2. 苏州大学附属儿童医院(江苏省苏州市, 215000)
2. Affiliated Children's Hospital, Soochow University, Suzhou 215003, China
急性阑尾炎是儿童常见的急腹症之一。小儿阑尾壁相对较薄,炎症侵犯容易造成穿孔,较成人炎症穿孔率高,易引起腹膜炎,迅速导致严重的全身中毒症状,甚至危及生命[1]。C反应蛋白(C-reactive protein,CRP)、白介素-6(interleukin 6,IL-6)和降钙素原(procalcitonin,PCT)均属于机体炎症标志物,目前研究表明,上述指标在多种感染性疾病的诊断中均具有一定意义。CRP不受患者免疫功能、肝肾功能等多种因素的影响,故其灵敏度和稳定性均较高[2-5]。IL-6是参与脓毒症及脓毒血症发生过程的一种炎性介质,在机体发生炎症2~3 h后即可达到血浓度高峰。PCT作为人体重要的感染标记物,当细菌感染导致系统发生炎症反应时,血清PCT浓度可迅速升高[6-8]。本研究旨在探讨CRP、IL-6和PCT与小儿急性复杂性阑尾炎的关系,并量化其诊断价值。
材料与方法 一、一般资料本研究经医院伦理委员会审批,研究对象及监护人皆知情并签署同意书。收集2016年1月至2017年5月包头市第四医院小儿外科收治并接受手术治疗的小儿急性阑尾炎患者,术式均为腹腔镜下阑尾切除术。排除标准:①心肺功能不全、肝肾功能异常、自身免疫性疾病或罹患肿瘤;②近期接受过手术或发生重大创伤;③近期使用过抗生素、糖皮质激素或免疫抑制剂。最终纳入符合条件的患者96例,年龄2~12岁,平均年龄5.5岁,其中男60例,女36例。根据本院病理科对术后标本做出的最终病理诊断,将患者按照病理类型分为两组:单纯性阑尾炎组30例,复杂性阑尾炎组66例。两组患者年龄、性别、体重差异无统计学意义(P>0.05),具有可比性,见表 1。
| 表 1 两组患者一般资料比较 Table 1 Comparison of general data for two groups |
|
|
所有患者于入院当天术前2 h采集外周静脉血3 mL于干燥管中,2 000 r/min离心15 min,样品置于-70℃冰箱待测。
(二)分析方法CRP采用全自动微量蛋白分析仪及其配套试剂进行检测,IL-6、PCT检测分别采用相应的酶联免疫吸附法,试剂盒购自武汉博士德生物工程公司,检测时严格按照试剂说明书操作。
三、统计学处理采用SPSS19.0进行统计学分析,计量资料采用(x±s)进行描述,两组间比较采用独立样本t检验;计数资料采用频数和构成比进行描述,组间比较采用χ2检验;通过绘制ROC曲线,计算曲线下面积(area under the curve,AUC),获得各检测指标及联合指标的敏感性、特异性;AUC之间的显著性差异采用单一变量Z检验,P<0.05表示差异具有统计学意义。
结果 一、复杂性阑尾炎与单纯性阑尾炎炎性指标水平比较复杂性阑尾炎组CRP、IL-6、PCT水平均明显高于单纯性阑尾炎组,差异具有统计学意义(P<0.05),见表 2。
| 表 2 两组炎性指标水平比较 Table 2 Comparison of levels of inflammatory markers for two groups |
|
|
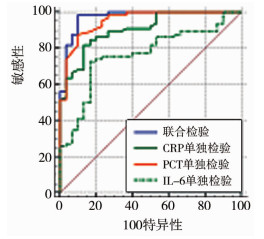
以手术后病理结果为金标准绘制ROC曲线,分析CRP、PCT、IL-6对复杂性阑尾炎诊断效能,得到CRP、PCT、IL-6及三者联合检验曲线下面积分别为0.906(95%置信区间:0.829~0.956)、0.953(95%置信区间:0.889~0.986)、0.765(95%置信区间:0.668~0.846)、0.973(95%置信区间:0.971~0.995)。曲线下面积值由大到小排序:PCT+CRP+IL-6>PCT>CRP>IL-6。经两两比较发现,联合检验的曲线下面积与CRP单独检验、IL-6单独检验曲线下面积差异存在统计学意义(Z=2.932,P=0.003;Z=3.854,P=0.0001);联合检验的曲线下面积与PCT单独检验比较差异无统计学意义(Z=1.861,P=0.063);CRP单独检验与PCT单独检验的曲线下面积差异无统计学意义(Z=1.668,P=0.095),IL-6单独检验与CRP单独检验、PCT单独检验比较曲线下面积差异具有统计学意义(Z=2.312,P=0.021;Z=3.371,P=0.001);得到最佳临界点分别为11.47(95%置信区间:11.42~14.48)mg/L,0.87(95%置信区间:0.63~0.98)ng/L,88.60(95%置信区间:87.12~170.83)pg/mL,见表 3、图 1。
| 表 3 CRP、IL-6、PCT及联合检验对复杂性阑尾炎诊断效能的比较 Table 3 Comparison of diagnostic efficacy of CRP, IL-6, PCT and combined tests for complex appendicitis |
|
|
|
图 1 CRP、IL-6、PCT及联合检验的ROC曲线 Fig.1 ROC curves of CRP, IL-6, PCT and combined tests |
小儿阑尾壁薄,管腔狭窄,容易造成阑尾腔梗阻和血运障碍,加上大网膜发育不全,故更容易发生化脓、坏疽,临床主张早期诊断后尽早进行手术[9]。但目前部分专家学者认为阑尾切除后可能导致消化系统、心血管系统、内分泌系统异常,早期急性单纯性阑尾炎大部分可选择内科治疗[10]。因此,需要尽早进行诊断并对阑尾炎病理类型进行区分[11-13]。
CRP不受患者免疫功能、肝肾功能等因素的影响,所以其灵敏度和稳定性均较高[14]。本研究发现,急性复杂性阑尾炎患者的CRP水平明显高于急性单纯性阑尾炎患者,在诊断效能的评价中,其灵敏度为81.82%,特异度为86.67%,曲线下面积为0.906,对急性复杂性阑尾炎具有较高的诊断效能。
PCT是一种血清降钙素的前体物,在人体内部很稳定,正常生理情况下,通过双抗夹心法检测正常人群血液中的PCT浓度,一般都在0.1 ng/mL以下。研究表明,PCT往往在感染发生的2 h之内迅速升高,约6 h左右达到顶峰[15]。IL-6是一种功能广泛的多效性细胞因子,机体受炎症刺激后由T细胞、B细胞、单核巨噬细胞及内皮细胞等分泌,是炎症介质网络的关键成分,也是急性期反应的主要调节因子之一,可调节局部、全身的炎症反应及免疫应答。有研究报道,IL-6的主要作用是放大和催化炎症反应,也是临床上诊断急慢性炎症常用的标志物,其含量越高代表感染越严重[16]。本研究表明,急性复杂性阑尾炎患者的IL-6水平明显高于单纯性阑尾炎组,但在诊断效能的评价中,其特异性及敏感度要低于CRP及PCT。
综上,CRP、IL-6和PCT与阑尾炎的严重程度均存在相关性,对小儿复杂性阑尾炎具有一定的诊断价值,且联合诊断的诊断效能更高,有助于医师对术前病情严重程度预判。
| [1] |
张金哲. 小儿腹部外科学(第1版)[M]. 杭州: 浙江科学技术出版社, 2008. Zhang JZ. Editor-in-Chief, Pediatric Abdominal Surgery (First Edition)[M]. Hangzhou: Zhejiang Science and Technology Publishing House, 2008. (in Chinese) |
| [2] |
Acharya A, Markar SR, Ni M, et al. Biomarkers of acute appendicitis:systematic review and cost-benefit trade-off analysis[J]. Surg Endosc, 2017, 31(3): 1022-1031. DOI:10.1007/s00464-016-5109-1 |
| [3] |
徐长胜. 腹腔镜手术治疗急性穿孔性阑尾炎的临床疗效及对血清C反应蛋白和降钙素原水平的影响[J]. 临床医学研究与实践, 2017, 2(23): 44-45. Xu CS. Clinical efficacy of laparoscopy for acute perforating appendicitis and its effect on serum levels of C-reactive protein and procalcitonin[J]. Clinical Research and Practice, 2017, 2(23): 44-45. DOI:10.19347/j.cnki.2096-1413.201723021 (in Chinese) |
| [4] |
孔燕军, 陈颖, 赵华头. C-反应蛋白在急诊中鉴别小儿肠系膜淋巴结炎与急性阑尾炎中的意义[J]. 中国美容医学, 2012, 21(10): 37-38. Kong YJ, Chen Y, Zhao HT. Role of C-reactive protein in the differential diagnosis of acute mesenteric lymphadenitis and acute appendicitis in children in emergency settings[J]. China Aesthetic Medicine, 2012, 21(10): 37-38. DOI:10.3969/j.issn.1008-6455.2012.10.028 (in Chinese) |
| [5] |
黄爱芳. 超敏C反应蛋白、白细胞计数联合检测对诊断小儿急性阑尾炎的临床意义[J]. 检验医学与临床, 2012, 9(20): 2620-2621. Huang AF. Clinical significance of combined detection of high-sensitivity C-reactive protein and white blood cell count in the diagnosis of acute appendicitis in children[J]. Laboratory Medicine and Clinical, 2012, 9(20): 2620-2621. DOI:10.3969/j.issn.1672-9455.2012.20.052 (in Chinese) |
| [6] |
周兵. 急性阑尾炎患者行D-二聚体, 降钙素原和C反应蛋白诊断的价值[J]. 深圳中西医结合杂志, 2017, 27(5): 79-80. Zhou B. Diagnostic values of D-dimer, procalcitonin and C-reactive protein in patients with acute appendicitis[J]. Shenzhen Journal of Integrated Traditional Chinese and Western Medicinee, 2017, 27(5): 79-80. DOI:10.16458/j.cnki.1007-0893.2017.05.038 (in Chinese) |
| [7] |
方红伟, 李峰. 血清降钙素原, 超敏C反应蛋白以及白细胞介素6在小儿急性上呼吸道感染中的临床诊断价值[J]. 新疆医学, 2014, 44(6): 16-18. Fang HW, Li F. Clinical diagnostic value of serum procalcitonin, hypersensitive C-reactive protein and interleukin-6 in children with acute upper respiratory tract infection[J]. Xinjiang Medical Science, 2014, 44(6): 16-18. (in Chinese) |
| [8] |
朱秋良. D-二聚体, 降钙素原和C反应蛋白在急性阑尾炎中的评价[J]. 国际检验医学杂志, 2013, 34(17): 2248-2249. Zhu QL. Evaluations of D-dimer, procalcitonin and C-reactive protein in acute appendicitis[J]. International Journal of Laboratory Medicine, 2013, 34(17): 2248-2249. DOI:10.3969/j.issn.1673-4130.2013.17.017 (in Chinese) |
| [9] |
Blab E, Kohlhuber U, Tillawi S, et al. Advancements in the diagnosis of acute appendicitis in children and adolescents[J]. Eur J Pediatr Surg, 2004, 14(6): 404-409. DOI:10.1055/s-2004-821152 |
| [10] |
张菊嫦.阑尾对肠道微生物影响的研究[D].南方医科大学, 2017.DOI: 10.7666/d.Y3280759. Zhang JC.Effects of appendix on gut microbiota[D].Southern Medical University, 2017.DOI: 10.7666/d.Y3280759. |
| [11] |
张甜. 实时监测血清降钙素原水平在小儿急性阑尾炎诊治中的应用价值[J]. 医学临床研究, 2017, 34(4): 749-751. Zhang T. Application value of real-time monitoring serum level of procalcitonin in the diagnosis and treatment of acute appendicitis in children[J]. Medical Clinical Study, 2017, 34(4): 749-751. DOI:10.3969/j.issn.1671-7171.2017.04.042 (in Chinese) |
| [12] |
张曼丽. 尿常规检验用于诊断小儿急性阑尾炎的临床观察[J]. 中国急救医学, 2016, 36(1): 6-7. Zhang ML. ML.Clinical observation of urinary routine examination for diagnosing acute appendicitis in children[J]. China Emergency, 2016, 36(1): 6-7. DOI:10.3969/j.issn.1002-1949.2016.z1.005 (in Chinese) |
| [13] |
Tanrıkulu CŞ, Karamercan MA, Tanrıkulu Y, et al. The predictive value of Alvarado score, inflammatory parameters and ultrasound imaging in the diagnosis of acute appendicitis[J]. Ulusal cerrahi dergisi, 2015, 32(2): 115-121. DOI:10.5152/UCD.2015.3103 |
| [14] |
Acharya A, Markar SR, Ni M, et al. Biomarkers of acute appendicitis:systematic review and cost-benefit trade-off analysis[J]. Surgical endoscopy, 2017, 31(3): 1022-1031. DOI:10.1007/s00464-016-5109-1 |
| [15] |
Hackam DJ, Afrazi A, Good M, et al. Innate immune signaling in the pathogenesis of necrotizing enterocolitis[J]. Clin Dev Immunol, 2013, 54(32): 2015-2025. DOI:10.1155/2013/475415 |
| [16] |
Yu CW, Juan LI, Wu MH, et al. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis[J]. Br J Surg, 2013, 100(3): 322-329. DOI:10.1002/bjs.9008 |
 2021, Vol. 20
2021, Vol. 20


