2. 青岛大学附属妇女儿童医院(山东省青岛市, 266000)
2. Affiliated Women and Children's Hospital of Qingdao University, Qingdao 266000, China
精索静脉曲张(varicocele, VC)是儿童及青少年的常见病,也是男性不育的病因之一,尤其对于睾丸正在发育的青少年来说影响更甚。随着腹腔镜技术的发展,微创化、精准化治疗已经成为小儿外科未来发展的趋势[1]。腹腔镜微创技术手段不断进步、革新,由传统的多孔到现在的单孔腔镜手术,使得疾病的治疗越来越精准化、微创化[2]。因此对于青少年VC的治疗,不单需要考虑如何治疗疾病,还需要考虑如何将手术做到精准化、微创化以及减少术后并发症。为了减少VC术后复发、继发性鞘膜积液等并发症的发生,新的手术方式正不断探索并应用于临床。本中心在保留淋巴管的前提下,通过改进Palomo术式使用经脐单孔腹腔镜下淋巴管显影治疗VC,并取得良好效果,现报道如下。
材料与方法 一、临床资料选取2016年7月至2019年10月由青岛大学附属医院收治的精索静脉曲张患者15例作为研究对象,年龄11~14岁,平均年龄(12.67±1.03)岁,患侧均为左侧,其中3例以阴囊坠痛感就诊(3例皆为Ⅱ级),12例以阴囊肿物就诊(1例为Ⅱ级,11例为Ⅲ级)。精索静脉曲张Ⅲ级11例,Ⅱ级4例。4例Ⅱ级患者随访6个月,阴囊肿物未缩小,阴囊不适感未缓解。所有患者行泌尿系统B超检查,提示精索内静脉内径增粗,精索静脉曲张,精索静脉内径直径为2.40~4.80 mm,平均为(3.37±0.67)mm,见表 1。纳入标准:年龄11~14岁;左侧精索静脉曲张Ⅱ~Ⅲ度;原发性精索静脉曲张,无胡桃夹综合征;有明显的临床症状,阴囊坠涨感;术前均行B超进一步确诊,精索静脉血管内径均>2.0 mm,行乏式动作后,反流现象为阳性;手术由同一副主任医师主刀完成。
| 表 1 15例VC患者年龄、睾丸变化、临床表现、术后并发症 Table 1 Age, testicular changes, clinical manifestations and postoperative complications of 15VC |
|
|
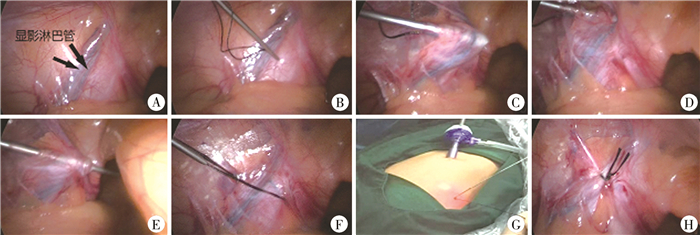
所有患者采用气管插管全身麻醉,取自然腔道脐部为切口,切口约1 cm,沿脐部正中纵行切开,钝性分离,置入10 mm Trocar,建立气腹,压力维持在8~10 mmHg,经Trocar进入监视镜头,探查见左侧精索静脉曲张、增粗。经左侧睾丸鞘膜腔内注射亚甲蓝3 mL,约60 s即可发现患者左侧精索静脉伴行的淋巴管显影。此时可通过拉近腹腔镜镜头,可清晰地看到显影的淋巴管(图 1A)。取左下腹腹横纹处2 mm精索血管束体表投影处,将带线疝针经左下腹壁穿入至腹膜外(图 1B)。通过疝针游离精索血管术内淋巴管,此时可以先将疝针从精索血管束于接近内环口处下方穿过,然后挑起血管束(图 1C)。进一步通过疝针挑开显影淋巴管将其压在疝针下方(图 1D),然后穿出带线疝针(图 1E)。至少保留1根淋巴管,然后穿出带线疝针,将疝针钩针拉起线环带出(图 1F),由于精索血管有一定弹性,可将其拉出体外进行打结(图 1G),将线结打紧。打结时避免夹杂皮下脂肪等组织,将线结送回腹腔后(图 1H),缝合脐部切口。
|
图 1 精索静脉曲张患者手术过程图 注 A:显影淋巴管;B:带线疝针经皮穿入腹腔;C:疝针将精索血管束挑起;D:疝针将显影淋巴管挑开压在下方;E:带线疝针穿出;F:将带线疝针带出体外;G:体外打结; H:将线结送回腹腔 Fig.1 Operation diagram of varicocele A: Displayed lymphangion; B: Guiding a hernia needle percutaneously into abdominal cavity; C: Hernia needle lifted spermatic cord bundle; D: Hernia needle pushed down visualized lymphatic vessels; E: Retracting hernia needle with thread; F: Threading hernia needle out of body; G: Knotting in vitro; H: Returning the knot back into abdominal cavity |
采用SPSS20.0进行统计学分析,对于服从正态分布计量资料采用均数加减标准差(x±s)表示,手术前后患者睾丸体积差值的变化采用配对样本t检验,以P<0.05为差异有统计学意义。
结果所有患者淋巴管成功显影,均至少保留1根淋巴管,从注射到显影时间为30~90 s,平均(60.40±20.03)s。手术时间33~60 min,平均(40.13±11.25)min。患者住院时间1~6 d,平均(3.40±1.40)d,阴囊蓝染消失时间3~7 d,平均(4.40±1.45)d。所有患者获得随访,术后随访6~18个月,发现阴囊肿物缩小,阴囊坠痛获得改善,术后患者双侧睾丸均有不同程度增长(P < 0.001),且左侧睾丸体积增长为(1.68±0.52)mm3,大于右侧(1.58±0.44)mm3,但差异无统计学意义(t=0.577,P=0.573)。无精索静脉曲张的复发,无鞘膜积液、阴囊水肿、阴囊色素沉积发生。
讨论VC可导致睾丸发育障碍,是导致男性不育的原因之一,青少年是VC的高发人群,据赵斌等[3]报道,我国6~19岁青少年发病率为10.76%,可能与该时期患者生殖系统的快速发育、睾丸血流增加有关。
VC以手术治疗为主,手术方法包括传统开放手术、腹腔镜手术、显微外科手术以及介入手术,腹腔镜术式包括保留精索内动脉的Ivanissevich术式和精索内血管高位结扎Palomo术。前者虽保留精索内动脉但会遗漏小静脉或误扎精索内淋巴管,可能会增加术后鞘膜积液的发生率;后者高位结扎精索血管束,不保留淋巴管,也同样增加术后并发鞘膜积液的概率。Kamal等[4]研究发现Palomo术继发性鞘膜积液的发生率为8.24%,而Ivanissevich术为7.3%。为了避免术后并发鞘膜积液,本研究进一步改良Palomo术式(通过术中亚甲蓝鞘膜腔内注射显影淋巴管并保留淋巴管的手术方式)[5, 6]。在乳腺癌根治术中应用亚甲蓝显影哨兵淋巴结的技术已相当成熟,其安全性及适用性已得到广泛证实[7]。Goldstein等[8]报道利用显微外科技术结合亚甲蓝染色协助辨别主要淋巴管,认为利用该法辨别并保留淋巴管可明显减少睾丸鞘膜积液等并发症的发生。因此,本研究选择了亚甲蓝作为精索内淋巴管显影的染料。丁强红等[9]与刘颖等[10]研究则选择鞘膜腔内注射,而潘爱民等[11]研究在进行亚甲蓝注射时,为了提高显影成功率及加快显影速度,选择了睾丸内注射。Makari等[12]通过小鼠实验在睾丸内注射染料,发现即使睾丸内注射生理盐水也会使睾丸产生病理性变化。而青少年睾丸正处于迅速发育期,为避免睾丸内注射亚甲蓝对患者睾丸发育产生影响,故本研究选择与丁强红等[10]和刘颖等[11]研究相同的注射部位,即鞘膜腔内注射亚甲蓝。本研究发现鞘膜腔内注射亚甲蓝,淋巴管显影率也能得到保证。本研究中所有患者淋巴管显影获得成功。
在注射亚甲蓝时拉紧患侧睾丸皮肤,使用5 mL空针抽取3 mL亚甲蓝,向近心端倾斜30°经患侧阴囊皮肤于睾丸上方处注射进入鞘膜腔。在手术过程中需注意以下几点:第一,切勿进针过深,否则可能会使淋巴管显影失败[10]。第二,注射亚甲蓝之后可轻柔挤压患侧阴囊,使亚甲蓝充分通过淋巴回流。第三,待淋巴管充分后显影后,疝针经精索血管束体表投影位置经皮穿入腹腔,通过疝针游离精索血管束时,此时可拉近镜头,同时用疝针将精索挑起,这样可更加清晰地观察显影的淋巴管,将显影淋巴管压到疝针下方,穿出疝针,避开显影淋巴管的同时结扎精索血管束。第四,手术过程中应尽可能多保留淋巴管。
青少年采集精液的依从性低于成人,且此时期睾丸一直处于生长发育的过程中,故本研究选择睾丸体积来测定VC患者睾丸发育情况[13]。本研究显示术后患者睾丸体积明显增大,且无鞘膜积液发生,说明单孔腹腔镜保留淋巴管治疗青少年VC可改善患侧睾丸发育,同时可降低术后鞘膜积液发生率[14]。但关于术后患者生育情况需待患者成年后进一步随访。患者术后阴囊会发生蓝染,一般会在7 d内自然吸收。
与多孔不保留淋巴管和多孔保留淋巴管两种术式相比,经脐单孔腹腔镜下淋巴管显影治疗VC,减少了术后并发鞘膜积液、阴囊水肿的风险,缩短了手术时间,同时由于Trocar孔经由脐部,术后瘢痕更加隐蔽[15-17]。疝针穿刺无需缝合,术后恢复快。因此,应用亚甲蓝单孔腹腔镜保留淋巴管治疗青少年VC,使精索内淋巴管显影,同时保留淋巴管,对降低术后鞘膜积液的发生率有一定作用。但本研究样本量较小,随访时间不足,患者生育情况需待成年后进一步随访,缺少对照,还需进一步积累病例,并长期随访。
| [1] |
李龙, 张金哲. 精准微创技术是现代小儿外科发展的新阶段[J]. 中国微创外科杂志, 2011, 11(2): 97-100. Li L, Zhang JZ. Accurate and mini-invasive technology is a new stage in the development of modern pediatric surgery[J]. Chinese Journal of Minimally Invasive Surgery, 2011, 11(2): 97-100. DOI:10.3969/j.issn.1009-6604.2011.02.001 |
| [2] |
关小明, 张意茗, 范晓东. 单孔腹腔镜技术的发展及展望[J]. 山东大学学报(医学版), 2019, 57(12): 5-9. Guan XM, Zhang YM, Fang XD. Developments and future prospects of laparoendoscopic single-site surgery[J]. Journal of Shandong University (Health Sciences), 2019, 57(12): 5-9. DOI:10.6040/j.issn.1671-7554.0.2019.1104 |
| [3] |
赵斌, 吴荣德, 于启海, 等. 儿童精索静脉曲张患病情况的调查[J]. 中华小儿外科杂志, 2005, 26(3): 132-134. Zhao B, Wu RD, Yu QH, et al. The prevalence of varicocele in children of Shandong Province[J]. Chin J Pediatr Surg, 2005, 26(3): 132-134. DOI:10.3760/cma.j.issn.0253-3006.2005.03.007 |
| [4] |
Hosseini K, Nejatifar M, Kabir A. Comparison of the efficacy and safety of palomo, ivanissevich and laparoscopic varicocelectomy in iranian infertile men with palpable varicocele[J]. Int J Fertil Steril, 2018, 12(1): 81-87. DOI:10.22074/ijfs.2018.5158 |
| [5] |
Esposito C, Turrà F, Del Conte F, et al. indocyanine green fluorescence lymphography: a new technique to perform lymphatic sparing laparoscopic palomo varicocelectomy in children[J]. J Laparoendosc Adv Surg Tech A, 2019, 29(4): 564-567. DOI:10.1089/lap.2018.0624 |
| [6] |
杨林. Eur Urol: 儿童及青少年精索静脉曲张的治疗——来自欧洲泌尿外科学会/欧洲小儿泌尿外科学会指南专家组的系统综述及Meta分析[J]. 现代泌尿外科杂志, 2019, 24(4): 314. Yang L. Eur Urol: Treatment of varicocele in children and adolescents: a systematic review and meta-analysis from the European Urological Society/European Urological Society of Paediatric Urology Guidelines Expert group[J]. Journal of Modern Urology, 2019, 24(4): 314. DOI:10.3969/j.issn.1009-8291.2019.04.016 |
| [7] |
贾卫娟, 苏逢锡, 陈积圣. 乳腺癌哨兵淋巴结活检126例的临床研究[J]. 中华普通外科杂志, 2003, 18(3): 133-135. Jia WJ, Su FX, Chen JS. Sentinel lymph node biopsy for breast cancer: a report of 126 cases[J]. Chinese Journal of General Surgery, 2003, 18(3): 133-135. DOI:10.3760/j.issn:1007-631X.2003.03.001 |
| [8] |
Goldstein M, Gilbert BR, Dicker AP, et al. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique[J]. J Urol, 1992, 148(6): 1808-1811. DOI:10.1089/end.1992.6.463 |
| [9] |
丁强红, 刘涛, 何灼彬, 等. 腹腔镜下淋巴管保留在精索静脉高位结扎术中的应用[J]. 中华腔镜泌尿外科杂志(电子版), 2017, 9(6): 55-58. Ding QH, Liu T, He ZB, et al. Clinical application of lymphatic-sparing laparoscopic varicocelectomy[J]. Chinese Journal of Endourology(Electronic Version), 2017, 9(2): 28-30. DOI:10.3969/j.issn.1674-7410.2017.02.010 |
| [10] |
刘颖, 毕允力, 陆良生, 等. 保留淋巴管的腹腔镜精索静脉高位结扎术12例治疗体会[J]. 中华小儿外科杂志, 2017, 38(6): 416-419. Liu Y, Bi YL, Lu LS, et al. Laparoscopic high-ligation of spermatic vein with lymphatic retention for varicocele: a report of 12 cases[J]. Chin J Pediatr Surg, 2017, 38(6): 416-419. DOI:10.3760/cma.j.issn.0253-3006.2017.04.005 |
| [11] |
潘爱民, 王效强, 丁占一, 等. 亚甲蓝染色在腹腔镜精索静脉高位结扎术中保留淋巴管的应用[J]. 中华腔镜泌尿外科杂志(电子版), 2018, 12(6): 418-421. Pan AM, Wang XQ, Ding ZY, et al. Clinical application of methylene blue staining during lymphatic-sparing laparoscopic varicocelectomy[J]. Chinese Journal of Endourology (Electronic Version), 2018, 12(6): 418-421. DOI:10.3877/cma.j.issn.1674-3253.2018.06.014 |
| [12] |
Makari JH, Atalla MA, Belman AB, et al. Safety and efficacy of intratesticular injection of vital dyes for lymphatic preservation during varicocelectomy[J]. J Urol, 2007, 178(3): 1026-1030. DOI:10.1016/j.juro.2007.05.072 |
| [13] |
Sack BS, Schäfer M, Kurtz MP. the dilemma of adolescent varicoceles: do they really have to be repaired?[J]. Curr Urol Rep, 2017, 18(5): 38. DOI:10.1007/s11934-017-0686-7 |
| [14] |
Kolon TF, Clement MR, Cartwright L, et al. Transient asynchronous testicular growth in adolescent males with a varicocele[J]. Journal of Urology, 2008, 180(3): 1111-1114. DOI:10.1016/j.juro.2008.05.061 |
| [15] |
Silay MS, Hoen L, Quadackaers J, et al. Treatment of varicocele in children and adolescents: a systematic review and Meta-analysis from the European Association of Urology/European Society for Paediatric Urology Guidelines Panel[J]. Eur Urol, 2019, 75(3): 448-461. DOI:10.1016/j.eururo.2018.09.042 |
| [16] |
胡岩, 靳红霞, 齐灿, 等. 腹腔镜下保留精索淋巴管技术治疗青少年精索静脉曲张[J]. 中国微创外科杂志, 2018, 18(10): 899-901. Hu Y, Jin HX, Qi C, et al. Spermatic lymphatic vessels preservation of laparoscopy for adolescent varicocele[J]. Chin J Minim Inva Surg, 2018, 18(10): 899-901. DOI:10.3969/j.issn.1009-6604.2018.10.010 |
| [17] |
孙凡修, 刘海东, 王庆新, 等. 通过术中注射亚甲蓝行保留淋巴管的腹腔镜精索静脉高位结扎术的临床研究[J]. 泌尿外科杂志(电子版), 2017, 9(2): 28-30. Sun FX, Liu HD, Wang QX, et al. A clinical study of laparoscopic lymphatic sparing varicocelectomy using methylene blue[J]. Journal of Urology for Clinician (Electronic Version), 2017, 9(2): 28-30. DOI:10.3969/j.issn.1674-7410.2017.02.010 |
 2021, Vol. 20
2021, Vol. 20


