2. 南京医科大学附属儿童医院消化科,南京 210008
2. Department of Gastroenterology, Children's Hospital of Nanjing Medical University, Nanjing 210008, China
据不完全统计,儿童便秘的发病率为0.7% ~30%[1-2]。小儿结肠冗长症以难治性便秘为主要临床表现。难治性便秘表现为排便次数减少、排便困难、大便失禁和腹痛,显著影响患儿生长发育。小儿结肠冗长症在灌肠造影检查中可见结肠冗长,这既是功能性问题,也是器质性问题[3]。难治性便秘伴结肠冗长患儿的症状可迁延至成人阶段,严重影响患儿生活质量,也给患儿家庭带来极大负担[4-5]。因此,结肠冗长症的研究对难治性便秘患儿具有重要意义。本文对以难治性便秘为主要表现的儿童结肠冗长症的评估、检查及诊治进展进行综述。
一、概述难治性便秘患儿常并发结肠冗长症,出现长期便秘和大量粪便潴留,造成肠道蠕动障碍,灌肠造影检查提示结肠直径变宽、长度拉长[6-7]。结肠测压检查显示结肠冗长患儿有过早终止的高振幅传播收缩,提示可能存在结肠运动障碍[8]。El-Sonbaty等[6]将结肠冗长作为难治性便秘的手术指征,Koppen等[9]研究发现结肠冗长程度与泻药的使用量有关。
二、结肠冗长症及其判定标准部分难治性便秘患儿存在器质性病变,可通过灌肠造影检查发现异常的结肠解剖结构,并评价结肠的定位与形态变化[10]。成人结肠冗长的判定标准为结肠任一肠段长度超过标准长度的35% ~40%,且活动范围变化大(横结肠活动超过髂棘,乙状结肠活动范围达右上腹或右下腹)[11]。也可根据发病部位进行分型,Ⅰ型为单结肠病变,Ⅱ型为二段结肠病变,Ⅲ型则为三段、四段结肠冗长[12]。目前儿童结肠冗长症的诊断标准尚有争议,小儿仅需满足乙状结肠长度达40~60 cm即可诊断为乙状结肠冗长,但无结肠直径的相关标准[13]。Koppen等[14]针对6岁以下健康儿童进行结肠测量,将结肠段直径/第二腰椎宽度的比值作为结肠相对长度,发现正常儿童结肠相对长度与年龄无显著相关性;而与正常儿童比较,难治性便秘患儿的乙状结肠直径增宽,直肠乙状结肠和降结肠的长度明显变长[9]。
三、结肠冗长症的辅助检查 (一) 结肠传输试验结肠传输试验的目的在于测量粪便在结肠中通过的速度,测定肠道各段传输时间,评估其运动及排空能力是否正常[15]。结肠传输试验可为便秘分型及胃肠动力异常提供诊断依据,通过X线标记与核素扫描,将难治性便秘进一步分为正常传输型便秘、慢传输型便秘及出口梗阻型便秘[16]。Wood等[7]研究发现,结肠冗长患儿的横结肠与乙状结肠形态曲折,且其长度较正常患儿增长30%以上。此外,Raahave等[8]研究发现结肠冗长患儿与对照组平均结肠传输时间存在显著差异。在结肠传输试验提示为慢传输便秘的患儿中,大多数患儿在接受次全结肠切除术后证实存在结肠冗长。该试验中排空时间的延长,提示结肠慢传输障碍与结肠冗长有关。
(二) 肛门直肠测压(anorectal manometry, ARM)ARM是儿童最常用的动力试验。欧洲和北美儿科胃肠病、肝病和营养学会共识将ARM列为难治性便秘患儿需要进行的检查之一。ARM可评估肛门括约肌压力、直肠肛门感觉反应以及排便的协调性。借由ARM检测直肠肛门抑制反射(rectal anal inhibitory reflex, RAIR)情况,提示患儿是否有正常的感觉阈值和排便冲动[17]。在乙状结肠冗长患儿的ARM检查中,RAIR正常存在,但其表现为波幅宽大的W波,且直肠静息压低,肛管静息压以及肛管高压区的长度值明显升高[18]。对于成人结肠冗长患者,O'Dwyer等[19]发现可出现直肠顺应性增加以及肛管超慢波发生率较高的现象。而Wu等[20]指出在先天性巨结肠患者中,85%存在RAIR,且同时有肛门静息压和直肠静息压的升高。另外,慢传输型便秘ARM发生肛管最大收缩压不足的概率较高[21]。由此可见,ARM在疾病鉴别诊断中具有重要作用。在结肠冗长症患者中,RAIR虽存在,但ARM的波形特征与正常表现不同,提示可能存在结肠动力异常。
(三) 结肠测压(colonic manometry, CM)作为诊断难治性便秘的推荐方法之一,CM可实时监测肠腔内的压力变化,以评估患儿的肠蠕动和肠收缩能力,确认有无潜在的神经肌肉异常[2]。
结肠测压可帮助识别不同的结肠运动模式,包括孤立性收缩、传播性收缩、高振幅传播收缩(high amplitude propagating contractions, HAPCs)、同步收缩、逆行性收缩以及周期性结直肠动力活动等[22]。其中HAPCs对粪便运输和排便起到重要作用,被认为是正常结肠运动的重要组成[23]。Koppen等[9]研究发现,结肠冗长患儿的结肠测压结果中,HAPCs表现为过早终止。而过早终止的HAPCs对应的结肠段直径显著大于正常HAPCs的结肠段直径,提示结肠扩张与运动障碍有关。因此,如果CM发现过早终止的HAPCs,则提示患儿可能患有结肠冗长症。虽然过早终止的HAPCs表明结肠存在运动障碍,但在研究中仍可观察到这部分结肠段的收缩。这间接说明其部分神经和肌肉网络仍存在一定的正常功能[8]。在Gupta等[24]研究中,大多数患儿会在手术前进行CM,以有效识别并定位存在运动障碍的结肠段。患者可透过CM区分其病变部位为左侧结肠功能障碍还是全结肠功能障碍,辅助医生确定病因并进行相应治疗,因此CM已成为诊断以难治性便秘为主要表现的结肠冗长患儿的重要手段。
(四) 结肠组织病理学肠道活动主要受到消化道平滑肌、肠神经系统和胃肠道慢波电位起搏细胞中的Cajal间质细胞(interstitial cells of Cajal, ICC)调节。首先,结果正常的平滑肌层是肠道有效蠕动的先决条件。O'Dwyer等[19]指出,冗长结肠的平滑肌细胞会出现萎缩、变性,使其无法正常收缩,从而导致结肠扩张。第二,肠神经系统在肠道功能调节中同样发挥重要作用。在成人特发性巨结肠患者中,黏膜下层和肌间神经丛的神经节细胞虽形态正常,但数量有所减少[25];也有相似研究提及神经胶质细胞的数量有明显减少趋势,说明肠神经系统的异常与便秘有关。第三,ICC会产生慢波活动,参与肠道神经传递,调节脑肠轴功能[26]。Cuda等[27]研究发现,冗长段的ICC数量减少、密度降低和细胞形态异常,提示ICC的异常与难治性便秘相关结肠冗长症的发病相关。上述研究提示肠道肌肉、神经、间质病变因素均与肠动力障碍有关[28]。
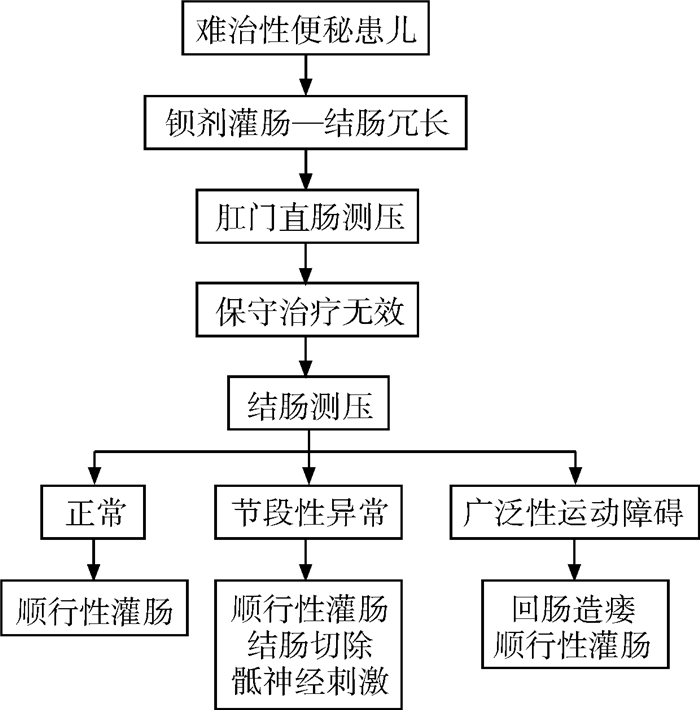
四、难治性便秘相关结肠冗长症的治疗进展不完全代偿期和失代偿期儿童结肠冗长症的主要表现是病程较长且症状较重的难治性便秘[29]。灌肠造影和结肠测压法可帮助识别肠道形态异常和运动障碍,以评估病情严重程度。当长期保守治疗无效时,需采取个体化综合治疗(图 1)[30]。
|
图 1 以难治性便秘为表现的儿童结肠冗长症的诊治流程 Fig.1 Diagnosis and treatment of intractable constipation due to redundant colon in children |
ACE即经盲肠和Malone阑尾造瘘口行顺行性结肠冲洗[31]。Dolejs等[32]发现难治性便秘患者行ACE治疗后,肠道功能有所好转且蠕动恢复正常;后期随访中约有43%的患者在停止ACE治疗后未再出现反复便秘。由此推断结肠运动障碍可能是由于长期便秘、粪便潴留导致。经结肠减压及结肠冲洗后,结肠运动障碍是可逆的[33]。
(二) 骶神经刺激(sacral nerve stimulation, SNS)SNS是通过臀部皮下植入神经刺激的装置,将导线伸入骶骨孔中,进而刺激第3、4骶神经,调节肠神经系统。Vriesman等[34]研究发现SNS可显著改善难治性便秘合并粪便失禁患儿的症状。
(三) 外科手术部分难治性便秘患儿经长期保守治疗后,症状持续不缓解且病情较严重,对生活质量造成很大影响,需考虑进行手术干预。评估难治性便秘相关结肠冗长症患儿是否需要手术治疗,需从以下几个方面考量:①有功能性便秘表现;②肠道管理计划失败;③灌肠造影检查提示结肠冗长;④排便造影显示大便排空不良(50%)和对比不良;⑤ARM显示直肠僵硬且顺应性差[35]。根治性手术包括结肠切除回肠储袋吻合术、Duhamel术、经肛门Soave和Swenson术、Soave-George腹腔镜手术以及乙状结肠切除术[36]。治疗结肠冗长最常用的手术方式为病变扩张肠段行节段性结肠切除术[37]。Cheng等[4]指出,对于直肠、乙状结肠冗长患儿,行节段性结肠切除术预后良好。刘永东等[1]研究发现,14例乙状结肠冗长患儿行Soave术后,难治性便秘情况好转且恢复正常排便,预后良好。而在成人患者中,次全结肠切除加回肠直肠吻合术最常见[38]。但此术式在难治性便秘患儿中预后欠佳,约30%的患儿手术后出现大便失禁,因此较少见于儿童结肠冗长症的手术方案中[39]。Kuizenga-Wessel等[40]随访了114例经外科手术治疗的难治性便秘患儿,其父母对手术治疗的满意度达91%,提示外科干预能显著改善患儿病情。
综上所述,以难治性便秘为表现的结肠冗长患儿,会出现长期便秘和大量粪便潴留,从而造成肠道功能受损。灌肠造影可判断结肠定位及异常形态,诊断结肠冗长症。结肠传输试验、组织病理学检查和肠道测压可帮助识别运动障碍并进行评估,指导诊疗决策。目前以难治性便秘为表现的结肠冗长症的治疗包括ACE、SNS和外科手术等。通过辅助检查手段早期发现、早期诊断有助于对整体肠道的综合评估及决定治疗策略,这对于以难治性便秘为主要表现的儿童结肠冗长症具有重要意义。
利益冲突 所有作者声明不存在利益冲突
作者贡献声明 黄怡璇负责文献收集、分析和起草文章;刘志峰负责研究设计与酝酿,并对文章知识性内容进行审阅
| [1] |
刘永东, 胡强, 李俊峰, 等. 14例小儿乙状结肠冗长症手术治疗分析[J]. 临床小儿外科杂志, 2015, 14(4): 345-346. Liu YD, Hu Q, Li JF, et al. Analyses of surgical treatment of 14 cases of dolichosigmoid in children[J]. J Clin Ped Sur, 2015, 14(4): 345-346. DOI:10.3969/j.issn.1671-6353.2015.04.029 |
| [2] |
Koppen IJN, Kuizenga-Wessel S, Lu PL, et al. Surgical decision-making in the management of children with intractable functional constipation: what are we doing and are we doing it right?[J]. J Pediatr Surg, 2016, 51(10): 1607-1612. DOI:10.1016/j.jpedsurg.2016.05.023 |
| [3] |
Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN[J]. J Pediatr Gastroenterol Nutr, 2014, 58(2): 258-274. DOI:10.1097/MPG.0000000000000266 |
| [4] |
Cheng LS, Goldstein AM. Surgical management of idiopathic constipation in pediatric patients[J]. Clin Colon Rectal Surg, 2018, 31(2): 89-98. DOI:10.1055/s-0037-1609023 |
| [5] |
Paknejad MS, Motaharifard MS, Barimani S, et al. Traditional, complementary and alternative medicine in children constipation: a systematic review[J]. Daru, 2019, 27(2): 811-826. DOI:10.1007/s40199-019-00297-w |
| [6] |
El-Sonbaty MM, Fathy A, Aljohani A, et al. Assessment of behavioural disorders in children with functional constipation[J]. Open Access Maced J Med Sci, 2019, 7(23): 4019-4022. DOI:10.3889/oamjms.2019.677 |
| [7] |
Wood RJ, Yacob D, Levitt MA. Surgical options for the management of severe functional constipation in children[J]. Curr Opin Pediatr, 2016, 28(3): 370-379. DOI:10.1097/MOP.0000000000000345 |
| [8] |
Raahave D. Dolichocolon revisited: an inborn anatomic variant with redundancies causing constipation and volvulus[J]. World J Gastrointest Surg, 2018, 10(2): 6-12. DOI:10.4240/wjgs.v10.i2.6 |
| [9] |
Koppen IJN, Thompson BP, Ambeba EJ, et al. Segmental colonic dilation is associated with premature termination of high-amplitude propagating contractions in children with intractable functional constipation[J]. Neurogastroenterol Motil, 2017, 29(10): 1-9. DOI:10.1111/nmo.13110 |
| [10] |
Radwan AB, El-Debeiky MS, Abdel-Hay S. Contrast enema as a guide for senna-based laxatives in managing overflow retentive stool incontinence in pediatrics[J]. Pediatr Surg Int, 2015, 31(8): 765-771. DOI:10.1007/s00383-015-3741-9 |
| [11] |
黄国强, 魏小巍. 结肠冗长症研究现状及治疗新进展[J]. 世界最新医学信息文摘, 2017, 17(40): 44, 46. Huang GQ, Wei XW. Current research status and new treatment progress of redundant colon[J]. World Latest Med Inf, 2017, 17(40): 44, 46. |
| [12] |
胡波, 张开晓. 外科治疗结肠冗长症的心得体会[J]. 世界最新医学信息文摘, 2019, 19(45): 317, 320. Hu B, Zhang KX. Surgical experiences of redundant colon[J]. World Latest Med Inf, 2019, 19(45): 317, 320. DOI:10.19613/j.cnki.1671-3141.2019.45.227 |
| [13] |
许芝林, 王强, 李琰, 等. 乙状结肠冗长症的术式选择探讨[J]. 临床小儿外科杂志, 2010, 9(6): 432-434. Xu ZL, Wang Q, Li Y, et al. Selecting surgical approaches for dolichosigmoid[J]. J Clin Ped Sur, 2010, 9(6): 432-434. DOI:10.3969/j.issn.1671-6353.2010.06.010 |
| [14] |
Koppen IJN, Yacob D, Di Lorenzo C, et al. Assessing colonic anatomy normal values based on air contrast enemas in children younger than 6 years[J]. Pediatr Radiol, 2017, 47(3): 306-312. DOI:10.1007/s00247-016-3746-0 |
| [15] |
Li YW, Yu YJ, Fei F, et al. High-resolution colonic manometry and its clinical application in patients with colonic dysmotility: a review[J]. World J Clin Cases, 2019, 7(18): 2675-2686. DOI:10.12998/wjcc.v7.i18.2675 |
| [16] |
Hutson JM, Hynes MC, Kearsey I, et al. 'Rapid transit' constipation in children: a possible genesis for irritable bowel syndrome[J]. Pediatr Surg Int, 2020, 36(1): 11-19. DOI:10.1007/s00383-019-04587-x |
| [17] |
Benninga MA, Faure C, Hyman PE, et al. Childhood functional gastrointestinal disorders: neonate/toddler[J]. Gastroenterology, 2006, 150(6): 1443-1455.E2. DOI:10.1053/j.gastro.2016.02.016 |
| [18] |
苗绘, 许芝林, 任冬晗, 等. 单纯乙状结肠冗长症患儿术前及术后的肛门直肠测压分析[J]. 中华临床医师杂志(电子版), 2011, 5(21): 6463-6465. Miao H, Xu ZL, Ren DH, et al. Analysis of anorectal manometry before and after surgery in children with dolichosigmoid[J]. Chin J Clin (Electron Ed), 2011, 5(21): 6463-6465. DOI:10.3877/cma.j.issn.1674-0785.2011.21.051 |
| [19] |
O'Dwyer RH, Acosta A, Camilleri M, et al. Clinical features and colonic motor disturbances in chronic megacolon in adults[J]. Dig Dis Sci, 2015, 60(8): 2398-2407. DOI:10.1007/s10620-015-3645-5 |
| [20] |
Wu XJ, Zhang HY, Li N, et al. A new diagnostic scoring system to differentiate Hirschsprung's disease from Hirschsprung's disease-allied disorders in patients with suspected intestinal dysganglionosis[J]. Int J Colorectal Dis, 2013, 28(5): 689-696. DOI:10.1007/s00384-013-1691-z |
| [21] |
Andromanakos NP, Pinis SI, Kostakis AI. Chronic severe constipation: current pathophysiological aspects, new diagnostic approaches, and therapeutic options[J]. Eur J Gastroenterol Hepatol, 2015, 27(3): 204-214. DOI:10.1097/MEG.0000000000000288 |
| [22] |
Wessel S, Koppen IJN, Wiklendt L, et al. Characterizing colonic motility in children with chronic intractable constipation: a look beyond high-amplitude propagating sequences[J]. Neurogastroenterol Motil, 2016, 28(5): 743-757. DOI:10.1111/nmo.12771 |
| [23] |
Corsetti M, Costa M, Bassotti G, et al. First translational consensus on terminology and definitions of colonic motility in animals and humans studied by manometric and other techniques[J]. Nat Rev Gastroenterol Hepatol, 2019, 16(9): 559-579. DOI:10.1038/s41575-019-0167-1 |
| [24] |
Gupta A, Basson S, Borrelli O, et al. Surgically treated intractable constipation in children evaluated with colonic manometry[J]. J Pediatr Surg, 2020, 55(2): 265-268. DOI:10.1016/j.jpedsurg.2019.10.046 |
| [25] |
Ohkubo H, Masaki T, Matsuhashi N, et al. Histopathologic findings in patients with idiopathic megacolon: a comparison between dilated and non-dilated loops[J]. Neurogastroenterol Motil, 2014, 26(4): 571-580. DOI:10.1111/nmo.12303 |
| [26] |
Wang XJ, Camilleri M. Chronic megacolon presenting in adolescents or adults: clinical manifestations, diagnosis, and genetic associations[J]. Dig Dis Sci, 2019, 64(10): 2750-2756. DOI:10.1007/s10620-019-05605-7 |
| [27] |
Cuda T, Gunnarsson R, De Costa A. Symptoms and diagnostic criteria of acquired megacolon-a systematic literature review[J]. BMC Gastroenterol, 2018, 18(1): 25. DOI:10.1186/s12876-018-0753-7 |
| [28] |
Keller J, Bassotti G, Clarke J, et al. Expert consensus document: advances in the diagnosis and classification of gastric and intestinal motility disorders[J]. Nat Rev Gastroenterol Hepatol, 2018, 15(5): 291-308. DOI:10.1038/nrgastro.2018.7 |
| [29] |
陶桢, 蒋学武, 李建宏. 小儿乙状结肠冗长症21例诊治分析[J]. 临床小儿外科杂志, 2006, 5(5): 328-330. Tao Z, Jiang XW, Li JH. Clinical analyses of diagnosing and treating 21 cases of dolichosigmoid in children[J]. J Clin Ped Sur, 2006, 5(5): 328-330. DOI:10.3969/j.issn.1671-6353.2006.05.003 |
| [30] |
Rodriguez L, Sood M, Di Lorenzo C, et al. An ANMS-NASPGHAN consensus document on anorectal and colonic manometry in children[J]. Neurogastroenterol Motil, 2017, 29(1): e12944. DOI:10.1111/nmo.12944 |
| [31] |
Halleran DR, Vilanova-Sanchez A, Rentea RM, et al. A comparison of Malone appendicostomy and cecostomy for antegrade access as adjuncts to a bowel management program for patients with functional constipation or fecal incontinence[J]. J Pediatr Surg, 2019, 54(1): 123-128. DOI:10.1016/j.jpedsurg.2018.10.008 |
| [32] |
Dolejs SC, Smith JK, Jr, Sheplock J, et al. Contemporary short- and long-term outcomes in patients with unremitting constipation and fecal incontinence treated with an antegrade continence enema[J]. J Pediatr Surg, 2017, 52(1): 79-83. DOI:10.1016/j.jpedsurg.2016.10.022 |
| [33] |
Chong C, Featherstone N, Sharif S, et al. 5 years after an ACE: what happens then?[J]. Pediatr Surg Int, 2016, 32(4): 397-401. DOI:10.1007/s00383-016-3857-6 |
| [34] |
Vriesman MH, Wang L, Park C, et al. Comparison of antegrade continence enema treatment and sacral nerve stimulation for children with severe functional constipation and fecal incontinence[J]. Neurogastroenterol Motil, 2020, 32(8): e13809. DOI:10.1111/nmo.13809 |
| [35] |
Glasser JG, Nottingham JM, Durkin M, et al. Case series with literature review: surgical approach to megarectum and/or megasigmoid in children with unremitting constipation[J]. Ann Med Surg (Lond), 2018, 26: 24-29. DOI:10.1016/j.amsu.2017.12.009 |
| [36] |
Rodriguez L, Heinz N, Nurko S. Utility of colon manometry in guiding therapy and predicting need for surgery in children with defecation disorders[J]. J Pediatr Gastroenterol Nutr, 2020, 70(2): 232-237. DOI:10.1097/MPG.0000000000002504 |
| [37] |
Siminas S, Losty PD. Current surgical management of pediatric idiopathic constipation: a systematic review of published studies[J]. Ann Surg, 2015, 262(6): 925-933. DOI:10.1097/SLA.0000000000001191 |
| [38] |
Cuda T, Gunnarsson R, De Costa A. The correlation between diverticulosis and redundant colon[J]. Int J Colorectal Dis, 2017, 32(11): 1603-1607. DOI:10.1007/s00384-017-2894-5 |
| [39] |
Kerur B, Kantekure K, Bonilla S, et al. Management of chronic intractable constipation in children[J]. J Pediatr Gastroenterol Nutr, 2014, 59(6): 754-757. DOI:10.1097/MPG.0000000000000535 |
| [40] |
Kuizenga-Wessel S, Koppen IJN, Zwager LW, et al. Surgical management of children with intractable functional constipation; experience of a single tertiary children's hospital[J]. Neurogastroenterol Motil, 2017, 29(5): e13005. DOI:10.1111/nmo.13005 |
 2022, Vol. 21
2022, Vol. 21


