2. 四川省出生缺陷临床医学研究中心(四川省泸州市, 646000);
3. 凉山彝族自治州第一人民医院儿外科(四川省凉山州, 615000)
2. Sichuan Clinical Research Center for Birth Defects;
3. Pediatric Surgery, The First Hospital of LiangShan
儿童外伤性十二指肠血肿是一种临床少见的腹部闭合性损伤,约占腹部脏器损伤的3% ~5%[1]。因十二指肠为间位器官,位置固定,常合并周围脏器损伤,常伴有上消化道梗阻症状。随着CT影像技术的广泛应用,其诊断多不困难,但因其发病率不高,文献报道相对较少。现将西南医科大学附属医院儿外科近年来收治的8例确诊为外伤所致的十二指肠血肿伴上消化梗阻患者的临床诊治经验予以总结,并结合国内外文献进行分析,为临床诊治该病提供经验参考。
材料与方法以我院2014年至2017年我院收治的腹部闭合性损伤患者为研究对象。纳入标准:①有明确的腹部外伤史; ②以呕吐、腹痛为主要症状; ③影像学检查可见上消化道梗阻,CT检查可见沿十二指肠走行的血肿。排除十二指肠穿孔病例。本研究已通过西南医科大学附属医院伦理委员会批准。
符合纳入标准的患者有8例,男5例,女3例,年龄5~16岁,平均年龄9.1岁,均有外伤后硬物(木堆、水泥块、桌角)撞击中上腹部病史,于伤后10小时至7天前来就诊,主诉腹痛、频繁呕吐、呕吐物含胆汁样物,均无发热,生命体征平稳。详细临床资料见表 1。
| 表 1 外伤性十二指肠血肿患者临床资料 Table 1 Clinical data of eight children with duodenal intramural hematoma due to blunt abdominal trauma |
|
|
| 表 2 外伤性十二指肠血肿患者辅助检查资料 Table 2 Anxillary examinations of eight children with duodenal intramural hematoma due to blunt abdominal trauma |
|
|
入院后急诊行血常规、凝血、血及尿淀粉酶、血生化等常规检查,并行右下腹诊断性穿刺。患者于入院前或入院后均行腹部CT检查,可显示与十二指肠走形一致的混杂密度圆形、椭圆形肿块,提示十二指肠肠壁内血肿,并伴有上消化道梗阻。血肿部位:5例位于十二指肠降部及水平部,3例位于十二指肠降部,按照十二指肠损伤分级,3例为Ⅰ级,5例Ⅱ级[2]。部分患者于1周后病情平稳时行增强CT和稀释碘海醇上消化道造影检查,均提示存在完全性上消化道梗阻。
二、治疗8例入院后均给予心电监护、禁食、持续胃肠减压、抑酸、补液、止血、卧床休息等对症处理,并详细记录和观察患者胃肠减压液的量与颜色(图 1)。4例血淀粉酶有升高,3例超过正常值3倍,考虑存在胰腺损伤,给予生长抑素抑制胰腺分泌,病情稳定后给予肠外营养支持治疗,定期复查血常规、肝肾功能、血电解质、血及尿淀粉酶,维持内环境稳定,每周复查影像学检查1次。病例2经过保守治疗3周(包括院外治疗1周)后梗阻症状无缓解,胃肠减压液量持续维持在每天800 mL左右,颜色为绿色,上消化道造影提示完全性肠梗阻,复查腹部CT提示血肿大小无变化,血肿内为均匀一致密度影,CT值20~40 Hu,未见融冰征,考虑血肿已液化,行剖腹探查,可见十二指肠降段和水平段一血肿(约8.4 cm×4.3 cm×2.5 cm)压迫十二指肠造成完全梗阻,遂沿十二指肠纵轴切开浆肌层,吸引约60 mL暗褐色液体后胃管内注水见受压迫的十二指肠黏膜再次隆起,十二指肠再通,予血肿内留置引流管后关腹,术后继续给予禁食、胃肠减压、抗炎、补液等对症治疗。典型病例影像学检查结果见图 1至图 4,胃肠减压量趋势见图 5。
|
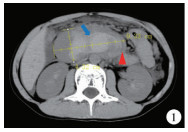
图 1 病例4入院时CT提示十二指血肿伴梗阻。红色箭头提示“空气裂隙征”,蓝色箭头提示“融冰征” Fig.1 In case No.4, admission CT hinted at duodenal intramural hematoma with obstruction.Red arrow implied airspace sign while blue arrow melting ice sign |

|
图 2 病例4受伤后10天上消化道造影提示完全梗阻,造影剂无法进入远端消化道 Fig.2 In case No.4, upper gastrointestinal contrast at Day 10 after trauma hinted at total obstruction.The constrasting agnet failed to enter distal gastrointestinal tract |

|
图 3 病例4受伤后16天上消化道造影提示十二指肠再通,红色箭头提示造影剂通过十二指肠进入远端消化道 Fig.3 In case No.4, upper gastrointestinal contrast at Day 16 after trauma hinted at duodenal patency.Red arrow indicated that the contrasting agent entered distal gastrointestinal tract via duodenum |
|
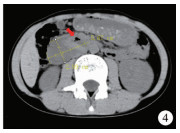
图 4 病例4受伤后20天复查CT提示血肿明显减小,且无“融冰征”,红色箭头提示十二指肠出现再通 Fig.4 In case No.4, upper gastrointestinal contrast at Day 20 after trauma hinted at a diminishing hematoma without a sign of melting ice.Red arrow indicated duodenal patency |

|
图 5 胃肠减压量趋势图 Fig.5 Trend graph of gastrointestinal decompression volume |
检索万方、维普、知网、PubMed、Medline数据库,以儿童(child/children)、外伤/创伤(trauma)、十二指肠血肿(duodenal hematoma)为关键词,检索日期截至2020年2月。剔除综述和无法获得全文资料的文献,符合检索条件的中英文文献31篇,共报道儿童外伤性十二指肠血肿病例331例。
结果除病例2外,其他患者经保守治疗后腹痛、呕吐症状缓解,恢复饮食时间为8~26天,平均15.2天,4例应用静脉营养10天后血生化检查提示肝酶学指标及胆红素轻度升高,考虑与禁食及静脉营养相关,予以保肝药物治疗及恢复饮食后逐渐降至正常,其余病例未出现并发症。出院时无发热,进食流质饮食及软食后无恶心、呕吐等不适。查体:腹平软,无明显压痛,腹部未扪及确切包块,复查血、尿各项指标正常,部分患者行上消化道造影证实造影剂顺利通过十二指肠,出院后随访6个月至3年,患者健康成长,正常进食,无上消化道梗阻症状。病例2在术后第3天即开始饮水及进流食,术后第5天恢复饮食,随访2年,因粘连性不全性肠梗阻住院1次,经保守治疗痊愈。
文献报道共计331例儿童外伤性十二指肠血肿,结合本组8例,共339例,均有上腹部钝性外伤病史,其中189例接受手术治疗的病例中有51例行急诊探查,探查原因为诊断不明确、存在腹膜炎体征、腹部其他脏器损伤,其中26例行血肿引流,16例行旁路手术,9例探查发现十二指肠血肿后未做其他处理,术后保守治疗痊愈;45例在诊断为十二指肠血肿后行延迟开腹手术,其中39例行血肿引流(3例加做空肠造瘘),6例行旁路手术;1例在治疗过程中因腹痛加重怀疑肠套叠,探查证实为十二指肠血肿,未做处理关腹后继续保守治疗10天痊愈;1例治疗过程中因腹痛加重行手术探查血肿引流;其余91例在保守治疗4~30天后因梗阻无缓解行手术治疗,其中67例行开腹血肿引流,19例行旁路手术,2例行腹腔镜引流,1例行B超引导下经皮血肿引流,2例行CT引导下经皮血肿引流。保守治疗150例,保守治疗时间7~29天。
讨论儿童十二指肠血肿是一种少见的腹部闭合性损伤,多因腹部钝性外伤所致,其他少见的原因包括抗凝治疗、血液系统疾病、医源性因素等[32-35]。因儿童肠腔面黏膜层较浆肌层更柔软、褶皱更多,故血肿形成后更趋向于突向肠腔,从而导致不同程度的十二指肠狭窄及梗阻[2]。本组病例中患者均存在呕吐等上消化道梗阻症状。大龄儿童尚能自诉上腹部疼痛,本组中3例存在右下腹疼痛,右侧腹部CT值为30~40 Hu,考虑可能为周围脏器损伤渗血,经结肠旁沟流至右下腹,从而出现局部血性腹膜炎,导致疼痛。由于血肿位于腹膜后,患者感知能力较差,因而存在延迟就诊现象,本组病例延迟就诊时间平均为2.52天,与国内报道的平均时间(2.5天)基本相符。
十二指肠血肿形成后,在CT图像上可见沿十二指肠走形的圆形或椭圆形混杂密度影,包括边缘病灶游离缘与肠管内气体形成新月形“空气裂隙征”和血凝块吸收浓缩呈“融冰征”,而无游离气体、腹盆腔大量积液等消化道穿孔或实质脏器出血表现,伴有胰腺损伤,可见胰周模糊不清,伴有肝脾损伤,可见脏器周围血肿[36]。再结合患者有典型外伤病史和上消化道梗阻症状,诊断多不困难。文献报道该病以保守治疗为主[1, 2]。与十二指肠穿孔需接受手术治疗不同,十二指肠壁内血肿多为良性,因其解剖位置较固定,且儿童肠壁各层弹性较成人好,不易破裂,出血量到一定压力后多可自行止血,一般不会引起持续大出血,经过积极的抗休克、止血等对症处理后患者生命体征平稳。即使其合并胰腺、肝脏、脾脏等周围器官的损伤,也可先试行保守治疗。既往报道显示十二指肠损伤的病死率较高,多为电解质紊乱及长期禁食、能量供给不足所致,随着持续胃肠减压和肠外营养的应用,其病死率已大大下降。Clendenon等[1]报道了42例十二指肠损伤患者,仅1例因严重颅脑损伤出现死亡,Michelle等[2]报道的19例保守治疗患者无一例死亡,国内报道的单纯十二指肠血肿也未见死亡病例。保守治疗的基本理论基础是十二指肠血供丰富,血肿可自行吸收,十二指肠可再通,Yang等[23]认为十二指肠血肿可能在2周内自行吸收,国内的文献亦报道其平均缓解时间为2~3周,故建议保守治疗的时间可根据病情转归适当延长至3周,国外研究报道最长禁食时间达29天[18, 30]。
本次研究中,7例给予保守治疗获得治愈,平均恢复进食时间为15.5天,最长为26天,与文献报道基本相符。因十二指肠血肿所致梗阻为上消化道梗阻,有大量消化液分泌,所以持续有效的胃肠减压是保守治疗的重要措施,目的是充分引流消化液,减轻消化液对血肿的刺激以及梗阻所致的腹胀、呕吐等不适。本研究对患者胃肠减压的量及颜色变化进行了详细的观察和记录,结果显示:在受伤后3~5天其胃肠减压量达到峰值,且为墨绿色,持续时间不定,在伤后4~18天胃肠减压量逐渐减少,颜色变清亮,部分患者经上消化道造影,证实造影剂通过梗阻部位进入远端消化道。本组研究中病例4(血肿大小:9.3 cm×4.3 cm)在确诊后第9天胃肠减压颜色逐渐变淡,量逐渐变少,行上消化道造影仍提示梗阻,继续坚持保守治疗,在确诊后第16天,胃肠减压量由峰值1 200 mL减少到400 mL,再次上消化道水溶性造影证实造影剂通过十二指肠进入远端消化道,考虑十二指肠再通,间断夹闭胃管,无腹胀、恶心、呕吐等不适,开始饮水及进食肠内营养液,逐步拔除胃管恢复流质饮食,确诊后第20天时复查CT显示血肿明显减小。因此本研究认为,在保守治疗过程中,观察胃肠减压液量及颜色的变化对判断疾病的转归及治疗方案的制定有重要指导意义,可避免不必要的上消化道造影和CT检查,减少患者的X线暴露。Michelle[2]亦指出当胃肠减压液不含胆汁时可逐步恢复肠内营养。在此经验的基础上,我们对后面2例更大血肿的患者进行胃肠减压液量与颜色的严密监测,坚持保守治疗,分别在确诊后第26天和确诊后第19天获得再通。
目前对抗休克、止血等对症处理后生命体征平稳的十二指肠血肿伴梗阻的手术治疗指征及手术时机,尚缺乏一致的意见。王勇等[29]指出保守治疗存在血肿持续压迫导致继发性损伤穿孔可能,且保守治疗时间长,经拖延后再选择手术时可能因血肿机化造成清除副损伤,该研究对13例血肿长径大于5 cm的病例进行了早期剖腹探查,术中清除十二指肠浆膜下及腹膜后血凝块,并留置引流管,术后2例出现切口感染,其余恢复顺利。Gregory等[28]报道了1例18岁腹部钝性损伤后导致十二指肠血肿,经保守治疗2周后症状无缓解,通过腹腔镜完成了对血肿的抽吸和冲洗,并留置引流,术后2天即开始进液体食物,随访恢复良好。Yang[23]报道了一例14岁十二指肠血肿患者在经过20天的保守治疗后复查CT提示血肿增大,给予超声引导下经皮血肿引流,在引出约90 mL暗褐色液体后第2天患者即开始进食流质饮食,4天后复查CT提示血肿基本消失,2周后恢复正常饮食无并发症发生。Patterson[37]报道了一例7岁患者经过11天保守治疗复查血肿增大(6 cm×4.8 cm×4.1 cm),经过CT引导穿刺引流约32 mL陈旧性液化性血液后获得治愈。Steven[38]认为十二指肠血肿可经皮引流的理论基础是超过2周后,血肿内很少有血凝块,而在血肿形成早期,血凝块仍会存在,早期经皮血肿引流则管道容易堵塞,引流不充分,这与我们早期能在血肿内看到血凝块浓缩形成“溶冰征”相符。本研究中1例在保守治疗3周后无缓解,术中发现血肿内仅60 mL暗褐色液体,无明显血凝块机化,血肿内未见多房和分隔现象,引流手术操作简单,引流效果好。
综上,对抗休克、止血等对症处理后生命体征平稳的十二指肠血肿伴梗阻应首选保守治疗。观察胃肠减压液量及颜色的变化,对判断疾病的转归及治疗方案的制定有重要指导作用。若胃肠减压液的量在逐渐减少、颜色变淡,保守治疗可延长至3周甚至更长时间;若保守治疗超过3周,梗阻仍无缓解迹象,影像学检查提示血肿无减小甚至有增大,仍建议手术治疗。此时血肿多已液化,手术操作简单、效果好,只需引流血肿内液体,无需剥离血凝块,可根据医疗条件选择开腹手术、腹腔镜手术或经皮穿刺引流。
| [1] |
Clendenon JN, Meyers RL, Nance ML, et al. Management of duodenal injuries in children[J]. J Pediatr Surg, 2004, 39(6): 964-968. DOI:10.1016/j.jpedsurg.2004.02.032 |
| [2] |
Peterson ML, Abbas PI, Fallon SC, et al. Management of traumatic duodenal hematomas in children[J]. J Surg Res, 2015, 199(1): 126-129. DOI:10.1016/j.jss.2015.04.015 |
| [3] |
Kelley JE. Duodenal hematoma:case report[J]. Mil Med, 1982, 147(2): 106-108. DOI:10.1093/milmed/147.2.106 |
| [4] |
Klausner JM, Merhav A, Lelcuck S, et al. Intramural haematoma of the duodenum following blunt abdominal injury-the place for conservative treatment[J]. Injury, 1986, 17(2): 131-132. DOI:10.1016/s0020-1383(86)80013-4 |
| [5] |
靳振怀, 孔燕. 小儿外伤性十二指肠壁内血肿1例报告[J]. 徐州医学院学报, 1988, 8(4): 245. Jin ZH, Kong Y. Traumatic intramural hematoma of duodenum in child:one case report[J]. Acta Academiae Medicinae Xuzhou, 1988, 8(4): 245. (in Chinese) |
| [6] |
Jewett TC Jr, Caldarola V, Karp MP, et al. Intramural hematoma of the duodenum[J]. Arch Surg, 1988, 123(1): 54-58. DOI:10.1001/archsurg.1988.01400250064011 |
| [7] |
Thoms CA, Ricketts RR. Intramural duodenal hematoma in children:reappraisal of current management[J]. South Med J, 1988, 81(8): 985-988. DOI:10.1097/00007611-198808000-00011 |
| [8] |
Grosfeld JL, Rescorla FJ, West KW, et al. Gastrointestinal injuries in childhood:analysis of 53 patients[J]. J Pediatr Surg, 1989, 24(6): 580-583. DOI:10.1016/s0022-3468(89)80511-1 |
| [9] |
Mehta MH, Patel RV, Bhoot NH, et al. Intramural duodenal hematoma following blunt bicycle handle bar injury[J]. Indian J Pediatr, 1993, 60(6): 836-838. DOI:10.1007/bf02751064 |
| [10] |
陆道瑯, 缪维洲, 王舒. 小儿外伤性十二指肠壁血肿2例报告[J]. 临床儿科杂志, 1993, 11(3): 193. Lu DL, Miu WZ, Wang S. Traumatic intramural hematoma of duodenum in child:two case report[J]. The Journal of clinical Pediatrics, 1993, 11(3): 193. (in Chinese) |
| [11] |
乔宝成, 孙明非, 马立新. 儿童外伤性十二指肠肠壁内血肿2例[J]. 中华小儿外科杂志, 1996, 17(1): 27. Qiao BC, Sun MF, Ma LX. A report of two cases of Traumatic intramural hematoma of duodenum in children[J]. Chin J Pediatr Surg, 1996, 17(1): 27. (in Chinese) |
| [12] |
Xeropotamos NS, Tsakayannis DE, Kappas AM. Intramural post-traumatic haematomas of the duodenum:are there any late sequelae of operative intervention?[J]. Injury, 1997, 28(5-6): 349-352. DOI:10.1016/s0020-1383(97)00031-4 |
| [13] |
Sidhu MK, Weinberger E, Healey P. Intramural duodenal hematoma after blunt abdominal trauma[J]. AJR Am J Roentgenol, 1998, 170(1): 38. DOI:10.2214/ajr.170.1.9423594 |
| [14] |
陆耀宇. 外伤性十二指肠壁内血肿致高位梗阻1例报告[J]. 江苏医药, 1999, 31(2): 168. Lu YY. A report of one case of traumatic intramural hematoma of the duodenum with high obstruction[J]. Jiangsu Medical Journal, 1999, 31(2): 168. (in Chinese) |
| [15] |
郑镇元, 张平. 小儿外伤性十二指肠壁内血肿3例临床分析[J]. 现代临床普通外科, 2000, 1(2): 95-96. Zheng ZY, Zhang P. Clinical analysis of three case in children with traumatic intramural hematoma of duodenum[J]. Modern Clinics in General Surgery, 2000, 1(2): 95-96. (in Chinese) |
| [16] |
Takishima T, Hirata M, Kataoka Y, et al. Delayed development of obstructive jaundice and pancreatitis resulting from traumatic intramural hematoma of the duodenum:report of a case requiring deferred laparotomy[J]. J Trauma, 2000, 49(1): 160-162. DOI:10.1097/00005373-200007000-00026 |
| [17] |
吴小平, 何启明. 外伤性十二指肠壁内血肿诊治分析(附1例报告及文献复习)[J]. 华西医学, 2003, 18(4): 541-542. Wu XP, He QM. Diagnosis and treatment of traumatic intramural hematoma of duodenum (Report of 1 case and literature review)[J]. West China Medical Journal, 2003, 18(4): 541-542. DOI:10.3969/j.issn.1002-0179.2003.04.064 (in Chinese) |
| [18] |
Desai KM, Dorward IG, Minkes RK, et al. Blunt duodenal injuries in children[J]. J Trauma, 2003, 54(4): 640-646. DOI:10.1097/01.Ta.0000056184.80706.9b |
| [19] |
谭丽华, 董岿然, 肖现民. 小儿外伤性十二指肠壁内血肿的诊断和治疗[J]. 中华小儿外科杂志, 2006, 10(27): 516-518. Tan LH, Dong KR, Xiao XM. The diagnosis and treatment of the dudenal intramural hematoma in children[J]. Chin J Pediatr Surg, 2006, 10(27): 516-518. DOI:10.3760/cma.j.issn.0253-3006.2006.10.004 (in Chinese) |
| [20] |
Iuchtman M, Steiner T, Faierman T, et al. Post-traumatic intramural duodenal hematoma in children[J]. Isr Med Assoc J, 2006, 8(2): 95-97. |
| [21] |
Ikeda T, Koshinaga T, Inoue M, et al. Traumatic intramural hematoma of duodenum with thrombasthenia in childhood[J]. Pediatr Int, 2007, 49(5): 668-671. DOI:10.1111/j.1442-200X.2007.02438.x |
| [22] |
Banieghbal B, Vermaak C, Beale P. Laparoscopic drainage of a post-traumatic intramural duodenal hematoma in a child[J]. J Laparoendosc Adv Surg Tech A, 2008, 18(3): 469-472. DOI:10.1089/lap.2007.0147 |
| [23] |
Yang JC, Rivard DC, Morello FP, et al. Successful percutaneous drainage of duodenal hematoma after blunt trauma[J]. J Pediatr Surg, 2008, 43(9): e13-e15. DOI:10.1016/j.jpedsurg.2008.03.068 |
| [24] |
武瑞清. 小儿外伤性十二指肠壁血肿4例诊治体会[J]. 中国实用儿科杂志, 2009, 24(1): 76-77. Wu RQ. Diagnosis and treatment of dudenal intramural hematoma in 4 children[J]. Chinese Journal of Practical Pediatrics, 2009, 24(1): 76-77. (in Chinese) |
| [25] |
Moon SB, Jung SE, Cheon JE, et al. Very large traumatic duodenal hematoma:successful percutaneous drainage in a child[J]. Eur J Pediatr Surg, 2009, 19(6): 412-413. DOI:10.1055/s-0029-1202255 |
| [26] |
陈有望. 小儿十二指肠壁内血肿2例报告[J]. 贵州医药, 2011, 35(10): 907-909. Chen YW. A report of two cases of Traumatic intramural hematoma of duodenum in children[J]. Guizhou Medical Journal, 2011, 35(10): 907-909. DOI:10.3969/j.ISSN.1000-744X.2011.10.016 (in Chinese) |
| [27] |
刘菁华, 李婷婷, 韩燕乔. 儿童十二指肠肠壁血肿3例[J]. 世界华人消化杂志, 2011, 19(22): 2411-2413. Liu JH, Li TT, Han YQ. A report of three cases of duodenal wall hematoma in children[J]. World Chinese Joural of Digestology, 2011, 19(22): 2411-2413. (in Chinese) |
| [28] |
Nolan GJ, Bendinelli C, Gani J. Laparoscopic drainage of an intramural duodenal haematoma:a novel technique and review of the literature[J]. World J Emerg Surg, 2011, 6(1): 42. DOI:10.1186/1749-7922-6-42 |
| [29] |
王勇, 汤绍涛, 李金朋. 小儿外伤性十二指肠血肿并肠梗阻13例[J]. 临床小儿外科杂志, 2014, 13(5): 430-431, 446. Wang Y, Tang ST, Lin JP. Duodenal hematoma and intestinal obstruction caused by Trauma in children:a report of thirteen cases[J]. J Clin Ped Sur, 2014, 13(5): 430-431, 446. DOI:10.3969/j.issn.1671-6353.2014.05.018 (in Chinese) |
| [30] |
陈红, 向波, 李福玉, 等. 儿童外伤所致单纯性十二指肠壁内血肿的诊治经验[J]. 临床小儿外科杂志, 2016, 15(1): 94-96. Chen H, Xiang B, Li FY, et al. Diagnosis and treatment of simple intramural hematoma of doudenum due to trauma in children[J]. J Clin Ped Sur, 2016, 15(1): 94-96. DOI:10.3969/j.issn.1671-6353.2016.01.028 (in Chinese) |
| [31] |
Kim SJ, Lee JH, Park SM, et al. Conservative management of traumatic acute intramural hematoma of duodenal 2nd and 3rd portion:A case report and review of literature[J]. Ann Hepatobiliary Pancreat Surg, 2020, 24(1): 109-113. DOI:10.14701/ahbps.2020.24.1.109 |
| [32] |
Eichele DD, Ross M, Tang P, et al. Spontaneous intramural duodenal hematoma in type 2B von Willebrand disease[J]. World J Gastroenterol, 2013, 19(41): 7205-7208. DOI:10.3748/wjg.v19.i41.7205 |
| [33] |
Jan IA, AlKaabi SK, AlMughadam A, et al. Simultaneous occurrence of intussusception and duodenal haematoma in a patient with Glanzmann's thrombasthenia[J]. Afr J Paediatr Surg, 2016, 13(4): 202-205. DOI:10.4103/0189-6725.194676 |
| [34] |
Williams ZB, Organ NM, Deane S. Inferior vena caval filter strut perforation causing intramural duodenal haematoma[J]. J Surg Case Rep, 2016, 2016(11): rjw170. DOI:10.1093/jscr/rjw170 |
| [35] |
Sowrey L, Lawson KA, Garcia-Filion P, et al. Duodenal injuries in the very young:child abuse?[J]. J Trauma Acute Care Surg, 2013, 74(1): 136-141. DOI:10.1097/TA.0b013e3182788cb2 |
| [36] |
李钱程, 张欣贤, 郝向东, 等. 儿童腹部钝性损伤致十二指肠肠壁血肿CT和MRI表现[J]. 医学影像学杂志, 2017, 27(27): 2171-2175. Li QC, Zhang XX, Hao XD, et al. The CT and MIiI findings of intramural hematoma duodenum in children with blunt abdominal trauma[J]. J Med Imaging, 2017, 27(11): 2171-2175. (in Chinese) |
| [37] |
Patterson VM, Goettler CE, Thomas CC. Traumatic duodenal hematoma in a pediatric patient treated by percutaneous drainage[J]. Am Surg, 2011, 77(11): e220-e221. |
| [38] |
Hanish SI, Pappas TN. CT guided drainage of a duodenal hematoma after trauma[J]. J Trauma, 2007, 63(1): e10-e12. DOI:10.1097/01.ta.0000270107.78188.fb |
 2021, Vol. 20
2021, Vol. 20


