桡骨远端骨折是儿童最常见的骨折类型,约占所有儿童骨折的40%[1-3]。其中伴骨膜完全破裂的桡骨远端骨干与干骺端交界区骨折因其位置特殊,通常被认为是不稳定骨折[4]。根据内固定问题研究协会(arbeitsgemeinschaftfür osteosynthesefragen, AO)关于儿童长骨骨折的定位和分型,在尺桡骨远端以骨骺板为底边向骨干方向绘制正方形,干骺端即为正方形覆盖部位。儿童桡骨远端骨折中,骨干与干骺端交界区的骨折被定义为骨折线中点位于桡骨远端干骺交界线远、近1 cm范围内的骨折[5-7]。儿童桡骨远端骨干与干骺端交界区骨折的手术治疗以往通常采用克氏针内固定、逆行弹性髓内针内固定等。由于儿童桡骨远端骨干与干骺端交界区骨折解剖位置特殊,此处不仅骨质相对薄弱,也不易稳定复位。目前克氏针内固定因采用平行或交叉进针,易造成角度受限;逆行弹性髓内针内固定进针时由于远端骨折段较短,易造成远端骨折段固定不稳,一定程度上限制了进针操作,故上述两种手术方式的适应证存在争议。本研究旨在探讨顺行弹性髓内针治疗儿童桡骨远端骨干与干骺端交界区骨折的临床疗效。
资料与方法 一、一般资料本研究为回顾性研究,以2019年1月至2022年1月于青岛大学医学院附属医院就诊的儿童桡骨远端骨干与干骺端交界区骨折患者为研究对象。纳入标准:①新发的闭合性桡骨远端骨干与干骺端交界区骨折;②采用顺行弹性髓内钉或克氏针内固定治疗;③随访时间大于3个月。排除标准:①合并桡骨头脱位;②合并腕部先天畸形或腕部陈旧性骨折;③合并严重前臂血管、神经损伤;④病理性骨折。最终本研究共纳入50例患儿,男43例,女7例;年龄(9.4±2.6)岁。根据手术方式的不同,将50例患儿分别纳入顺行弹性髓内针组及克氏针组。顺行弹性髓内针组17例,男15例,女2例,合并尺骨远端骨折4例。克氏针组33例,男28例,女5例,合并尺骨远端骨折9例。本研究获得青岛大学医学院附属医院医学伦理委员会批准(QYFYWZLL27270),所有患儿家属均知情同意。
二、手术方法顺行弹性髓内针组:术前拍摄患肢尺桡骨数字化X线(digital radiography, DR)正侧位片。患儿取仰卧位,全身麻醉成功后先予手法复位,C臂透视确定对位对线良好后常规消毒、铺巾,前臂置于C臂透视机上。以桡骨髓腔最狭窄处2/3直径为参照依据,选取不同直径的弹性髓内针,于桡骨近端背外侧3 cm左右处(图 1)取0.5 cm手术切口,分离肌间隙直达桡骨表面,用尖端扩口器扩开骨皮质,将弹性髓内针尖端轻度C型预弯后旋转推动置入髓腔,过程中如果髓内针尖端过直,且用锤子敲击时容易穿过对侧骨皮质,则进针技巧为一边旋转一边用手推动,待弹性髓内针抵达骨折线后,于C臂透视下再次采用对抗牵引手法复位。若复位困难,可辅以克氏针于前臂远端骨折线处桡背侧进针撬拨复位。注意弹性髓内钉应抵达桡骨骨折远端干骺端,但不应穿过生长板。复查尺桡骨DR正侧位片,以确保复位满意。于桡骨近端骨表面髓内针尾距离进针点约0.5 cm处将髓内针剪断,注意避免留针过长导致皮肤激惹,或留针过短导致取出困难。用血管钳挑起针尾周围软组织,将钉尾端覆盖于肌肉及皮下(图 2)。最后过患肢腕关节及肘关节行石膏托外固定,记录手术时间。

|
图 1 顺行弹性髓内针治疗1例5岁男性患儿左桡骨远端骨干与干骺端交界区骨折的进针点选取 Fig.1 Selection of entry point for antegrade elastic intramedullary nail in the treatment of a 5-year-old male child with fracture at the junction of distal shaft and metaphysis of left radius. 注 A:前臂解剖图切面,进针点选在桡骨近端背外侧3 cm左右;B: 术中顺行弹性髓内针进针点选取的辅助解剖示意图 |
|
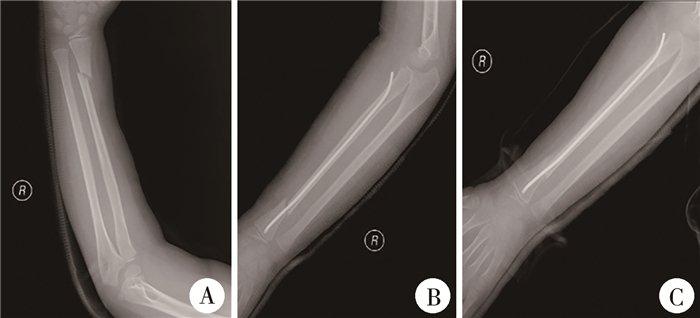
图 2 顺行弹性髓内针治疗1例9岁男性右桡骨远端骨干与干骺端交界区骨折患儿手术前后的右桡骨数字化X线片对比 Fig.2 Anterograde elastic intramedullary needling of a 9-year-old boy with distal diaphyseal junction fracture of right radius before and after surgery 注 A:术前右桡骨数字化X线片示右桡骨远端骨干与干骺端交界区骨折,完全移位; B:术后右桡骨数字化X线片示经顺行弹性髓内针治疗后,骨折对位、对线良好; C:术后3个月右桡骨数字化X线片示骨折线模糊,骨折愈合良好 |
克氏针组:术前及麻醉处理同顺行弹性髓内针组。选择1.5~2.0 mm克氏针,第1枚克氏针进针点选择在骨折线远端,可穿过骺板,借助患肢尺桡骨DR正侧位片调整克氏针进针角度及方向,使其穿过骨折断端。第2枚克氏针由桡骨骨折远端向近端进针,两枚克氏针平行或交叉以固定骨折断端,注意避免克氏针进入关节腔。复位不满意时,可将两枚克氏针依次取出,重新对抗牵引后再次进针。若复位困难,可辅以克氏针于前臂远端骨折线处桡背侧进针撬拨复位。尺桡骨DR正侧位片提示骨折断面对位、对线良好时,向近端手背方向折弯克氏针,剪断其尾部,预留距皮肤长度约0.5 cm,将尾部置于皮外。最后过患肢腕关节及肘关节行石膏托外固定,记录手术时间。
对于合并尺骨远端骨折的患儿,均于评估尺骨远端骨折线位置及骨折端稳定性后,酌情采用对抗牵引手法复位或采用克氏针、弹性髓内钉内固定。
三、围术期处理及预后评估两组均于术前30 min预防性应用抗生素1次,若手术时间超过2 h,则术后加用抗生素1次;术后均予以4 h心电监护、血压监测、面罩吸氧、常规补液以及消肿止痛等对症支持治疗。术后第1天起均指导患儿进行掌指、指间关节锻炼。分别于术后1、2、3、4周拍摄尺桡骨正侧位X线片,观察骨折对位及愈合情况。出院后均随访3~6个月,根据患儿情况拆除石膏外固定,拆除石膏后指导患儿进行腕关节及肘关节康复训练。
术中记录手术时间。随访过程中记录石膏外固定时间,术后第2周X线复查骨折成角、对位情况,术后3个月评估腕关节桡偏、尺偏、掌屈、背伸功能及并发症发生情况。采用Garland-Werley评分评价腕关节功能优良率,得分0~2分为优、3~8分为良、9~20分为可、≥21分为差,优良率=(优+良) 例数/总例数×100%。采用Broberg-Morrey评分系统对肘关节功能进行评分,满分为100分,得分95~100分为优,80~94分为良,60~79分为可,<60分为差,优良率=(优+良)例数/总例数×100%。
四、统计学处理采用SPSS 26.0进行统计学分析。采用单样本K-S检验对所有计量资料进行正态性检验,服从正态分布计量资料采用x±s表示,组间比较采用独立样本t检验或配对t检验;不服从正态分布的计量资料采用M(Q1,Q3)表示,组间比较采用Mann-Whitney秩和检验或配对秩和检验。P<0.05为差异有统计学意义。
结果 一、手术时间及术后骨折愈合情况顺行弹性髓内针组患儿手术时间长于克氏针组[(81.8±38.4)min比(59.4±26.1)min],差异无统计学意义(P>0.05);术后2周骨折平均对位率大于克氏针组(92%比88%),差异无统计学意义(P>0.05);拆除石膏外固定时间短于克氏针组[(31.5±5.1)d比(39.0±9.2)d],差异有统计学意义(P<0.05)。
二、关节活动恢复情况测量术后3个月腕关节活动度,顺行弹性髓内针组组测量结果大于克氏针组(P<0.05),见表 1。顺行弹性髓内针组腕关节功能优良率高于克氏针组,差异有统计学意义(P<0.05),见表 2。顺行弹性髓内针组肘关节功能优良率低于克氏针组,差异无统计学意义(P>0.05),见表 3。
| 表 1 两组桡骨干与干骺交界区骨折患儿腕关节活动度比较(x±s,°) Table 1 Comparing wrist range of motion between two groups (x±s, °) |
|
|
| 表 2 两组桡骨干与干骺交界区骨折患儿Garland-Werley腕关节功能评分优良率比较(例) Table 2 Comparing excellent/good rate of Garland-Werley wrist function score between two groups (n) |
|
|
| 表 3 两组桡骨干与干骺交界区骨折患儿Broberg-Morrey肘关节功能评分优良率比较(例) Table 3 Comparing excellent/good rate of Broberg-Morrey elbow function score between two groups (n) |
|
|
两组术后均无一例发生骨折不愈合、骨髓炎;顺行弹性髓内针组发生皮肤激惹1例,取针后症状消失。克氏针组发生拇长伸肌腱损伤2例,皮肤激惹2例,皮肤激惹于取针后消失。两组术后并发症发生率差异无统计学意义(P>0.05)。
讨论儿童及青少年正处于骨骼发育期,解剖复位及有效固定是桡骨远端不稳定骨折的首选治疗方法。干骺端骨折首选经皮克氏针交叉固定[3, 8-10]。弹性髓内针固定是儿童长骨骨干骨折的首选治疗方法[2]。与桡骨干骺端骨折相比,骨折线偏向桡骨近端,克氏针平行或交叉进针由于角度受限,操作性和稳定性较差。桡骨干骨折常用的逆行髓内针内固定应用于儿童桡骨远端骨干与干骺端交界区骨折时,由于远端骨折段较短,一定程度上限制了进针操作。儿童桡骨远端骨干与干骺端交界区骨折也可采用钢板内固定进行治疗,钢板提供了良好和稳定的复位,但会造成切口较大,并损伤骨膜,导致较慢的愈合速度和较高的再骨折率。
本研究中,我们对顺行弹性髓内针内固定术与克氏针内固定术的临床疗效进行了比较。顺行弹性髓内针内固定术进针位置选择在桡骨背外侧及肱桡关节线远端2~4 cm处,由于此进针点避免了对腕关节的损伤,故术后3个月顺行弹性髓内针组腕关节活动度及腕关节功能优良率均大于克氏针组。且该进针点是指伸肌和尺腕伸肌之间的间隙,为乏神经区,桡骨仅被较薄的后旋肌覆盖,选择此处进针不仅更易操作,对肘关节功能的影响也较小。根据两组术后并发症情况可知,顺行弹性髓内针内固定可在一定程度上减少拇长伸肌腱的损伤,提示顺行弹性髓内针内固定的进针位置更加安全。由于术后患儿患肢消肿,使石膏外固定较前松动,加之肌肉牵拉、骨折远端可致骨折成角或移位,对比术后2周的X线结果,顺行弹性髓内针组较克氏针组骨折成角小,且对位面积大,一定程度上说明顺行弹性髓内针内固定术更有利于骨折断端恢复良好的力学稳定性,从而促进骨痂形成,有利于骨折早期愈合[11]。
针尾刺激征产生的皮肤激惹是弹性髓内针技术最常见的术后并发症。选择合适进针点及掌握操作技巧、妥善处理针尾,可使并发症发生率降低[12]。顺行弹性髓内针固定技术因桡骨近端软组织覆盖多,故减少了针尾刺激导致的皮肤激惹现象。本研究结果表明,儿童桡骨远端骨干与干骺端交界区骨折采用顺行弹性髓内针治疗的疗效较克氏针好,顺行弹性髓内针内固定术是治疗儿童桡骨远端骨干与干骺端交界区骨折的可选手术方法,具有微创、易操作、复位稳定、有利于术后恢复等优点。但本研究存在一定局限性,因儿童桡骨远端骨干- 干骺端交界区骨折患者例数较少,本研究结果可能存在偏倚,可通过增加样本量并设置相应的对照组展开进一步研究。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 石佳宁、李富江、张琳负责研究的设计、实施和起草文章;石佳宁、周显军、段于河、英庆龙进行病例数据收集及分析;李富江、邢茂青负责研究设计与酝酿,并对文章知识性内容进行审阅
| [1] |
Cheng JC, Ng BK, Ying SY, et al. A 10-year study of the changes in the pattern and treatment of 6, 493 fractures[J]. J Pediatr Orthop, 1999, 19(3): 344-350. |
| [2] |
Bae DS. Pediatric distal radius and forearm fractures[J]. J Hand Surg Am, 2008, 33(10): 1911-1923. DOI:10.1016/j.jhsa.2008.10.013 |
| [3] |
杜智军, 陆士姣, 张友波. 弹性髓内针顺行固定治疗儿童桡骨远端干骺端移行部骨折[J]. 中国矫形外科杂志, 2017, 25(24): 2290-2293. Du ZJ, Lu SJ, Zhang YB. Elastic intramedullary needling for anterograde fixation of distal radius metaphyseal transition fractures in children[J]. Orthop J China, 2017, 25(24): 2290-2293. DOI:10.3977/j.issn.1005-8478.2017.24.19 |
| [4] |
Bae DS, Waters PM. Pediatric distal radius fractures and triangular fibrocartilage complex injuries[J]. Hand Clin, 2006, 22(1): 43-53. DOI:10.1016/j.hcl.2005.09.002 |
| [5] |
Slongo T, Audigé L, Lutz N, et al. Documentation of fracture severity with the AO classification of pediatric long-bone fractures[J]. Acta Orthop, 2007, 78(2): 247-253. DOI:10.1080/17453670710013753 |
| [6] |
徐蕴岚, 沈恺颖, 王志刚. 弹性髓内钉在儿童长骨干骺交界区骨折中的治疗体会[J]. 中国矫形外科杂志, 2016, 24(16): 1455-1461. Xu YL, Shen KY, Wang ZG. Elastic stable intramedullary nailing for fracture locating at borderline between diaphysis and metaphysis of long bone in children[J]. Orthop J China, 2016, 24(16): 1455-1461. DOI:10.3977/j.issn.1005-8478.2016.16.04 |
| [7] |
杜蒙蒙. 顺行弹性髓内钉治疗儿童桡骨远端骨干与干骺端交界区骨折: 一种新的手术入路[D]. 石家庄: 河北医科大学, 2019. Du MM. Antegrade elastic stable intramedullary nail fixation for pediatric distal radial diaphyseal metaphyseal junction fractures: a novel operative approach[D]. Shijiazhuang: Hebei Medical University, 2019. |
| [8] |
Lieber J, Schmid E, Schmittenbecher PP. Unstable diametaphyseal forearm fractures: transepiphyseal intramedullary Kirschner-wire fixation as a treatment option in children[J]. Eur J Pediatr Surg, 2010, 20(6): 395-398. DOI:10.1055/s-0030-1262843 |
| [9] |
Yung PSH, Lam CY, Ng BKW, et al. Percutaneous transphyseal intramedullary Kirschner wire pinning: a safe and effective procedure for treatment of displaced diaphyseal forearm fracture in children[J]. J Pediatr Orthop, 2004, 24(1): 7-12. DOI:10.1097/00004694-200401000-00002 |
| [10] |
Miller BS, Taylor B, Widmann RF, et al. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: a prospective, randomized study[J]. J Pediatr Orthop, 2005, 25(4): 490-494. DOI:10.1097/01.bpo.0000158780.52849.39 |
| [11] |
呼和, 蒋飞, 侯利民, 等. 两种手术方法治疗儿童桡骨远段1/3处骨折[J]. 临床骨科杂志, 2020, 23(3): 384-386. Hu H, Jiang F, Hou LM, et al. Two surgical approaches for distal 1/3 humeral fracture in children[J]. J Clin Orthop, 2020, 23(3): 384-386. DOI:10.3969/j.issn.1008-0287.2020.03.029 |
| [12] |
Lieber J, Joeris A, Knorr P, et al. ESIN in forearm fractures: clear indications, often used, but some avoidable complications[J]. Eur J Trauma, 2005, 31(1): 3-11. DOI:10.1007/s00068-005-1071-7 |
 2023, Vol. 22
2023, Vol. 22


