尿道下裂是小儿常见的先天性泌尿生殖系统畸形,发病率约为1/300,近年来有升高趋势[1]。根据尿道口位置的不同, 尿道下裂可分为远端型、中段型和近端型。非远端型尿道下裂包括中段型和近端型,中段型定义为尿道开口于阴茎体中部的尿道下裂,近端型包括阴茎根部型、阴茎阴囊交界型、阴囊型和会阴型。相比于远端型尿道下裂,非远端型尿道下裂尿道缺损长,阴茎下弯程度重,术中常需横断尿道板,手术修复难度较大,术后并发症发生率更高,其术式选择一直存在争议。对于非远端型尿道下裂中需要横断尿道板以矫正阴茎下弯的患儿,一期横裁包皮岛状皮瓣尿道成形术(one-stage transverse preputial island flap urethroplasty, 一期Duckett尿道成形术)是国内应用最多的术式[2]。国外学者更倾向于采用分期移植物尿道成形术(staged graft urethroplasty, 分期Bracka尿道成形术)[3]。目前关于这两种术式的优劣尚无定论,本研究旨在运用循证医学原理评价以上两种术式治疗非远端型尿道下裂的临床疗效及安全性,以期为手术方式的选择提供参考。
资料与方法 一、文献检索策略计算机检索PubMed、Embase、Web of Science、Cochrane图书馆、中国知网、万方数据库和维普数据库。检索词包括尿道下裂、横裁包皮岛状皮瓣、Duckett术、Bracka术、移植物、hypospadias、preputial flap、foreskin flap、Bracka、graft。检索文献时限为数据库建库至2022年3月28日。此外,查找相关研究的参考文献清单,追溯纳入文献的参考文献,必要时与研究者联系,补充相关文献。
二、文献纳入与排除标准纳入标准:①随机或非随机对照试验,队列研究和病例对照研究;②研究对象为非远端型尿道下裂患者;③干预措施为一期Duckett尿道成形术或分期Bracka尿道成形术者;④初次行尿道手术者;⑤手术年龄<18岁。排除标准:①研究质量差,数据不完整等无法进行信息提取的文献;②样本量 < 10例的研究;③综述、信件、病例报告、会议摘要及具有相同数据来源的研究。
三、文献筛选流程、质量评价及数据提取方法由2名评价者通过阅读文献题目和摘要,按照纳入及排除标准筛选文献,随后查找并阅读全文进行二次筛选,由2名评价者独立进行数据提取,并交叉核对,意见不同时通过咨询相关专家及共同讨论达成一致。提取内容:①纳入研究的基本特征:第一作者、出版年份、尿道下裂类型、样本量、手术年龄和干预方式; ②结局指标:总体并发症、独立并发症(尿道瘘、尿道狭窄、尿道憩室、伤口裂开、移植物相关并发症及其他并发症)、手术次数。移植物相关并发症是指文献中记为术后并发症的移植物收缩、挛缩、瘢痕和坏死;伤口裂开是指阴茎头和(或)尿道裂开。纳入研究中无随机对照研究,使用The Newcastle Ottawa Scale(NOS)文献质量评价量表进行评价,包括选择(4分)、可比性(2分)和结局(3分),满分为9分[4]。
四、统计学处理使用RevMan 5.4进行统计学分析。首先对各项研究进行异质性检验,采用Q和I2值反映各研究间异质性,若P≤0.1,I2≥50%,可认为多项研究间异质性较大,采用随机效应模型;反之采用固定效应模型。构建森林图以比较一期Duckett尿道成形术与分期Bracka尿道成形术后总体并发症和独立并发症的发生率。采用比值比(OR)、风险差(RD)和95%置信区间(CI)分析统计量。当统计值较小时,使用卡方检验或Fisher精确概率法进行统计分析。对于研究中只报道中位数及极值的资料使用Hozo等[5]提出的方法估算均数和标准差。所有研究结果均为双侧检验结果,P < 0.05为差异具有统计学意义。
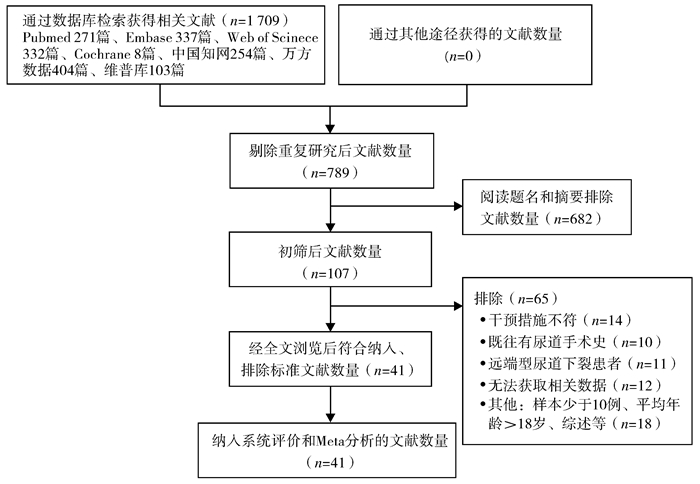
结果 一、文献筛选流程及结果共检索出文献1 709篇,其中PubMed 271篇,Embase 337篇,Web of Science 332篇,Cochrane 8篇,中国知网254篇,万方数据库404篇,维普数据库103篇。剔除重复文献后获789篇文献。阅读文献标题和摘要后初筛获107篇文献;阅读全文后最终纳入41篇文章进行Meta分析,干预方式中至少包括一期Duckett尿道成形术和分期Bracka尿道成形术且互为对照的文献有5篇。文献筛选流程见图 1。纳入文献基本特征及质量评价见表 1,纳入数据结局指标见表 2。
|
图 1 文献筛选流程图 Fig.1 Flowchart of literature screening |
| 表 1 两种手术方式治疗非远端型尿道下裂临床疗效研究文献的基本特征及质量评价 Table 1 Basic characteristics and quality evaluation of the included literature items |
|
|
| 表 2 两种手术方式治疗非远端型尿道下裂临床疗效研究文献的结局指标 Table 2 Outcomes included in the literature |
|
|
纳入41篇文献中共报道3 713例患儿,其中2 395(64.5%)例接受一期Duckett尿道成形术,平均随访时间为31.7个月;1 318(35.5%)例接受分期Bracka尿道成形术,平均随访时间为59.6个月。
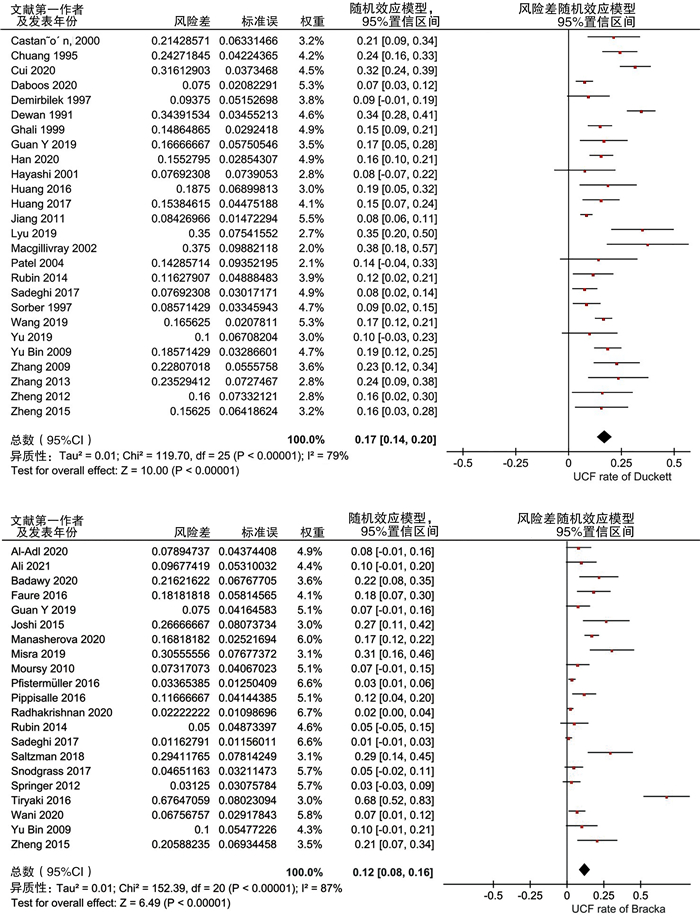
(一) 尿道瘘共41篇文献报道术后尿道瘘的发生率,一期Duckett尿道成形术与分期Bracka尿道成形术后尿道瘘的发生率分别约为17%(95%CI:0.14~0.20,I2=79%,采用随机效应模型)、10%(95%CI:0.07~0.13,I2=79%,采用随机效应模型),见图 2。
|
图 2 两种手术治疗尿道下裂后尿道瘘森林图 Fig.2 Forest plot of postoperative urethral fistula 注 UCF:urethrocutaneous fistula 尿道瘘;Duckett: 一期Duckett尿道成形术;Bracka: 分期Bracka尿道成形术 |
共34篇文献报道术后尿道狭窄的发生率,一期Duckett尿道成形术与分期Bracka尿道成形术后尿道狭窄的发生率分别约为10%(95%CI:0.07~0.13,I2=90%,采用随机效应模型)、3%(95%CI:0.02~0.04,I2=39%,采用固定效应模型),见图 3。

|
图 3 两种手术治疗尿道下裂后尿道狭窄森林图 Fig.3 Forest plot of postoperative urethral stricture 注 stenosis:狭窄;Duckett: 一期Duckett尿道成形术;Bracka: 分期Bracka尿道成形术 |
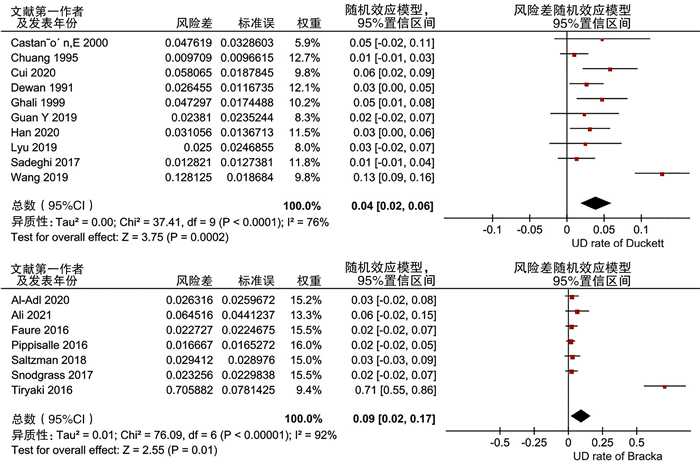
共16篇文献报道术后尿道憩室的发生率,一期Duckett尿道成形术与分期Bracka尿道成形术后尿道憩室的发生率分别约为4%(95%CI:0.02~0.06,I2=76%,采用随机效应模型)、2%(95%CI:0.01~0.04,I2=0%,采用固定效应模型),见图 4。
|
图 4 两种手术治疗尿道下裂后尿道憩室森林图 Fig.4 Forest plot of postoperative urethral diverticulum 注 UD:urethral diverticulum 尿道憩室;Duckett: 一期Duckett尿道成形术;Bracka: 分期Bracka尿道成形术 |
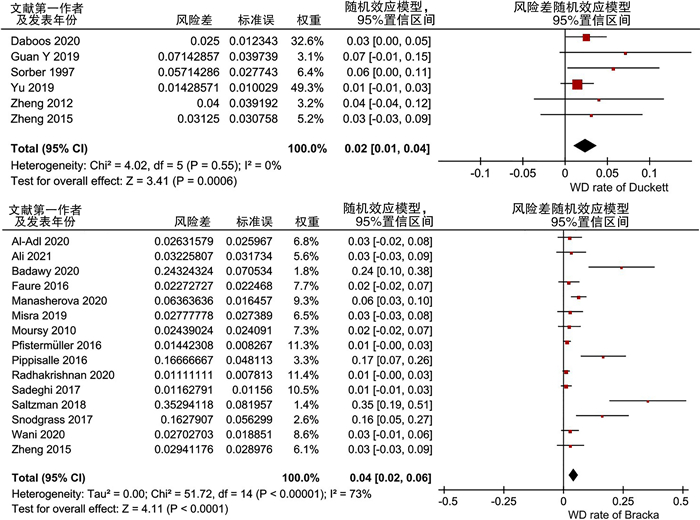
共20篇文献报道术后伤口裂开的发生率,一期Duckett尿道成形术与分期Bracka尿道成形术后伤口裂开的发生率分别约为2%(95%CI:0.01~0.04,I2=0%,固定效应模型)、4%(95%CI:0.02~0.06,I2=73%,采用随机效应模型),见图 5。
|
图 5 两种手术治疗尿道下裂后伤口裂开森林图 Fig.5 Forest plot of postoperative wound dehiscence 注 WD:wound dehiscence 伤口裂开;Duckett: 一期Duckett尿道成形术;Bracka: 分期Bracka尿道成形术 |
共5篇文献报道分期Bracka尿道成形术后移植物相关并发症的发生率,移植物相关并发症的发生率约为5%(95%CI:0.01~0.10,I2=71%,随机效应模型),见图 6。
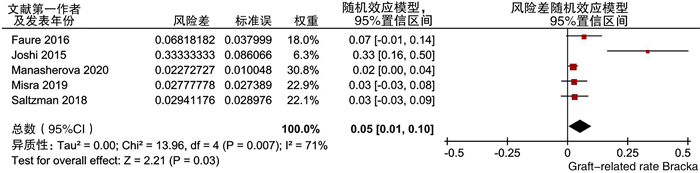
|
图 6 两种手术治疗尿道下裂后移植物相关并发症森林图 Fig.6 Forest plot of postoperative graft-related complications 注 Graft-related:移植物相关;Duckett: 一期Duckett尿道成形术;Bracka: 分期Bracka尿道成形术 |
有5篇文献报道干预措施同时包括一期Duckett尿道成形术和分期Bracka尿道成形术,且互为对照。研究之间无明显异质性(I2=22%,P=0.28),合并结果显示一期Duckett尿道成形术后总并发症发生率高于分期Bracka尿道成形术,差异有统计学意义(OR=2.63,95%CI:1.54~4.50,P<0.05,固定效应模型), 见图 7。
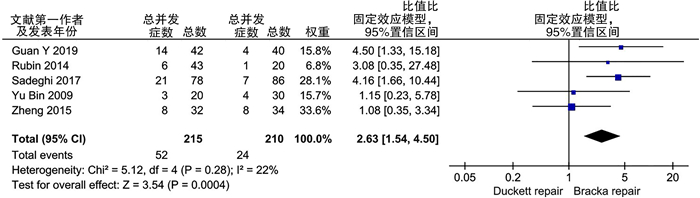
|
图 7 尿道下裂两种手术方式对比研究的术后总并发症森林图 Fig.7 Forest plot of total postoperative complications for comparative studies 注 Duckett: 一期Duckett尿道成形术;Bracka: 分期Bracka尿道成形术 |
共25篇文献报道了手术次数,包括2 082例患儿。其中1 137例接受一期Duckett尿道成形术,平均手术次数为1.29次;945例接受分期Bracka尿道成形术,平均手术次数为2.15次。
讨论尿道下裂是小儿泌尿生殖系统常见的先天性畸形,与远端型尿道下裂相比,非远端型尿道下裂治疗难度大,预后较差,术式选择存在较大争议。一期Duckett尿道成形术在国内有较广泛的应用基础,而国际上目前更倾向于选择分期Bracka尿道成形术[2-3]。这可能与临床上非远端型尿道下裂病例相对较少、缺乏一期Duckett尿道成形术经验、分期Bracka尿道成形术学习曲线较短有关[47]。近年来国内也显现出从一期转向分期的趋势,但两者优劣尚无明确共识。就术式而言,分期Bracka尿道成形术一期矫正阴茎下弯后使用移植物重建尿道板,二期行尿道成形术;而一期Duckett尿道成形术一次手术即完成阴茎下弯的矫正及尿道成形。分期Bracka尿道成形术需至少进行两次手术,比较两种术式两次手术后并发症的发生率可能更有临床意义。然而一期Duckett尿道成形术后仅部分发生并发症的患儿需进行再次手术,且纳入文献中多为初次手术后的并发症情况,故本研究仅分析分期Bracka两次手术后及一期Duckett一次手术后并发症的发生率,旨在评价一期Duckett尿道成形术与分期Bracka尿道成形术治疗非远端型尿道下裂的疗效,为手术方式的选择提供循证依据。
本研究纳入41篇文献中,报道一期Duckett尿道成形术与分期Bracka尿道成形术及其相关结果的文献分别有26篇和20篇,有5篇文献的干预措施同时包括上述两种术式,且互为对照。分析结果显示,一期Duckett尿道成形术后尿道瘘(17%)、尿道狭窄(10%)及尿道憩室的发生率(4%)均高于分期Bracka尿道成形术(10%、3%及2%),与Sadeghi等、关勇等[24-25]研究结果一致。考虑与分期手术的两次手术至少间隔6个月,有利于重建尿道板建立良好的血运,减少尿道瘘的发生有关;而一期Duckett尿道成形术中近端尿道口的环形吻合有可能增加尿道狭窄的发生率。另外,一期Duckett手术成形尿道由于缺乏与周围组织的附着,新尿道富有弹性,易于扩张,形成憩室[48]。Shukla等[49]对Duckett术式进行改良,将皮瓣边缘纵向锚定到腹面以优化尿道板的重建,从而减少尿道憩室的发生。
纳入的5篇对比研究经Meta分析显示,一期Duckett尿道成形术后总并发症的发生率高于分期Bracka术式(OR=2.63,P<0.01),其中有3篇得出相同结果[22, 24-25];另2篇的数据表明两种术式总并发症发生率差异无统计学意义[21, 23]。需强调的是,尿道下裂手术后并发症的发生率不应作为衡量术式优劣的唯一评价指标。首先,分期Bracka尿道成形术存在移植物相关并发症,本研究中一期Bracka尿道成形术后移植物相关并发症发生率经合并后估计为5%。Leslie等[50]研究发现分期颊黏膜移植中,约13%的患儿需重新进行移植。本研究结果显示一期Duckett与分期Bracka尿道成形术平均手术次数分别为1.29次与2.15次,相比于分期手术,一期Duckett尿道成形术治愈非远端型尿道下裂所需手术次数更少。此外,分期Bracka尿道成形术的治疗周期在6个月以上,相对更多的手术次数和更长的治疗周期也是手术者在进行术式选择时需要综合考虑的因素[51]。
尿道下裂的治疗决策十分复杂,术式选择受尿道下裂严重程度、术者经验及家长意愿等多方面因素影响。一期Duckett尿道成形术具有一次完成手术、平均治疗周期短的优点;分期Bracka尿道成形术后并发症的发生率相对较低。故一期Duckett尿道成形术对于伴有阴茎下弯且尿道缺损不严重的病例是较好的选择,而分期Bracka尿道成形术中移植物的使用在包皮组织少、包皮无主干血管的病例中具有不可替代的作用[25]。
本研究I2统计结果显示出高异质性,这可能与以下几个方面因素有关:①目前关于尿道下裂术式选择缺乏前瞻性队列研究和随机对照研究,本研究为回顾性研究,数据来自多个中心,异质性不可避免[52];②尿道下裂手术结局与术者经验高度相关,相比分期手术,一期Duckett尿道成形术学习曲线较长,可能导致偏倚[53]; ③尿道下裂术后并发症的发生时间存在差异,随访结果与随访时间密切相关,不同研究的随访时长可能导致相应并发症的低估,如阴茎复弯作为长期并发症,在随访时间短的文献中很少提及,无法进行统计分析;④不同文献对并发症的定义不同,部分文献报告了更多的并发症,如出血、感染、阴茎扭转、疼痛等[14, 17];而一些文献关注于主要并发症,如尿道瘘、尿道狭窄、尿道憩室[26]。此外,本研究未纳入术后阴茎外观和性功能的相关数据,这是由于其评估尚无统一标准,且需长期随访,纳入文献中数据缺失较多,也无法进行更有效的Meta分析。Castagnetti等[54]研究发现分期手术的美观效果明显优于一期手术。Rynja等[55]研究表明,一期Duckett尿道成形术可以实现与健康对照组相当的长期功能、性功能及美观效果。
综上所述,对于非远端型尿道下裂,一期Duckett尿道成形术后总并发症发生率、尿道瘘及尿道狭窄发生率高于分期Bracka尿道成形术,移植物相关并发症在分期Bracka尿道成形术后的发生率为5%。一期Duckett尿道成形术治愈非远端型尿道下裂所需手术次数更少。但现有文献中缺乏大样本、长期随访的随机对照试验以得出有效证据。此外,已有研究对于尿道下裂术后阴茎外观和青春期后性功能的评价尚缺乏统一标准,应在未来的研究中进一步完善。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 杨珍珍负责研究的设计、实施和起草文章;刘沛和李佳义进行病例数据收集及分析;宋宏程和张潍平负责研究设计与酝酿,并对文章知识性内容进行审阅
| [1] |
宋宏程. 尿道下裂专家共识[J]. 中华小儿外科杂志, 2018, 39(12): 883-888. Song HC. Expert consensus on hypospadias[J]. Chin J Pediatr Surg, 2018, 39(12): 883-888. DOI:10.3760/cma.j.issn.0253-3006.2018.12.002 |
| [2] |
李振武, 张潍平, 孙宁, 等. 国内医院尿道下裂治疗现状调查[J]. 中华小儿外科杂志, 2016, 37(6): 453-458. Li ZW, Zhang WP, Sun N, et al. Domestic trends of hypospadias surgery[J]. Chin J Pediatr Surg, 2016, 37(6): 453-458. DOI:10.3760/cma.j.issn.0253-3006.2016.06.000 |
| [3] |
Altarac S, Papeš D, Bracka A. Two-stage hypospadias repair with inner preputial layer Wolfe graft(Aivar Bracka repair)[J]. BJU Int, 2012, 110(3): 460-473. DOI:10.1111/j.1464-410X.2012.11304.x |
| [4] |
Wells G, Shea B, O'Connell J, et al. The Newcastle-Ottawa Scale(NOS)for assessing the quality of nonrandomized studies in meta-analysis[EB/OL]. [2013-04-13]. http://www.evidencebasedpublichealth.de/download/Newcastle_Ottowa_Scale_Pope_Bruce.pdf.
|
| [5] |
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample[J]. BMC Med Res Methodol, 2005, 5: 13. DOI:10.1186/1471-2288-5-13 |
| [6] |
Al-Adl AM, Abdel Aal AM, El-Karamany TM, et al. Two-stage repair of proximal hypospadias with moderate to severe chordee using inner preputial skin graft: prospective evaluation of functional and cosmetic outcomes[J]. World J Urol, 2020, 38(11): 2873-2879. DOI:10.1007/s00345-020-03075-5 |
| [7] |
Ali MM, Anwar AZ. Experience with modified two stage inner preputial flap for repair of proximal hypospadias with chordee: a single institution study with intermediate follow up[J]. J Pediatr Surg, 2022, 57(7): 1404-1408. DOI:10.1016/j.jpedsurg.2021.05.024 |
| [8] |
Badawy H, Dawood W, Soliman AS, et al. Staged repair of proximal hypospadias: reporting outcome of staged tubularized autograft repair(STAG)[J]. J Pediatr Surg, 2020, 55(12): 2710-2716. DOI:10.1016/j.jpedsurg.2020.07.023 |
| [9] |
Faure A, Bouty A, Nyo YL, et al. Two-stage graft urethroplasty for proximal and complicated hypospadias in children: a retrospective study[J]. J Pediatr Urol, 2016, 12(5): 286.e1-286.e7. DOI:10.1016/j.jpurol.2016.02.014 |
| [10] |
Joshi RS, Bachani MK, Uttarwar AM, et al. The Bracka two-stage repair for severe proximal hypospadias: a single center experience[J]. J Indian Assoc Pediatr Surg, 2015, 20(2): 72-76. DOI:10.4103/0971-9261.151549 |
| [11] |
Manasherova D, Kozyrev G, Nikolaev V, et al. Bracka's method of proximal hypospadias repair: preputial skin or buccal mucosa?[J]. Urology, 2020, 138: 138-143. DOI:10.1016/j.urology.2019.12.027 |
| [12] |
Misra D, Elbourne C, Vareli A, et al. Challenges in managing proximal hypospadias: a 17-year single-center experience[J]. J Pediatr Surg, 2019, 54(10): 2125-2129. DOI:10.1016/j.jpedsurg.2019.04.019 |
| [13] |
Moursy EE. Outcome of proximal hypospadias repair using three different techniques[J]. J Pediatr Urol, 2010, 6(1): 45-53. DOI:10.1016/j.jpurol.2009.04.013 |
| [14] |
Pfistermüller KLM, Manoharan S, Desai D, et al. Two-stage hypospadias repair with a free graft for severe primary and revision hypospadias: a single surgeon's experience with long-term follow-up[J]. J Pediatr Urol, 2017, 13(1): 35.e1-35.e7. DOI:10.1016/j.jpurol.2016.08.014 |
| [15] |
Pippi Salle JL, Sayed S, Salle A, et al. Proximal hypospadias: a persistent challenge.single institution outcome analysis of three surgical techniques over a 10-year period[J]. J Pediatr Urol, 2016, 12(1): 28.e1-28.e7. DOI:10.1016/j.jpurol.2015.06.011 |
| [16] |
Radhakrishnan CN, Radhakrishna V. The tunica-vaginalis flap to prevent postoperative fistula following severe hypospadias repair: has the search for holy grail ended?[J]. Actas Urol Esp(Engl Ed), 2021, 45(8): 552-556. DOI:10.1016/j.acuroe.2021.07.005 |
| [17] |
Saltzman AF, Carrasco A Jr, Colvin A, et al. Patients with disorders of sex development and proximal hypospadias are at high risk for reoperation[J]. World J Urol, 2018, 36(12): 2051-2058. DOI:10.1007/s00345-018-2350-3 |
| [18] |
Snodgrass W, Bush N. Staged tubularized autograft repair for primary proximal hypospadias with 30-degree or greater ventral curvature[J]. J Urol, 2017, 198(3): 680-686. DOI:10.1016/j.juro.2017.04.019 |
| [19] |
Springer A, Subramaniam R. Split dorsal dartos flap transposed ventrally as a bed for preputial skin graft in primary staged hypospadias repair[J]. Urology, 2012, 79(4): 939-942. DOI:10.1016/j.urology.2012.01.006 |
| [20] |
Wani SA, Baba AA, Mufti GN, et al. Bracka verses Byar's two-stage repair in proximal hypospadias associated with severe chordee: a randomized comparative study[J]. Pediatr Surg Int, 2020, 36(8): 965-970. DOI:10.1007/s00383-020-04697-x |
| [21] |
俞斌, 周娟, 王忠, 等. Duckett术式一期治疗尿道下裂的临床研究[J]. 中华男科学杂志, 2009, 15(1): 12-15. Yu B, Zhou J, Wang Z, et al. Ducketts procedure of one-stage urethroplasty for hypospadias[J]. Natl J Androl, 2009, 15(1): 12-15. DOI:10.13263/j.cnki.nja.2009.01.016 |
| [22] |
Rudin YE, Maruhnenko DV, Sayedov KM. Choosing the method of correction of proximal hypospadias in children[J]. Experimental & Clinical Urology, 2014(1): 81-87. |
| [23] |
Zheng DC, Yao HJ, Cai ZK, et al. Two-stage urethroplasty is a better choice for proximal hypospadias with severe chordee after urethral plate transection: a single-center experience[J]. Asian J Androl, 2015, 17(1): 94-97. DOI:10.4103/1008-682X.137688 |
| [24] |
Sadeghi A, Mirshemirani A, Tabari AK, et al. Duckett versus modified Bracka technique for proximal hypospadias repair a 10-year experience[J]. Iran J Pediatr, 2017, 27(6): e7752. DOI:10.5812/ijp.7752 |
| [25] |
关勇, 孟庆娅, 王欣, 等. Bracka法与Duckett法手术对初治近端型尿道下裂的疗效比较[J]. 中华泌尿外科杂志, 2019, 40(11): 821-824. Guan Y, Meng QY, Wang X, et al. A comparative analysis of Bracka versus Duckett in the treatment of primary proximal hypospadias[J]. Chin J Urol, 2019, 40(11): 821-824. DOI:10.3760/cma.j.issn.1000-6702.2019.11.005 |
| [26] |
Castañón M, Muñoz E, Carrasco R, et al. Treatment of proximal hypospadias with a tubularized island flap urethroplasty and the onlay technique: a comparative study[J]. J Pediatr Surg, 2000, 35(10): 1453-1455. DOI:10.1053/jpsu.2000.16412 |
| [27] |
Chuang JH, Shieh CS. Two-layer versus one-layer closure in transverse island flap repair of posterior hypospadias[J]. J Pediatr Surg, 1995, 30(5): 739-742. DOI:10.1016/0022-3468(95)90705-x |
| [28] |
Cui X, He YB, Huang WH, et al. Clinical efficacy of transverse preputial island flap urethroplasty for single-stage correction of proximal hypospadias: a single-centre experience in Chinese patients[J]. BMC Urol, 2020, 20(1): 118. DOI:10.1186/s12894-020-00686-3 |
| [29] |
Daboos M, Helal AA, Salama A. Five years' experience of double faced tubularized preputial flap for penoscrotal hypospadias repair in pediatrics[J]. J Pediatr Urol, 2020, 16(5): 673.e1-673.e7. DOI:10.1016/j.jpurol.2020.07.037 |
| [30] |
Demirbilek S, Atayurt HF. One-stage hypospadias repair with stent or suprapubic diversion: which is better?[J]. J Pediatr Surg, 1997, 32(12): 1711-1712. DOI:10.1016/s0022-3468(97)90511-x |
| [31] |
Dewan PA, Dinneen MD, Winkle D, et al. Hypospadias: Duckett pedicle tube urethroplasty[J]. Eur Urol, 1991, 20(1): 39-42. DOI:10.1159/000471657 |
| [32] |
Ghali AM. Hypospadias repair by skin flaps: a comparison of onlay preputial island flaps with either Mathieu's meatal-based or Duckett's tubularized preputial flaps[J]. BJU Int, 1999, 83(9): 1032-1038. DOI:10.1046/j.1464-410x.1999.00083.x |
| [33] |
Han WW, Zhang WP, Sun N, et al. Comparison of continuous eversion and inverting subepithelial suture in transverse preputial island flap urethroplasty in proximal hypospadias repair: a retrospective study[J]. Int Braz J Urol, 2020, 46(5): 772-777. DOI:10.1590/S1677-5538.IBJU.2019.0484 |
| [34] |
Hayashi Y, Kojima Y, Mizuno K, et al. The modified Koyanagi repair for severe proximal hypospadias[J]. BJU Int, 2001, 87(3): 235-238. DOI:10.1046/j.1464-410x.2001.02029.x |
| [35] |
Huang YC, Xie H, Lyu YQ, et al. One-stage repair of proximal hypospadias with severe chordee by in situ tubularization of the transverse preputial island flap[J]. J Pediatr Urol, 2017, 13(3): 296-299. DOI:10.1016/j.jpurol.2017.02.015 |
| [36] |
Huang LQ, Guo YF, Ge Z, et al. A new modification of the Duckett technique for one-stage repairing urethral plate transected hypospadias: another option for severe hypospadias?[J]. Int Urol Nephrol, 2017, 49(12): 2091-2097. DOI:10.1007/s11255-017-1690-z |
| [37] |
蒋先镇, 阳建福, 曾青, 等. 横向带蒂包皮皮管(Duckett术式)修补尿道下裂356例[J]. 中华男科学杂志, 2011, 17(7): 622-624. Jiang XZ, Yang JF, Zeng Q, et al. Transverse preputial island flap technique(Duckett's procedure)for hypospadias repair: a report of 356 cases[J]. Natl J Androl, 2011, 17(7): 622-624. DOI:10.13263/j.cnki.nja.2011.07.013 |
| [38] |
Lyu YQ, Yu L, Xie H, et al. Comparison of short-term complications between Onlay and Duckett urethroplasty and the analysis of risk factors[J]. Int Urol Nephrol, 2019, 51(5): 783-788. DOI:10.1007/s11255-019-02125-1 |
| [39] |
MacGillivray D, Shankar KR, Rickwood AMK. Management of severe hypospadias using Glassberg's modification of the Duckett repair[J]. BJU Int, 2002, 89(1): 101-102. DOI:10.1046/j.1464-410X.2002.02552.x |
| [40] |
Patel RP, Shukla AR, Snyder HM3rd. The island tube and island Onlay hypospadias repairs offer excellent long-term outcomes: a 14-year followup[J]. J Urol, 2004, 172(4 Pt 2): 1717-1719. DOI:10.1097/01.ju.0000138903.20136.22 |
| [41] |
Sorber M, Feitz WF, de Vries JD. Short-and mid-term outcome of different types of one-stage hypospadias corrections[J]. Eur Urol, 1997, 32(4): 475-479. DOI:10.1159/000480810 |
| [42] |
Wang CX, Zhang WP, Song HC. Complications of proximal hypospadias repair with transverse preputial island flap urethroplasty: a 15-year experience with long-term follow-up[J]. Asian J Androl, 2019, 21(3): 300-303. DOI:10.4103/aja.aja_115_18 |
| [43] |
余玲, 包杰文, 陈艳, 等. 分叉尿道海绵体修复在尿道下裂Duckett术中的应用研究[J]. 中华泌尿外科杂志, 2019, 40(11): 816-820. Yu L, Bao JW, Chen Y, et al. Application of branchedspongiosum repair in Duckett surgery for hypospadias[J]. Chin J Urol, 2019, 40(11): 816-820. DOI:10.3760/cma.j.issn.1000-6702.2019.11.004 |
| [44] |
章越龙, 肖家全, 张大宏, 等. 减少Duckett手术治疗尿道下裂并发症发生的体会[J]. 中国男科学杂志, 2009, 23(11): 30-33. Zhang YL, Xiao JQ, Zhang DH, et al. Clinical experience of reducing the failure rate of Duckett's operation for hypospadias[J]. Chin J Androl, 2009, 23(11): 30-33. DOI:10.3969/j.issn.1008-0848.2009.11.008 |
| [45] |
张卫星, 宋新浩, 贾东辉, 等. 不同来源皮瓣对近端尿道下裂修补术预后的影响[J]. 中国男科学杂志, 2013, 27(6): 27-29, 34. Zhang WX, Song XH, Jia DH, et al. Effects of different flaps and preservation of urethral plate on postoperative complication rate after proximal hypospadias repair[J]. Chin J Androl, 2013, 27(6): 27-29, 34. DOI:10.3969/j.issn.1008-0848.2013.06.006 |
| [46] |
Zheng DC, Wang H, Lu MJ, et al. A comparative study of the use of a transverse preputial island flap(the Duckett technique)to treat primary and secondary hypospadias in older Chinese patients with severe chordee[J]. World J Urol, 2013, 31(4): 965-969. DOI:10.1007/s00345-012-0990-2 |
| [47] |
Titley OG, Bracka A. A 5-year audit of trainees experience and outcomes with two-stage hypospadias surgery[J]. Br J Plast Surg, 1998, 51(5): 370-375. DOI:10.1054/bjps.1997.0157 |
| [48] |
Vallasciani S, Berrettini A, Nanni L, et al. Observational retrospective study on acquired megalourethra after primary proximal hypospadias repair and its recurrence after tapering[J]. J Pediatr Urol, 2013, 9(3): 364-367. DOI:10.1016/j.jpurol.2012.05.005 |
| [49] |
Shukla AR, Patel RP, Canning DA. The 2-stage hypospadias repair.Is it a misnomer?[J]. J Urol, 2004, 172(4 Pt 2): 1714-1716. DOI:10.1097/01.ju.0000138926.26530.f9 |
| [50] |
Leslie B, Lorenzo AJ, Figueroa V, et al. Critical outcome analysis of staged buccal mucosa graft urethroplasty for prior failed hypospadias repair in children[J]. J Urol, 2011, 185(3): 1077-1082. DOI:10.1016/j.juro.2010.10.047 |
| [51] |
Castagnetti M, El-Ghoneimi A. Surgical management of primary severe hypospadias in children: systematic 20-year review[J]. J Urol, 2010, 184(4): 1469-1474. DOI:10.1016/j.juro.2010.06.044 |
| [52] |
Wu YH, Wang JK, Zhao TX, et al. Complications following primary repair of non-proximal hypospadias in children: a systematic review and meta-analysis[J]. Front Pediatr, 2020, 8: 579364. DOI:10.3389/fped.2020.579364 |
| [53] |
韩文文, 张潍平, 孙宁, 等. 小儿泌尿外科医师尿道下裂学习曲线探讨[J]. 继续医学教育, 2016, 30(3): 51-52. Han WW, Zhang WP, Sun N, et al. Exploring the learning curve of hypospadias for pediatric urologists[J]. Contin Med Educ, 2016, 30(3): 51-52. DOI:10.3969/j.issn.1004-6763.2016.03.032 |
| [54] |
Castagnetti M, Zhapa E, Rigamonti W. Primary severe hypospadias: comparison of reoperation rates and parental perception of urinary symptoms and cosmetic outcomes among 4 repairs[J]. J Urol, 2013, 189(4): 1508-1513. DOI:10.1016/j.juro.2012.11.013 |
| [55] |
Rynja SP, de Jong TPVM, Bosch JLHR, et al. Proximal hypospadias treated with a transverse preputial island tube: long-term functional, sexual, and cosmetic outcomes[J]. BJU Int, 2018, 122(3): 463-471. DOI:10.1111/bju.14234 |
 2023, Vol. 22
2023, Vol. 22


