2. 北京大学医学部, 北京 100191;
3. 骨与关节精准医学工程研究中心, 北京 100191;
4. 脊柱疾病研究北京市重点实验室, 北京 100191
2. Department of Orthopedics, Peking University Third Hospital, Beijing 100191, China;
3. Engineering Research Center of Bone & Joint Precision Medicine, Beijing 100191, China;
4. Beijing Key Laboratory of Spinal Disease Research, Beijing 100191, China
寰枢关节旋转固定性脱位(atlanto-axial rotatory dislocation, AARD)属于寰枢关节旋转固定或脱位(atlanto-axial rotatory fixation or dislocation, AARF/D) 的一类,好发于儿童,以头部歪斜、颈部疼痛、颈椎活动受限为主要临床表现,其病因包括口咽或上呼吸道感染、颈部轻微扭伤或撞伤以及头颈部手术[1]。AARF/D均存在寰枕关节反向旋转移位代偿寰枢关节旋转移位的情况[2-3]。早期可表现为寰枕关节松弛和过度旋转,随着病程延长,寰枕关节旋转角度将进一步增大,出现旋转固定;当寰枕关节代偿过度,甚至可能导致寰枕关节脱位(atlanto-occipital dislocation, AOD),发展为枕寰枢关节旋转脱位(occipito-atlanto-axial rotatory dislocation, OAARD)[2-7]。本研究通过分析AARD患儿寰枢以及寰枕的旋转分离角特征,对寰枕关节代偿角度与寰枢关节旋转程度的关系进行验证,并进一步针对AARD患者在不同寰枢关节旋转移位程度下的寰枕关节代偿情况进行定量分析。
资料与方法 一、研究对象本研究为回顾性研究,以2016年6月至2023年6月在北京大学第三医院骨科就诊并接受手术的19例AARD患儿为研究对象,收集患儿术前CT影像、术前诊断、年龄、性别以及病程等临床资料。共纳入19例AARD患儿,男10例、女9例,寰椎相对枢椎向左旋转13例、向右旋转6例,年龄(10.12±0.55)岁,病程2~132个月(中位数7个月)。C1C2、OcC2分别为(24.5±2.9)°和(15.3±1.4)°;OcC1为-1.3(-14.4, 0.9)°。
病例纳入标准:①具有头部歪斜、颈部疼痛、颈椎活动受限中的一个或多个临床表现;②影像学资料确诊寰枢关节旋转固定性脱位;③年龄3~16岁。排除标准:①无术前CT检查影像;②CT检查未覆盖寰枢椎以及颅底区域;③寰枢关节手术史;④其他原因所致的寰枢关节不稳定或脱位,如颅椎区创伤性骨折脱位、感染或肿瘤。本研究经北京大学第三医院伦理委员会审核批准(M2022822),患儿家属均知情同意并签署知情同意书。
二、测量方法 (1) CT测量方法患者平躺于CT台,双肩贴于台面,颈椎呈自然位,行轴位寰枢椎或颈部扫描。
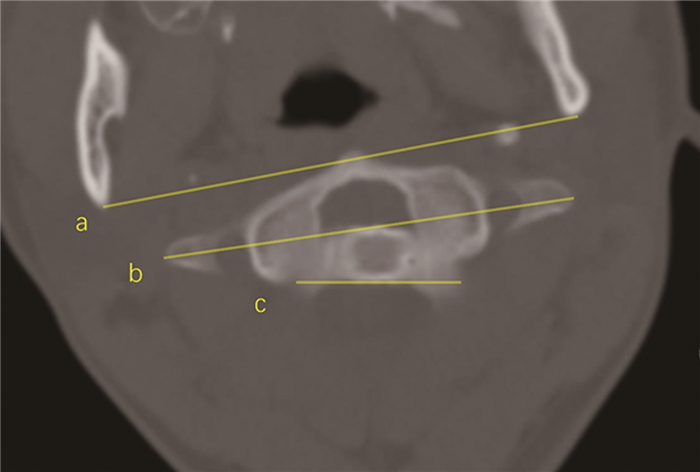
(2) 旋转分离角测量方法以双下颌支后缘连线代替枕骨的实时位置,寰椎横突连线代表寰椎实时位置,枢椎椎体后缘平行线代表枢椎实时位置。在北京大学第三医院PACS系统上测量寰枢旋转分离角(rotated separation angle of atlanto-axial joint, C1C2)与寰枕旋转分离角(rotated separation angle of occipito-atlantal joint, OcC1)。未能在同一CT切面中找到寰椎和枢椎时则通过测量枕枢旋转分离角(rotated separation angle of occipito-axial joint, OcC2),并通过OcC1+C1C2=OcC2计算得到C1C2。寰枢旋转分离角,在其他文献中也被称为寰枢椎相对旋转角度(rotating angle of atlas on dentate, RAAD)[8-9]。
|
图 1 寰枢关节旋转固定性脱位患者头颈CT旋转分离角测量方法示意图 Fig.1 Measurements for rotated separation angle of cranial CT in AARD children 注 直线a、b、c分别代表枕骨、寰椎、枢椎的实时位置 |
采用SPSS 27.0进行统计学分析。为了更好地利用数据并分析角度特征,本研究以寰椎相对枢椎的旋转方向为正(即在每个病例中以C1C2为正值,对OcC1、OcC2的正负号进行相应处理)。服从正态分布的计量资料以x±s表示,非正态分布的计量资料以M(Q1,Q3)表示。相关性分析根据变量是否服从正态分布,分别采用Pearson或Spearman相关。根据寰枕关节旋转是否在儿童生理旋转范围内,将所有患儿分为OcC1绝对值(|OcC1|)≤3°组(n=9)和|OcC1|>3°组(n=10);采用两独立样本t检验对比|OcC1|≤3°组和|OcC1|>3°组之间C1C2、OcC2的差异[10];采用线性回归对不同旋转分离角之间的变化特征进行分析。P<0.05为差异有统计学意义。
结果 一、整体相关性对OcC1、C1C2、OcC2两两之间进行相关性分析,结果显示OcC1与C1C2呈显著负相关(P<0.001),OcC2与C1C2呈显著正相关(P=0.006),而OcC1与OcC2的相关性不显著(P=0.892),见表 1。线性回归方程:OcC1=-0.66×C1C2+8.24(R2=0.727,P<0.001),OcC2=0.32×C1C2+8.25(R2=0.362,P=0.006)。
| 表 1 19例寰枢关节旋转固定性脱位患者寰枢旋转分离角、寰枕旋转分离角、枕枢旋转分离角之间的相关性 Table 1 Correlations between rotated separation angle of occipito-atlantal joint (OcC1), rotated separation angle of occipito-axial joint (OcC2) and rotated separation angle of atlantal-axial joint (C1C2) in 19AARD children |
|
|
|OcC1|≤3°组与|OcC1|>3°组之间的C1C2差异有统计学意义(P=0.011),OcC2差异无统计学意义(P=0.719);见表 2。
| 表 2 |OcC1|≤3°组与|OcC1|>3°组寰枢关节旋转固定性脱位患者的寰枢旋转分离角、枕枢旋转分离角数据比较 Table 2 Comparison of C1C2 and OcC2 in AARD children grouped according to whether or not |OcC1| was greater than 3° |
|
|
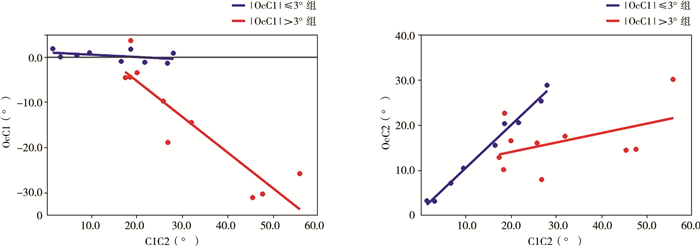
分组对OcC1与C1C2、OcC2与C1C2进行回归分析,|OcC1|>3°组的OcC1与C1C2线性回归方程(OcC1=-0.79×C1C2+10.44,R2=0.823,P<0.001)以及|OcC1|≤3°组的OcC2与C1C2线性回归方程(OcC2=0.95×C1C2+1.09,R2=0.987,P<0.001)拟合程度均较高;见图 2。
|
图 2 19例寰枢关节旋转固定性脱位患者根据寰枕旋转分离角绝对值是否大于3°分组后寰枕旋转分离角、枕枢旋转分离角与寰枢旋转分离角之间的线性回归分析图 Fig.2 Linear regression correlations between C1C2, OcC1 and OcC2 in AARD children after grouping according to whether or not |OcC1| was greater than 3° 注 A:OcC1与C1C2的线性回归结果,|OcC1|≤3°组的回归方程为OcC1=-0.05×C1C2+1.07(R2=0.180,P=0.255),|OcC1|>3°组的回归方程为OcC1=-0.79×C1C2+10.44(R2=0.823,P<0.001);B:OcC2与C1C2的线性回归结果,|OcC1|≤3°组的回归方程为OcC2=0.95×C1C2+1.09(R2=0.987,P<0.001),|OcC1|>3°组的回归方程为OcC2=0.21×C1C2+9.90(R2=0.216,P=0.176);C1C2:寰枢旋转分离角;OcC1:寰枕旋转分离角;OcC2:枕枢旋转分离角 |
AARF/D在其他文献中也被称为寰枢旋转半脱位(atlanto-axial rotatory subluxation, AARS)、寰枢旋转畸形以及寰枢旋转移位[11-14]。Fielding等[15]最早于1977年根据寰椎侧块脱位情况以及寰齿前间隙(atlas-dens interval, ADI)是否大于5 mm将AARD分为四类。Pang等[16]于2005年根据患者病程和解除“铰锁”的难易程度对寰枢关节旋转固定(atlanto-axial rotatory fixation, AARF)提出了新的分类。北京大学第三医院闫明等[1]根据此类疾病的共同发病机制、临床特征以及逐渐发展加重的关系将其统称为AARF/D,并根据ADI是否大于5 mm、寰椎侧块的脱位情况、寰枕关节脱位情况提出AARF/D的A、B、C三种分型,分别对应寰枢关节旋转固定、寰枢关节旋转固定性脱位以及枕寰枢关节旋转脱位(occipito-atlanto-axial rotatory dislocation, OAARD)[1, 3]。早期的AARF若不及时接受治疗,长期旋转移位可能导致寰椎横韧带断裂或逐渐松弛,当ADI>5 mm,则发展为AARD[1]。AARF或AARD中的B2型(一侧寰椎侧块前脱位,另一侧后脱位,是AARD中寰枢相对旋转程度最大的一类)寰枕关节反向旋转逐渐加重,在晚期可能发展为寰枕关节脱位,即OAARD[1, 3-5]。
寰枢关节旋转移位固定后患儿会出现斜颈,导致视觉歪斜,由强烈的视轴调节本能驱动,患儿下意识地收缩胸锁乳突肌,做出寰枕关节联合下颈椎反向旋转移位的努力,以代偿寰枢关节的旋转移位。在正常状态下,枕骨髁与寰椎侧块关节面紧密对合,寰枕关节的旋转运动幅度较小,在生理性旋转的范围内,正常儿童的寰枕旋转分离角不会超过3°[10]。胸锁乳突肌长期牵拉可能导致寰枕关节周围的肌肉和韧带松弛或拉伸,使儿童的OcC1超过3°,形成病理状态的寰枕关节旋转分离。寰枕关节的松弛不利于借助头骨作为杠杆力臂来减少寰枢关节不稳定[2]。
Pang等[2]通过研究不同病程AARF患者的OcC1,发现急性期(病程1个月以内)、亚急性期(1~3个月)和慢性期(病程3个月以上)患者之间的OcC1存在明显差异,平均OcC1分别为5°、9.1°、31.2°,仅慢性期患者的OcC1与寰椎朝向角度(反映寰枢关节旋转分离程度)存在较强的相关性(r=0.801,P=0.005)。说明随着病程延长,AARF患者的头部逐渐偏离了原来与寰椎的对合,向正中位偏移,大部分代偿发生在寰枢关节持续固定3个月后,通常由寰枕关节松弛度增大所致。但是有其他学者认为,AARF患者中的代偿性寰枕关节反方向旋转出现于亚急性期,晚期寰枕关节反向旋转的程度进一步增大,枕骨的朝向往往与枢椎及下颈椎一致[4]。Pang等[2]还通过计算从AARF患者急性期到慢性期OcC1与枕骨朝向角变化值的比值,得出寰枕关节代偿占总代偿的60% ~70%,下颈椎代偿仅占总代偿的30% ~40%。由于AARF病例的寰枢关节旋转角度普遍较大,该研究纳入的病例自然状态下的C1C2范围在25° ~49°,未讨论C1C2小于25°的情况。
闫明等[3]通过研究3例AARF患者、36例AARD患者以及1例OAARD患者寰枕旋转分离角与寰枢旋转分离角的关系,发现寰枕关节的反向旋转移位程度与寰枢关节旋转的程度成正比,相关性大小顺序为OAARD>AARD >AARF,其中AARD中仅一侧寰椎侧块前脱位、另一侧后脱位的这一类型,由于寰枢旋转分离程度较大,存在寰枕关节代偿现象,而AARD中其他寰椎侧块脱位情况(如一侧寰椎侧块前脱位、另一侧原位以及双侧寰椎侧块不对称前脱位)则未发现寰枕关节代偿;个别AARD患者还存在寰枕关节自发融合的现象。但该研究未对寰枕关节代偿与寰枢关节旋转分离正相关的大小进一步定量分析。OAARD较罕见,但许多文献报道OAARD存在巨大的寰枕关节代偿,寰枕旋转分离角与寰枢旋转分离角的比值在62% ~90%[1, 5-7, 17-18]。寰枕关节反向旋转位移逐渐增加,由枕骨髁骑跨在寰椎侧块关节面边缘发展到完全脱位,以此来代偿巨大的寰枢关节旋转。枕骨髁-寰椎间隙(condyle-C1 interval, CCI)已被提议作为AOD的一种诊断方法,具有高灵敏度、特异度[19]。CCI直接反映寰枕关节完整性,正常儿童的CCI应小于2 mm,且不会随着年龄增长发生显著变化(从出生到18岁)[20]。
本文探究了AARD患者在不同寰枢关节旋转移位下寰枕关节的代偿情况。C1C2与OcC1在|OcC1|≤3°组和|OcC1|>3°组中呈现不同的变化规律。在|OcC1|≤3°组中,C1C2的95%置信区间是0° ~20.8°,此时OcC1在横轴上下波动,呈现一个“平台”;C1C2与OcC2回归模型中的斜率接近于1同样佐证了这一规律(图 2)。|OcC1|>3°组中,随着C1C2的增大,OcC1往相反的方向代偿增大,回归方程为OcC1=-0.79×C1C2+10.44(R2=0.823,P<0.001)。回归直线不经过原点,说明当C1C2大于20.8°时寰枕关节开始代偿:随着寰椎和枢椎旋转分离程度的增大,寰枕关节先是保持相对固定,在生理性的分离角度内活动,不发生代偿;寰枢关节分离程度逐渐增大,当其超过临界值(20.8°)后,寰枕关节的代偿机制启动,且OcC1仅对C1C2旋转分离超出临界值的部分进行代偿。这一结果验证了闫明等[3]报道的“AARD中寰枕关节的反向旋转移位程度与寰枢关节旋转程度成正比”这一观点,并进一步得出寰枕关节代偿在寰枢关节旋转位移大于20.8°时开始出现。
|OcC1|>3°组线性回归模型的斜率(0.79)提示,当寰枢旋转角度超过临界值,寰枢旋转分离角每增加1°,寰枕关节反向旋转增加0.79°,大致说明AARD中寰枕关节的反向代偿占所有因素对寰枢关节旋转总代偿的79%。Pang等[2]研究AARF患者得出这一比例为60% ~70%,这种差异可能与研究对象和研究方法的不同有关。|OcC1|≤3°组的单侧95%置信区间的上限(20.85°)与|OcC1|>3°组的95%置信区间的下限(20.77°)较接近,坐标轴横轴在20°左右散点图出现拐点,提示这一临界角度(20.8°)很有可能是代偿的起点,但目前这一角度尚无文献报道,值得我们关注。
本研究结果为临床医生提供了AARD患者晚期寰枕关节代偿情况的预测模型。临床医生可以通过轴位CT测量AARD患者的寰枢旋转分离角,若小于20.8°则不太可能发生病理性寰枕关节代偿;若大于20.8°则可参考线性方程OcC1=-0.79×C1C2+10.44计算晚期寰枕关节代偿角度。在临界值以内,寰枕关节代偿不明显的原因可能是此时视轴歪斜的程度不高,儿童更可能通过其他途径(如转动眼球或下颈椎反向旋转)代偿,而不是通过收紧胸锁乳突肌转动头部。本研究的局限性在于样本量相对较小,亦未进行预测方程的验证,研究未关注病例的术后转归,且具体机制未探清,这些有待进一步研究。
综上,本文通过19例AARD患者的CT数据,验证了寰枕关节代偿角度与寰枢关节的旋转程度成正比;当AARD患者寰枢旋转分离角大于临界值(20.8°)时,其寰枕关节才可能开始反向旋转代偿寰枢关节的旋转移位。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 文献检索为兰麒锋、闫明、许南方,数据收集与分析为兰麒锋、王圣林、周星语,论文结果撰写为兰麒锋、周星语、许南方,论文讨论分析为兰麒锋、闫明、王圣林
| [1] |
闫明, 王超, 王圣林. 慢性寰枢关节旋转固定或脱位的临床及影像学特征-52例病例资料分析[J]. 中国脊柱脊髓杂志, 2019, 29(9): 782-790. Yan M, Wang C, Wang SL. Clinical manifestations and imaging characteristics of chronic atlantoaxial rotatory fixation or dislocation[J]. Chin J Spine Spinal Cord, 2019, 29(9): 782-790. DOI:10.3969/j.issn.1004-406X.2019.09.02 |
| [2] |
Pang D, Li V. Atlantoaxial rotatory fixation: part 3-a prospective study of the clinical manifestation, diagnosis, management, and outcome of children with alantoaxial rotatory fixation[J]. Neurosurgery, 2005, 57(5): 954-972. DOI:10.1227/01.neu.0000180052.81699.81 |
| [3] |
闫明, 王圣林, 张有余. 慢性寰枢关节旋转固定或脱位复位前后寰枕关节影像学变化[J]. 中国脊柱脊髓杂志, 2020, 30(4): 331-337. Yan M, Wang SL, Zhang YY. Retrospective radiographic study of Occipito-atlantal joint for patients with chronic atlanto-axial rotatory fixation or dislocation[J]. Chin J Spine Spinal Cord, 2020, 30(4): 331-337. DOI:10.3969/j.issn.1004-406X.2020.04.07 |
| [4] |
Ono K, Yonenobu K, Fuji T, et al. Atlantoaxial rotatory fixation.Radiographic study of its mechanism[J]. Spine (Phila Pa 1976), 1985, 10(7): 602-608. |
| [5] |
Koljonen PA, Cheung KM. Concomitant atlantoaxial and atlanto-occipital rotatory dislocation in children: Radiological features, diagnostic pitfalls, and long-term outcome[J]. J Orthop Surg (Hong Kong), 2021, 29(2): 23094990211015502. DOI:10.1177/23094990211015502 |
| [6] |
Fusco MR, Hankinson TC, Rozzelle CJ. Combined occipitoatlantoaxial rotatory fixation[J]. J Neurosurg Pediatr, 2011, 8(2): 198-204. DOI:10.3171/2011.5.PEDS10496 |
| [7] |
Clark CR, Kathol MH, Walsh T, et al. Atlantoaxial rotatory fixation with compensatory counter occipitoatlantal subluxation.A case report[J]. Spine (Phila Pa 1976), 1986, 11(10): 1048-1050. DOI:10.1097/00007632-198612000-00020 |
| [8] |
田曼曼, 林敏, 钱琦, 等. 寰枢关节多层螺旋CT旋转功能位影像学观测[J]. 中国骨伤, 2015, 28(10): 915-919. Tian MM, Lin M, Qian Q, et al. MSCT imaging analysis on atlanto-axial joint in rotary functional position[J]. Chin J Orthopa Trauma, 2015, 28(10): 915-919. DOI:10.3969/j.issn.1003-0034.2015.10.008 |
| [9] |
张晓波. 儿童寰枢关节旋转性半脱位的影像学分析及临床意义[D]. 重庆: 重庆医科大学, 2013. Zhang XB. Imaging analysis and clinical significance in the diagnosis and treatment of children with atlantoaxial rotatory subluxation[D]. Chongqing: Chongqing Medical University, 2013. |
| [10] |
Pang D, Li V. Atlantoaxial rotatory fixation: part 1-biomechanics of normal rotation at the atlantoaxial joint in children[J]. Neurosurgery, 2004, 55(3): 614-626. DOI:10.1227/01.neu.0000134386.31806.a6 |
| [11] |
王怀铿, 裴新红, 黄少敏, 等. 儿童寰枢椎旋转性半脱位的临床特征分析[J]. 临床小儿外科杂志, 2019, 18(10): 868-873. Wang HK, Pei XH, Huang SM, et al. Clinical characteristics of atlanto-axial rotatory subluxation in children[J]. J Clin Ped Sur, 2019, 18(10): 868-873. DOI:10.3969/j.issn.1671-6353.2019.10.014 |
| [12] |
Jeszenszky D, Fekete T, Kleinstück F, et al. Transoral closed reduction of fixed atlanto-axial rotatory-subluxation in childhood and adolescence[J]. Clin Spine Surg, 2018, 31(5): E252-E256. DOI:10.1097/BSD.0000000000000563 |
| [13] |
Martinez-Lage JF, Martinez Perez M, Fernandez Cornejo V, et al. Atlanto-axial rotatory subluxation in children: early management[J]. Acta Neurochir (Wien), 2001, 143(12): 1223-1228. DOI:10.1007/s007010100018 |
| [14] |
Subach BR, McLaughlin MR, Albright AL, et al. Current management of pediatric atlantoaxial rotatory subluxation[J]. Spine (Phila Pa 1976), 1998, 23(20): 2174-2179. DOI:10.1097/00007632-199810150-00006 |
| [15] |
Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation: Fixed rotatory subluxation of the atlanto-axial joint[J]. J Bone Joint Surg Am, 1977, 59(1): 37-44. |
| [16] |
Pang D, Li V. Atlantoaxial rotatory fixation: part 2-new diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging[J]. Neurosurgery, 2005, 57(5): 941-953. DOI:10.1227/01.neu.0000181309.13211.3a |
| [17] |
Kashii M, Masuhara K, Kaito T, et al. Rotatory subluxation and facet deformity in the atlanto-occipital joint in patients with chronic atlantoaxial rotatory fixation: two case reports[J]. J Orthop Case Rep, 2017, 7(6): 59-63. DOI:10.13107/jocr.2250-0685.950 |
| [18] |
Krengel WF 3rd, Kim PH, Wiater B. Spontaneous ankylosis of occiput to C2 following closed traction and halo treatment of atlantoaxial rotary fixation[J]. Global Spine J, 2015, 5(3): 233-238. DOI:10.1055/s-0035-1549432 |
| [19] |
Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation-part 2:the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children[J]. Neurosurgery, 2007, 61(5): 995-1015. DOI:10.1227/01.neu.0000303196.87672.78 |
| [20] |
Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation: part 1-normal occipital condyle-C1 interval in 89 children[J]. Neurosurgery, 2007, 61(3): 514-521. DOI:10.1227/01.NEU.0000290897.77448.1F |
 2023, Vol. 22
2023, Vol. 22


