万能皮瓣”[3]。股前外侧穿支皮瓣修复皮肤软组织缺损有两种方式,即需要吻合微血管的游离股前外侧穿支皮瓣移植术和无需吻合微血管的带蒂股前外侧穿支皮瓣移植术。湖南省儿童医院骨科于2020年采用带蒂股前外侧穿支皮瓣移植术修复臀部硬纤维瘤切除术后皮肤软组织缺损患儿1例,现结合文献复习报道如下。
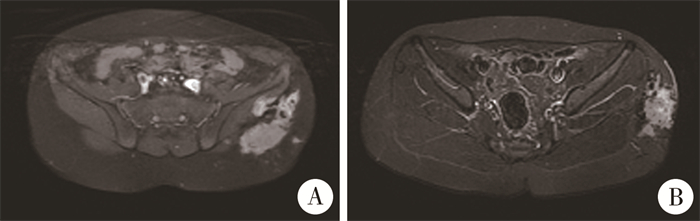
病例资料 一、本例患儿临床资料患儿男,9岁,因左臀部疼痛、触及包块就诊。查体:左臀部皮肤色素沉着,扪及大小约18 cm×8 cm质硬包块,边界不清楚,局部有压痛,左髋关节轻度屈髋,内收内旋受限。MRI检查提示:左臀部脂肪层内及邻近臀大肌、臀中肌区见团块状混杂信号肿块影,以等-稍长T1、长T2信号改变为主,其内见更长T1、短T2信号影混杂及流空血管样影,增强扫描呈明显不均匀强化,肿块大小约18 cm×8 cm,厚3~5 cm。见图 1。
|
图 1 9岁男性臀部硬纤维瘤患儿MRI平扫及增强扫描图 Fig.1 Plain and enhanced MRI scans of a 9-year-old male boy with hip fibroma 注 A:横断面见邻近臀大肌、臀中肌区团块状信号肿块影;B:肿块侵及表面皮肤 |
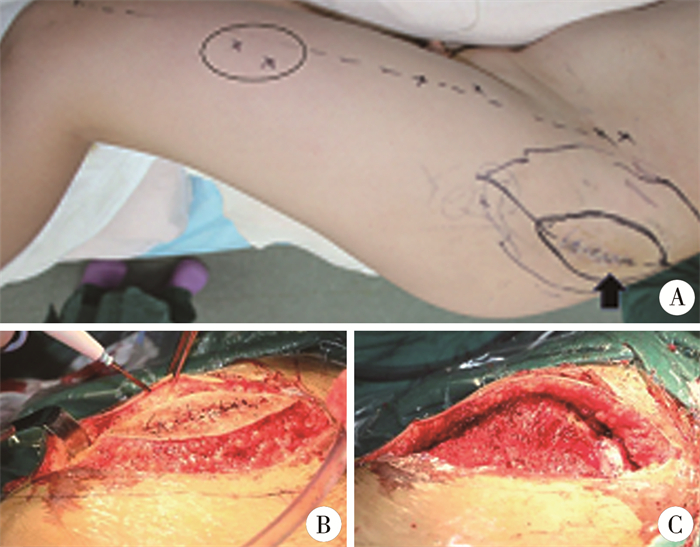
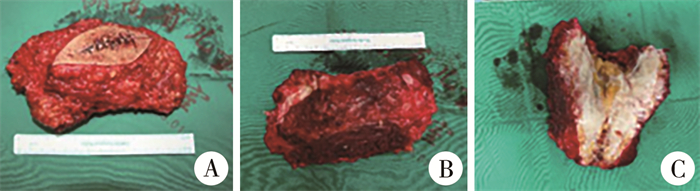
入院后在全身麻醉下行左臀部肿块切开活检术,病理结果提示为臀部硬纤维瘤。明确诊断后行左臀部硬纤维瘤R0切除术,沿髂后上棘至股骨大粗隆连线、左臀部肿瘤侵袭粘连皮肤区域外侧缘2 cm处,取长梭形切口(图 2),见左臀部硬纤维瘤位于髂后上棘至股骨大粗隆连线上,侵袭阔筋膜张肌、部分臀大肌和臀中肌,侵袭臀外侧约3 cm×6 cm大小皮肤;于肿瘤外侧缘2 cm分离并切断肿瘤所侵袭阔筋膜张肌、臀大肌、臀中肌,见肿瘤近端与髂后上棘及相邻髂嵴连接紧密,将连接部位骨膜、软骨切除,再将左侧臀部硬纤维瘤完全切除取出,测量肿块大小约15 cm×8 cm×6 cm(图 3),臀部皮肤缺损区大小约15 cm×6.5 cm(图 2)。
|
图 2 9岁男性臀部硬纤维瘤切除术中照片 Fig.2 Intraoperative views f a 9-year-old boy during a surgical excision of stiff fibrous tumor in buttock 注 A:术前计划切除皮肤范围(黑色实心箭头),于髂前上棘与髌骨外侧连线中点附近,用手提式彩色多普勒探出旋股外侧动脉降支穿支的体表投影(黑色椭圆圈内标记);B:切除侵犯皮肤的臀部硬纤维瘤;C:硬纤维瘤切除后皮肤软组织缺损范围15 cm×6.5 cm |
|
图 3 臀部硬纤维瘤外观及剖面观 Fig.3 Outer and cross-section views of stiff fibroma of buttock 注 A、B:硬纤维瘤及侵犯的皮肤切除外观;C:硬纤维瘤纵行剖开外观 |
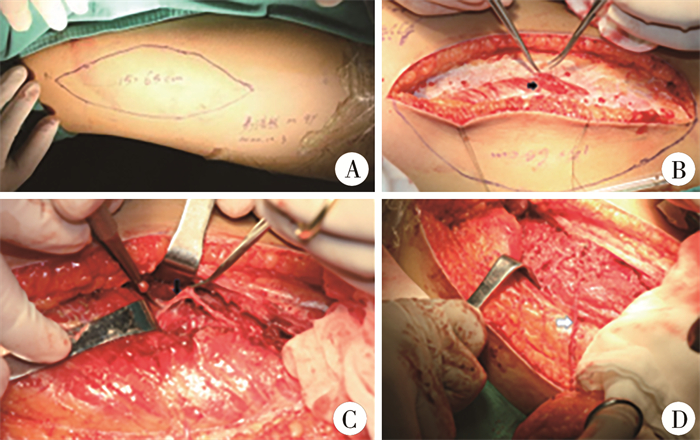
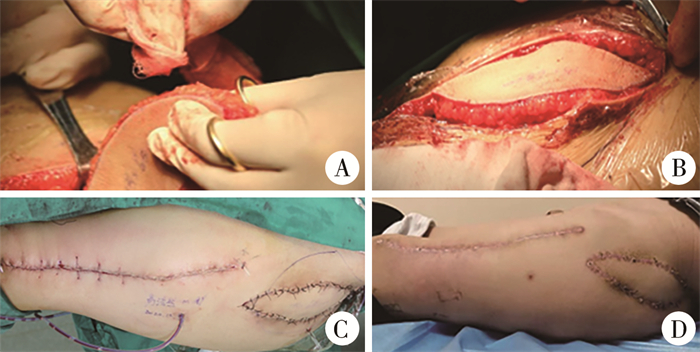
将部分切断臀肌缝合固定于毗邻的髂后上棘,采取带蒂股前外侧穿支皮瓣移植术修复臀外侧皮肤缺损,带蒂股前外侧穿支皮瓣设计见图 4,皮瓣大小约15 cm×6.5 cm。采用逆行四面解剖法游离旋股外侧动脉降支穿支,直至一级源血管,使其有足够长度转位移植至受区缺损部位(图 4)。确认皮瓣血运良好后,将带蒂股前外侧穿支皮瓣经皮下隧道顺行转位移植于臀部皮肤缺损区,缝合供区皮肤(图 5)。
|
图 4 带蒂股前外侧穿支皮瓣的切取 Fig.4 Harvesting pedicled anterolateral femoral perforator flap 注 A:股前外侧皮瓣设计及切取大小(15 cm×6.5 cm);B:深筋膜表面找到穿支血管(黑色实心箭头),并游离;C:采用逆行四面解剖法分离旋股外侧动脉降支穿支血管;D:游离旋股外侧动脉降支穿支血管,足够长度的血管蒂转位至受区缺损部位 |
|
图 5 带蒂股前外侧穿支皮瓣移植术中及随访照片 Fig.5 Intraoperative and follow-up views of pedicled anterolateral perforator thigh flap transplantation 注 A、B:股前外侧穿支皮瓣移植术中转位后皮瓣血运良好;C:受区皮肤缝合及供区直接拉拢缝合,皮瓣血运良好;D:术后随访皮瓣颜色、质地良好 |
患儿术后穿支皮瓣血运良好,均存活,未见血管危象发生,随访24个月,臀部硬纤维瘤无复发,供区愈合良好;无肌疝,受区皮瓣颜色、质地良好,患肢髋、膝关节活动无受限,受区及供区可见瘢痕增生。
二、文献检索方法及结果检索PubMed、万方数据库和中国知网自1970年1月至2022年12月公开发表的文献,中文检索词为“带蒂股前外侧皮瓣”、“臀部软组织缺损”,英文检索词“pedicled anterolateral perforator thigh flap”、“soft tissue defect of hip”。文献纳入标准:带蒂股前外侧穿支皮瓣修复臀部软组织缺损的病例报道或临床研究。文献排除标准:①非中、英文文献,文献报道数据不全,资料不齐;②综述、信件、会议摘要或同一数据来源的文献。
符合纳入与排除标准的文献共2篇(1篇英文文献和1篇中文文献),均为个案报道,共2例。其中Kadota等[4]报道1例涉及会阴、阴囊、腹股沟、大腿内侧、臀部和肛周区域,皮肤软组织缺损大小为36 cm×18 cm,采用3个带蒂皮瓣修复,即双侧带蒂股前外侧穿支皮瓣及腹壁下动脉带蒂穿支皮瓣。皮瓣无张力下转至缺损区,无需植皮即成功覆盖缺损。除腹壁下动脉穿支皮瓣尖端小部分表皮坏死外,未发生其他术后并发症,随访9个月,无髋关节运动障碍发生,重建皮肤无撕脱或溃疡,受区和供区外观满意。李福民等[5]报道1例涉及臀部、股骨大粗隆区,皮肤软组织缺损大小29 cm×20 cm,股骨大粗隆外露10 cm×5 cm,运用带蒂股前外侧穿支皮瓣加部分植皮修复缺损,术后穿支皮瓣未见血管危象,皮瓣全部存活,植皮有小部分坏死,经换药2周后愈合。术后随访18个月,供区愈合良好,无髋关节功能障碍。受区穿支皮瓣的颜色、质地均较好,髋、膝关节功能无受限。
讨论 一、带蒂股前外侧皮瓣的应用自徐达传等[1]首次报道股前外侧皮瓣的解剖研究后,Song等[2]、Kadota等[4]开始关注股前外侧穿支皮瓣的临床应用。股前外侧穿支皮瓣有恒定的穿支血管解剖,切取皮瓣时供区损伤小,切取相对简单,修复范围广,但股前外侧皮瓣穿支血管在解剖上存在一定变异[6]。Song等[2]、Samra等[3]报道时即提出这一点。
带蒂股前外侧穿支皮瓣有许多优点,其有长且相对稳定的穿支血管蒂,可以修复的缺损范围较为广泛。皮瓣的血供来自股深动脉的分支旋股外侧动脉降支。文献报道穿支血管蒂长度多为4~20 cm,也有文献报道1例穿支血管蒂长度为37 cm[7]。由于皮瓣蒂的长度较长,股前外侧皮瓣可带血管蒂顺行转移,移植至下腹部、会阴、腹股沟、臀区和大腿等多个区域,逆行转移可以修复大腿远端、膝部及小腿近端的皮肤软组织缺损,因而具有一定的灵活性[6]。
1999年Kimata等[8]第一个使用顺行带蒂股前外侧穿支皮瓣,其报道的3例带蒂股前外侧穿支皮瓣重建腹部皮肤软组织缺损大小为12 cm×2 cm~18 cm×24 cm,平均随访10.7个月,所有皮瓣完全存活,无一例腹壁疝发生。此后,带蒂股前外侧穿支皮瓣移植修复皮肤软组织缺损的应用越来越多[9]。Sharma等[10]报道了20例腹壁缺损采用带蒂股前外侧穿支皮瓣修复,皮肤软组织平均缺损长度14.2 cm。宋达疆等[11]介绍了18例腹壁肿瘤,经带蒂股前外侧穿支皮瓣或肌皮瓣移植修复后平均随访22.5个月,无一例肿瘤复发或腹壁疝。Acartürk等[12]报道了23例顺行带蒂股前外侧穿支皮瓣修复皮肤软组织缺损,其中位于腹壁(包括腹股沟)10例,坐骨及股骨大粗隆9例,会阴部4例,皮肤软组织缺损范围6 cm×6 cm~30 cm×35 cm,术后皮瓣均存活。Santanelli等[13]报道了5例脑脊膜脊髓膨出、坐骨溃疡病例,采用带股前外侧皮神经的股前外侧穿支皮瓣顺行修复,平均随访26.4个月,无一例发生早期或晚期并发症,因携带皮神经,患儿术后受区皮瓣感觉得到恢复。王丹莹[14]介绍了采用近端带蒂股前外侧穿支皮瓣修复不同部位皮肤软组织缺损83例,缺损大小13 cm×4 cm~30 cm×15 cm,血管蒂长度6~25 cm,平均12.2 cm,术后发生皮瓣远端缺血坏死1例,皮瓣静脉回流不畅2例,均经保守治疗后皮瓣存活,术后血肿1例,采用该皮瓣修复皮肤软组织缺损的手术成功率为95.2%。张启旭等[15]报道了112例股前外侧穿支皮瓣修复缺损,其中带蒂皮瓣顺行转移5例,逆行转移7例,皮瓣整体存活率95.6%,远期随访疗效满意率91%,无供区功能受限。Scaglioni等[16]报道了1例双侧带蒂股前外侧皮瓣及缝匠肌皮瓣修复会阴、阴囊及大腿内侧皮肤软组织缺损,大小27 cm×30 cm。之后Scaglioni等[17]又报道了1例右侧腹股沟区12 cm×18 cm污染软组织缺损且有股血管外露,运用带蒂股前外侧肌皮瓣修复(带皮神经)。Spyropoulou等[18]报道了10例带蒂股前外侧穿支皮瓣修复会阴、阴囊和阴道缺损,血管蒂长度为10~12 cm,所有病例供区无并发症。任洪军等[19]报道对软组织肿瘤切除后皮肤软组织缺损,采用股前外侧穿支皮瓣游离移植或带蒂转移的对比研究,指出带蒂皮瓣手术时间少于游离皮瓣手术时间,两组皮瓣存活率及并发症相当。Wang等[20]报道了21例带蒂股前外侧穿支肌皮瓣重建股骨粗隆压疮,皮瓣长8~21 cm,宽5~11 cm,平均随访13.9个月,无一例发生血管危象,皮瓣均存活,无严重并发症。申练兵等[21]报道了带蒂股前外侧穿支皮瓣顺行修复股骨粗隆部褥疮4例,逆行修复膝关节软组织缺损9例,皮瓣均存活,1例皮瓣大部分存活,随访12~36个月,皮瓣质地优良,外观及功能满意。Jang等[22]介绍的因腹壁复发性硬纤维瘤行根治性切除,致全层腹壁缺损,范围25 cm×20 cm,采用带血管蒂股前外侧穿支皮瓣移植修复腹部皮肤软组织缺损。除上述可能性外,带蒂股前外侧皮瓣有最小的供区发病率,如果皮瓣大小不超过21 cm×9 cm,供区可以直接闭合[23]。Kadota等[4]和李福民等[5]分别报道了1例带蒂股前外侧穿支皮瓣修复涉及臀部缺损病例。
带蒂股前外侧穿支皮瓣还可以逆行转移修复膝关节周围大面积皮肤软组织缺损。Wong等[24]报道了6例带蒂股前外侧穿支皮瓣逆行修复膝关节缺损。另外,申练兵等[21]、张启旭等[15]也有报道逆行转移修复膝关节周围缺损。
二、皮肤软组织缺损的治疗进展皮肤是人体最大的器官,是隔离人体内部结构与外界的第一道屏障,皮肤缺损后如果不及时处理或处理不当,可使细菌、病毒等微生物侵入而导致人体感染,严重者可危及生命[25]。传统皮肤软组织修复重建阶梯方案为:外科换药、外科缝合、皮片移植术、皮肤软组织扩张术、皮瓣转移手术[26]。近几十年来,皮肤移植技术的研究和发展主要聚焦于如何以最小的供区修复更大的皮肤缺损,如早期的网状植皮和Meek技术。网状植皮主要利用拉网机将皮片扩张至1∶6~1∶9的比例,而Meek技术则通过切割、拓展将皮片的可移植率扩大到1∶9[27]。移植皮片的一个重要条件是有良好的软组织床,皮片的存活早期主要依赖软组织床渗出的血浆和纤维蛋白,之后则依赖移植皮片内新生血管的长入提供营养。在血管长入过程中,若移植皮片发生移位、皮下血肿,则移植皮片血管化发生障碍,导致皮片坏死[28]。皮肤软组织扩张术是通过皮下植入硅胶扩张器并持续注入生理盐水,在机械力的作用下获取比局部皮肤更大的皮肤过程。该技术首先由Neumann[29]报道,后有研究者改良此方法,这种技术是目前用于皮肤软组织大面积缺损后修复的重要外科技术之一。但目前皮肤软组织扩张术的应用受到一定限制,首先,机械牵张诱导的皮肤再生能力有限,面积一般只有原来的2~3倍,且皮肤扩张后皮瓣有回缩现象,无限扩张导致扩张皮肤变薄、缺血,修复效果不理想。其次,皮肤感染、扩张组织坏死、溃疡等皮肤扩张后并发症的发生率较高[30]。随着显微外科技术的发展,游离皮瓣或带蒂皮瓣的应用越来越广泛,由于皮瓣可带筋膜、肌肉组织等,是皮肤及皮下组织缺损或有血管神经及骨外露,甚至感染创面的首选修复方法[31]。
本研究中的病例为了保证硬纤维瘤能实现显微边缘R0切除,术中切面穿过未被肿瘤浸润的正常组织面。广泛切除的缺点之一是术后臀部皮肤软组织缺损,且深达骨面,切除后有骨外露,综合考虑后选择带蒂股前外侧穿支皮瓣移植修复臀部硬纤维瘤切除后臀部皮肤软组织缺损。结合文献报道带蒂股前外侧穿支皮瓣术后均未见明显严重并发症,我们认为是一种相对可靠的治疗方式。
综上所述,对于有症状或进展性硬纤维瘤切除后有皮肤软组织缺损、尤其存在血管神经或骨外露的患儿,首选治疗方法是吻合血管的游离皮瓣或带蒂皮瓣移植修复,而带蒂皮瓣相对于游离皮瓣,由于不需要吻合微血管,手术时间短,对于臀部侵犯皮肤有症状的硬纤维瘤,行带蒂股前外侧穿支皮瓣移植修复缺损是一种合适的治疗方法。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 王军、曾凌嵘负责论文设计、论文撰写与修改;伍江雁、谭晓谦负责数据收集、文献检索;梅海波负责全文知识性内容的审读与修正。
| [1] |
徐达传, 钟世镇, 刘牧之, 等. 股前外侧部皮瓣的解剖学一个新的游离皮瓣供区[J]. 中国临床解剖学杂志, 1984, 2(3): 158-160. Xu DC, Zhong SZ, Liu MZ, et al. Anatomy of anterolateral thigh flap as a new free flap donor area[J]. Chin J Clin Anat, 1984, 2(3): 158-160. DOI:10.13418/j.issn.1001-165x.1984.03.012 |
| [2] |
Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery[J]. Br J Plast Surg, 1984, 37(2): 149-159. DOI:10.1016/0007-1226(84)90002-x |
| [3] |
Samra F, Bibbo C, Levin LS, et al. A practical guide to the use of the anterolateral thigh flap[J]. JBJS Essent Surg Tech, 2017, 7(3): e22. DOI:10.2106/JBJS.ST.16.00092 |
| [4] |
Kadota H, Momii K, Hanada M, et al. Simultaneous deep inferior epigastric and bilateral anterolateral thigh perforator flap reconstruction of an extended perineoscrotal defect in Fournier's gangrene: a case report[J]. Microsurgery, 2019, 39(3): 263-266. DOI:10.1002/micr.30409 |
| [5] |
李福民, 张功林, 任恒宽, 等. 股前外侧带蒂皮瓣修复臀和股部大面积软组织缺损一例[J]. 中华显微外科杂志, 2012, 35(2): 118. Li FM, Zhang GL, Ren HK, et al. Use of anterolateral thigh pedicled flap for repairing large soft tissue defect of buttock and thigh: one case report[J]. Chin J Microsurg, 2012, 35(2): 118. DOI:10.3760/cma.j.issn.1001-2036.2012.02.009 |
| [6] |
Gentileschi S, Servillo M, Garganese G, et al. Versatility of pedicled anterolateral thigh flap in gynecologic reconstruction after vulvar cancer extirpative surgery[J]. Microsurgery, 2017, 37(6): 516-524. DOI:10.1002/micr.30077 |
| [7] |
Vijayasekaran A, Gibreel W, Carlsen BT, et al. Maximizing the utility of the pedicled anterolateral thigh flap for locoregional reconstruction: technical pearls and pitfalls[J]. Clin Plast Surg, 2017, 44(2): 371-384. DOI:10.1016/j.cps.2016.12.004 |
| [8] |
Kimata Y, Uchiyama K, Sekido M, et al. Anterolateral thigh flap for abdominal wall reconstruction[J]. Plast Reconstr Surg, 1999, 103(4): 1191-1197. DOI:10.1097/00006534-199904040-00014 |
| [9] |
Neligan PC, Lannon DA. Versatility of the pedicled anterolateral thigh flap[J]. Clin Plast Surg, 2010, 37(4): 677-681. DOI:10.1016/j.cps.2010.07.001 |
| [10] |
Sharma A, Kalra S, Aggarwal M, et al. Abdominal wall reconstruction using pedicled antero lateral thigh flap[J]. World J Plast Surg, 2022, 11(3): 63-71. DOI:10.52547/wjps.11.3.63 |
| [11] |
宋达疆, 李赞, 周晓, 等. 带蒂股前外侧肌皮瓣修复腹壁肿瘤术后全层缺损[J]. 中国修复重建外科杂志, 2019, 33(6): 712-716. Song DJ, Li Z, Zhou X, et al. Application of pedicled anterolateral thigh myocutaneous flap for full-thickness abdominal wall reconstruction after tumor resection[J]. Chinese Journal of Reparative and Reconstructive Surgery, 2019, 33(6): 712-716. DOI:10.7507/1002-1892.201901005 |
| [12] |
Acartürk TO, Bengür FB. Individually tailored approach to reconstruction of complex defects using versatility of the lateral circumflex femoral artery system-based pedicled flaps[J]. J Plast Reconstr Aesthet Surg, 2022, 75(1): 199-209. DOI:10.1016/j.bjps.2021.08.035 |
| [13] |
Santanelli Di Pompeo F, Longo B, Pagnoni M, et al. Sensate anterolateral thigh perforator flap for ischiatic sores reconstruction in meningomyelocele patients[J]. Microsurgery, 2015, 35(4): 279-283. DOI:10.1002/micr.22330 |
| [14] |
王丹莹. 近端蒂股前外侧皮瓣的临床应用研究及CT血管造影预测近端蒂股前外皮瓣血管蒂长度的研究[D]. 北京: 北京协和医学院, 2022. DOI: 10.27648/d.cnki.gzxhu.2022.000176000176. Wang DY. Clinical applications and prediction of length using CT angiography of proximally-based anterolateral thigh flap[D]. Beijing: Peking Union Medical College, 2022. DOI: 10.27648/d.cnki.gzxhu.2022.000176000176. |
| [15] |
张启旭, 乔群, 陈光宇, 等. 股前外侧组织瓣临床应用112例分析[J]. 中国修复重建外科杂志, 2006, 20(5): 540-543. Zhang QX, Qiao Q, Chen GY, et al. Clinical application of anterolateral thigh flap: a report of 112 patients[J]. Chinese Journal of Reparative and Reconstructive Surgery, 2006, 20(5): 540-543. |
| [16] |
Scaglioni MF, Fakin RM, Barth AA, et al. Bilateral pedicle anterolateral thigh (ALT) flap combined with bilateral sartorius muscle flap for reconstruction of extensive perineoscrotal and medial thigh defect because of Fournier's gangrene[J]. Microsurgery, 2017, 37(6): 669-673. DOI:10.1002/micr.30083 |
| [17] |
Scaglioni MF, Franchi A, Giovanoli P. Pedicled chimeric sensitive fasciocutaneous anterolateral thigh (ALT) and vastus lateralis muscle (VLM) flap for groin defect reconstruction: A case report[J]. Microsurgery, 2018, 38(4): 423-426. DOI:10.1002/micr.30157 |
| [18] |
Spyropoulou GA, Jeng SF, Demiri E, et al. Reconstruction of peri-neoscrotal and vaginal defects with pedicled anterolateral thigh flap[J]. Urology, 2013, 82(2): 461-465. DOI:10.1016/j.urology.2013.04.044 |
| [19] |
任洪军, 李斌, 赵占卫. 股前外侧穿支皮瓣修复软组织恶性肿瘤切除术后创面缺损[J]. 实用手外科杂志, 2022, 36(1): 80-83. Ren HJ, Li B, Zhao ZW. Application of pedicled anterolateral thigh perforator flap for treating wound defects after resecting soft tissue malignant tumors[J]. J Pract Hand Surg, 2022, 36(1): 80-83. DOI:10.3969/j.issn.1671-2722.2022.01.023 |
| [20] |
Wang CH, Chen SY, Fu JP, et al. Reconstruction of trochanteric pressure sores with pedicled anterolateral thigh myocutaneous flaps[J]. J Plast Reconstr Aesthet Surg, 2011, 64(5): 671-676. DOI:10.1016/j.bjps.2010.08.042 |
| [21] |
申练兵, 谭俊铭, 王朝阳, 等. 带蒂股前外侧皮瓣的临床应用[J]. 中外医疗, 2010, 29(29): 38-39. Shen LB, Tan JM, Wang CY, et al. Clinical applications of pedicled anterolateral thigh flap[J]. China Foreign Med Treat, 2010, 29(29): 38-39. DOI:10.16662/j.cnki.1674-0742.2010.29.077 |
| [22] |
Jang J, Jeong SH, Han SK, et al. Reconstruction of extensive abdominal wall defect using an eccentric perforator-based pedicled anterolateral thigh flap: a case report[J]. Microsurgery, 2013, 33(6): 482-486. DOI:10.1002/micr.22117 |
| [23] |
Lin CT, Wang CH, Ou KW, et al. Clinical applications of the pedicled anterolateral thigh flap in reconstruction[J]. ANZ J Surg, 2017, 87(6): 499-504. DOI:10.1111/ans.12973 |
| [24] |
Wong CH, Goh T, Tan BK, et al. The anterolateral thigh perforator flap for reconstruction of knee defects[J]. Ann Plast Surg, 2013, 70(3): 337-342. DOI:10.1097/SAP.0b013e318234e8e2 |
| [25] |
Kohlhauser M, Luze H, Nischwitz SP, et al. Historical evolution of skin grafting-a journey through time[J]. Medicina (Kaunas), 2021, 57(4): 348. DOI:10.3390/medicina57040348 |
| [26] |
Arain AR, Cole K, Sullivan C, et al. Tissue expanders with a focus on extremity reconstruction[J]. Expert Rev Med Devices, 2018, 15(2): 145-155. DOI:10.1080/17434440.2018.1426457 |
| [27] |
Pripotnev S, Papp A. Split thickness skin graft meshing ratio indications and common practices[J]. Burns, 2017, 43(8): 1775-1781. DOI:10.1016/j.burns.2017.04.024 |
| [28] |
Cao XL, Hu ZC, Zhang Y, et al. Negative-pressure wound therapy improves take rate of skin graft in irregular, high-mobility areas: a randomized controlled trial[J]. Plast Reconstr Surg, 2022, 150(6): 1341-1349. DOI:10.1097/PRS.0000000000009704 |
| [29] |
Neumann CG. The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear[J]. Plast Reconstr Surg (1946), 1957, 19(2): 124-130. DOI:10.1097/00006534-195702000-00004 |
| [30] |
Karimi H, Latifi NA, Momeni M, et al. Tissue expanders; review of indications, results and outcome during 15 years' experience[J]. Burns, 2019, 45(4): 990-1004. DOI:10.1016/j.burns.2018.11.017 |
| [31] |
Qiao J, Mao HJ, Wen L, et al. Reconstruction of Soft tissue defect with a free vascularized anterolateral thigh flap after resection of Soft tissue sarcoma in extremities[J]. Orthop Surg, 2022, 14(2): 215-220. DOI:10.1111/os.12840 |
 2024, Vol. 23
2024, Vol. 23


