新生儿坏死性小肠结肠炎(necrotizing enterocolitis, NEC)是新生儿(尤其是早产儿)常见的急性消化道疾病[1]。近年来随着早产儿及低出生体重儿人数的增多,NEC发病率有所上升;伴随着围产期和新生儿重症医学技术的进步,NEC急性期的病死率有所下降,因此炎症后的肠狭窄病例愈来愈多[2]。本文回顾性分析2012年6月至2019年6月上海市儿童医院普外科行一期肠切除肠吻合术治疗的18例NEC后肠狭窄患儿临床资料,现报道如下。
材料与方法 一、临床资料患儿临床资料见表 1,包括临床表现、实验室检查、影像学检查、术前诊断、手术方法和疗效。
| 表 1 18例NEC后肠狭窄患儿的临床资料 Table 1 Clinical data of 18 children with intestinal stenosis after operations for NEC |
|
|
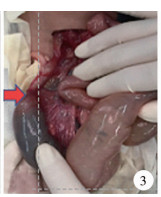
患儿均在气管插管全身麻醉下进行剖腹探查手术,选取右上腹横切口,探查肝胆胰脾肾未见异常,腹腔内渗液较澄清;探查腹腔见肠管扩张积气积液,并伴有不同部位的肠狭窄,均采用Ligasure或超声刀处理离断系膜血管,切除狭窄段肠管,分别行回肠-回肠、回肠-结肠、结肠-结肠端端吻合术。其中4例因狭窄部位包含回盲部,故回盲部未保留(图 1至图 4)。术后病理诊断均为:肠狭窄,慢性炎症细胞浸润聚集伴点灶坏死后改变。

|
图 1 腹腔内肠管积气明显,肠襻扩张,肠梗阻 Fig.1 Abdominal distension of intestine was obvious with intestinal dilatation and obstruction |

|
图 2 钡剂灌肠造影提示结肠显影,升结肠纤细,造影剂难以进入小肠。同时考虑扩张肠管可能为回肠末端 Fig.2 Barium enema angiography hinted at colonic visualization.Ascending colon was slender and contrast agents were difficult to enter small intestine.And distended intestine might be terminal ileum |
|
图 3 剖腹探查可见箭头所指处回肠末端狭窄,近端肠管扩张 Fig.3 Exploratory laparotomy revealed that terminal ileum was narrow and proximal intestine became dilated |

|
图 4 切除标本可见自回肠末端至升结肠狭窄明显 Fig.4 Excised specimen demonstrated marked stenosis from terminal ileum to ascending colon |
18例中17例为低出生体重儿,出现NEC症状后至肠狭窄的平均时间为45.7天,手术平均日龄73.8天。术前X-ray均提示肠腔扩张积气伴肠梗阻,消化道造影(BE灌肠)肠狭窄发现率仅8/18(44.4%),狭窄部位均位于结肠。剖腹探查发现狭窄部位仅1处者14例:7例位于回肠末端,5例位于升结肠,2例位于降结肠。多发狭窄者4例:1例位于回盲部和降乙交界,1例位于回肠末端和降乙交界,1例位于升结肠和横结肠中段,1例位于结肠肝曲和脾曲。
术后出现并发症5例(5/18,27.78%),其中2例吻合口漏因腹腔感染、肠壁水肿粘连等原因行造瘘术;1例吻合口狭窄伴伤口全层裂开,探查吻合口近段肠管扩张明显,考虑吻合术后再发狭窄,遂行原吻合口切除加保护性肠造口术;1例为两处吻合者,二次手术探查两处吻合口均无异常,其近端回-结肠吻合口的近端肠管因粘连扭转180°伴肠坏死,肠管因扭转后扩张水肿,因此在该处行保护性回肠造瘘;另1例再发回盲部狭窄,再行肠切除肠吻合术。随访5个月至7年,无一例死亡,4例肠造瘘者已关瘘3例,其余病例无腹痛,无肠粘连、肠梗阻、肠坏死等并发症,预后良好。
讨论NEC发病迅速,早期诊断困难,病死率高[3]。随着近年来围产期及新生儿重症医学的发展,NEC急性期病情有所控制,但因炎症造成的后期继发性肠狭窄逐渐增多,随之而来的NEC后肠狭窄诊断及治疗等问题越来越多[4]。Lamireau等[5]总结了10年病例资料,发现NEC后肠狭窄的并发症发生率从15%上升到了57%。
NEC后的肠狭窄为继发性狭窄,发生率为11.0% ~35.0%[7]。研究证明,任何引起胎儿肠道损伤和肠系膜血管缺血的因素均可导致肠闭锁与肠狭窄的发生[7]。继发性肠狭窄及肠闭锁的原因目前并不清楚,各家观点不一,但大多数学者认为是血栓及炎症后肠壁缺血性损伤修复的结果。而NEC后肠狭窄发生的时间也存在较大差异,国内沈淳[8]报道的11例平均为29.7天,Schimpl等[9]报道的16例中,NEC治愈后平均49天出现肠狭窄。对于肠狭窄出现的部位来讲,多为回肠末端和结肠,少数为多发狭窄。本组病例中7例位于结肠,7例位于回肠末端,另4例多发狭窄为以上两处位置的不同组合,与文献报道一致。
NEC后肠狭窄主要的临床表现为恢复饮食后出现反复喂养不耐受、宿奶、呕吐、腹胀、排便次数及量的减少等。诊断常借助的影像学检查包括X线、上消化道GI造影和BE钡剂灌肠等。Radhakrishnan等[10]提出在NEC治愈后喂养前常规行GI和BE检查,发现其中仅18%(9/50)的患儿两项造影检查均提示结肠狭窄,且均经手术确认。本组研究中均行BE造影,仅有8例发现不同部位结肠狭窄,本组BE检查无一例发现回肠末端的狭窄,究其原因,首先狭窄位置较高至造影剂无法达到狭窄位置而显影,其次回肠末端狭窄者多数伴有狭窄近段肠管扩张,患儿腹胀明显,BE灌肠若造影剂外溢则检查本身的风险较高,再者本组有10例BE未发现肠狭窄,检查时间为其出现腹胀的早期,此时肠管狭窄可能还未完全形成,而后期急剧的肠管扩张,多以X-ray提示的肠梗阻为根据行剖腹探查。临床上,借助X-ray所示的肠梗阻表现(如明显孤立扩张合并宽大液平面的肠襻),随访后对比无明显改善者,结合临床表现及明确的NEC病史,即便早期BE检查结果为阴性,也应高度怀疑NEC后肠狭窄[11, 12]。
治疗方面,目前大多数学者主张行一期肠切除肠吻合术,另有学者先行狭窄肠段切除术,后行肠端端吻合术,于其近端行保护性的肠造瘘,二期再行肠造口关闭术[5]。但随着研究的深入,2016年的NEC外科手术治疗专家共识中,针对NEC后肠狭窄,推荐一期行肠切除吻合术为其首选术式[13]。
虽然本组18例均采用一期肠切除吻合术,13例(13/18,72.22%)预后效果良好,但仍有5例出现术后并发症,因此作者认为该术式的选择仍需病例具备一定基础,主要取决于患者是否处于NEC急性期后以及术中肠管的条件。据报道,肠狭窄多见于NEC急性期后2~3个月内,迟发性的也可出现于发病后20个月,甚至有个案报道NEC后11年出现肠狭窄[14]。若过早行一期肠切除肠吻合术,术后可能因病情进展再发吻合口或其他部位的狭窄,此种情况的判定除需综合患儿的临床表现及炎症指标外,术中探查所有肠管并对可疑狭窄肠管做相应处理也尤为重要[15, 16]。本组并发症中就有1例为吻合口狭窄,二次手术行肠造瘘术;另有1例为再发回盲部狭窄,该例一期肠切除肠吻合术的手术时间为NEC发生后的第51天,术中探查狭窄部位为降结肠和乙状结肠交界处,同时发现升结肠起始部位出现肠管水肿,向该处肠管内注水后肠管充盈并无狭窄,考虑术后有恢复的可能并希望尽可能保留回盲部,当时一期手术仅行降乙交界处的狭窄切除吻合,然而术后1周再次出现狭窄症状,探查即为之前肠壁水肿处形成的回盲部至升结肠狭窄。后期我们也碰到了1例类似病例,鉴于之前的经历,术者在进行了狭窄肠段切除后又在水肿部位近端行保护性造瘘,而关闭造瘘时发现之前水肿部位已发展为完全肠狭窄。对此,一期肠切除肠吻合术在治疗NEC后肠狭窄手术的时间上以及保留肠管的质量上仍需谨慎斟酌。
一期肠切除肠吻合术治疗NEC后肠狭窄是否能够成功,除了术者的吻合技术以外,对吻合肠管的处理也非常重要。本组中1例两处吻合者,其近端回肠-结肠吻合口的近段回肠扭转坏死,二次手术原因为近端肠管粘连后造成180°扭转,导致肠管缺血坏死;另2例吻合口漏主要原因为肠管切除范围较长,吻合口张力较高,系膜血管牵拉过紧。以上情况的发生更加警示了保留肠管活性的重要性,NEC后肠狭窄所行的一期肠切除肠吻合术虽区别于急性期的一期吻合,但肠管血供的问题仍然要重视。若吻合肠管距离较远,肠管系膜牵拉太紧,则会导致吻合口缺血再狭窄,此时不可强行做一期肠切除肠吻合术,建议暂行肠造瘘术,再行二期关瘘手术[17]。
对于NEC后肠狭窄行一期肠切除肠吻合术,术后存在并发症并行肠造瘘者,二期关瘘手术前需同NEC急性期肠造瘘者一样,首先评估患者一般情况,再行钡剂造影检查,排除造口远端肠管是否再发狭窄[18]。术前行肠道准备时从造口远端注入温盐水,术中对可疑狭窄处注水确保其肠腔通畅,对于多处狭窄者亦可行多处吻合[19, 20]。
总之,肠狭窄是NEC保守治疗后最常见的继发性病变,治疗首选一期肠切除肠吻合术。NEC后若患儿出现反复宿奶、呕吐、腹胀、排便减少等症状,X线片提示肠梗阻,即使BE检查未发现肠狭窄也需考虑伴发NEC后肠狭窄,应及时手术探查。NEC后狭窄部位常位于回肠末端和结肠,需警惕多发狭窄的可能。在条件允许的情况下应行一期肠切除肠吻合术,对手术时间的把握和保留肠管质量的保证需综合考虑,术中应充分评估肠管条件,保证吻合质量,尽量避免二次手术。
| [1] |
Sheng QF, Lv ZB, Xu WJ, et al. Short-term surgical outcomes of preterm infants with necrotizing enterocolitis:A single-center experience[J]. Medicine (Baltimore), 2016, 95(30): e4379. DOI:10.1097/MD.0000000000004379 |
| [2] |
Zani A, Eaton S, Puri P, et al. International survey on the management of necrotizing enterocolitis[J]. Eur J Pediatr Surg, 2014, 25(1): 27-33. DOI:10.1055/s-0034-1387942 |
| [3] |
Seeman SM, Mehal JM, Haberling DL, et al. Infant and maternal risk factors related to necrotising enterocolitis-associated infant death in the United States[J]. Acta Paediatr, 2016, 105: 240-246. DOI:10.1111/apa.13390 |
| [4] |
Heida FH, Loos MH, Stolwijk L, et al. Risk factors associated with postnecrotizing enterocolitis strictures in infants[J]. J Pediatr Surg, 2016, 51(7): 1126-1130. DOI:10.1016/j.jpedsurg.2015.09.01 |
| [5] |
Lamireau T, Lianas B, Chateil JF, et al. Increasing frequency and diagnostic difficulties in intestinal stenosis after necrotizing enterocolitis[J]. Arch Pediatr, 1996, 3(1): 9-15. DOI:10.1016/s0929-693x(96)80002-9 |
| [6] |
潘登, 王献良, 邵雷朋. 新生儿坏死性小肠结肠炎经回肠造瘘术后远端肠闭锁7例[J]. 临床小儿外科杂志, 2016, 15(5): 513-515. Pan D, Wang XL, Shao LP. Management of acquired intestinal atresia after ileostomy due to necrotizing enterocolitis:a retrospective study of 7 cases[J]. J Clin Ped Sur, 2016, 15(5): 513-515. DOI:10.3969/j.issn.1671-6353.2016.05.028 (in Chinese) |
| [7] |
Trevor DC, Bailey HE, Amanda IU, et al. Direct peritoneal resuscitation improves survival and decreases inflammation after intestinal ischemia and reperfusion injury[J]. J Surg Res, 2015, 199(2): 428-434. DOI:10.1016/j.jss.2015.06.031 |
| [8] |
董晨彬, 郑珊, 沈淳. 新生儿坏死性小肠结肠炎后肠狭窄14例诊疗体会[J]. 中华小儿外科杂志, 2012, 33(5): 344-347. Dong CB, Zheng S, Shen C. Management of intestinal strictures after necrotizing enterocolitis:a retrospective study of 14 cases[J]. J Clin Ped Sur, 2012, 33(5): 344-347. DOI:10.3760/cma.j.issn.0253-3006.2012.05.007 (in Chinese) |
| [9] |
Schimpl G, Hollwarth ME, Fotter R, et al. Late intestinal strictures following successful treatment of necrotizing enterocolitis[J]. Aeta Paediatr, 1994, 83(s396): 80-83. DOI:10.1111/j.1651-2227.1994.tb13251.x |
| [10] |
Radhakrishnan J, Blechman G, Shrader C, et al. Colonic strictures following successful medical management of necrotizing enterocolitis:a prospective study evaluating early gastrointestinal contrast studies[J]. J Pediatr Surg, 1991, 26(9): 1043-1046. DOI:10.1111/codi.12436 |
| [11] |
梁琼鹤, 张新荣, 杨明, 等. 钡灌肠在新生儿坏死性小肠结肠炎后遗肠狭窄中的诊断价值[J]. 实用放射学杂志, 2017, 33(3): 476-477. Liang QH, Zhang XR, Yang M, et al. Value of barium enema in post-necrotizing enterocolitis strictures[J]. Journal of Practical Radiology, 2017, 33(3): 476-477. DOI:10.3969/j.issn.1002-1671.2017.03.040 (in Chinese) |
| [12] |
Zhang H, Chen J, Wang Y, et al. Predictive factors and clinical practice profile for strictures post-necrotising enterocolitis[J]. Medicine, 2017, 96(10): e6273. DOI:10.1097/MD.0000000000006273 |
| [13] |
中华医学会小儿外科分会新生儿外科学组. 新生儿坏死性小肠结肠炎外科手术治疗专家共识[J]. 中华小儿外科杂志, 2016, 37(10): 724-727. Group of Neonatal Surgery, Branch of Pediatric Surgery. Chinese Medical Association:Expert Consensus on Surgery for Neonatal Necrotizing Enterocolitis[J]. J Clin Ped Sur, 2016, 37(10): 724-727. DOI:10.3760/cma.j.issn.0253-3006.2016.10.002 (in Chinese) |
| [14] |
Goettler CE, Stallion A, Grisoni ER, et al. An unusual late complication of necrotizing enterocolitis[J]. J Pediatr Surg, 2001, 36(12): 1853-1854. DOI:10.1053/jpsu.2001.28868 |
| [15] |
Burnand KM, Zaparackaite I, Lahiri RP, et al. The value of contrast studies in the evaluation of bowel strictures after necrotising enterocolitis[J]. Pediatr Surg Int, 2016, 32(5): 465-470. DOI:10.1007/s00383-016-3880-7 |
| [16] |
Cuna AC, Reddy N, Robinson AL, et al. Bowel ultrasound for predicting surgical management of necrotizing enterocolitis:a systematic review and meta-analysis[J]. Pediatr Radiol May, 2018, 48(5): 658-666. DOI:10.1007/s00247-017-4056-x |
| [17] |
Hong CR, Han SM, Jaksic T. Surgical considerations for neonates with necrotizing enterocolitis[J]. Semin Fetal Neonatal Med, 2018, 23(6): 420-425. DOI:10.1016/j.siny.2018.08.007 |
| [18] |
Banerjee DB, Vithana H, Sharma S, et al. Outcome of stoma closure in babies with necrotising enterocolitis:early vs late closure[J]. Pediatr Surg Int, 2017, 33(7): 783-786. DOI:10.1007/s00383-017-4084-5 |
| [19] |
Talbot LJ, Sinyard RD, Rialon KL, et al. Influence of weight at enterostomy reversal on surgical outcomes in infants after emergent neonatal stoma creation[J]. J Pediatr Surg, 2017, 52(1): 35-39. DOI:10.1016/j.jpedsurg.2016.10.015 |
| [20] |
陈发玲, 徐伟珏, 李龙至, 等. 不同病变范围新生儿坏死性小肠结肠炎手术干预效果分析[J]. 中华实用儿科临床杂志, 2016, 31(23): 1783-1786. Chen FL, Xu WJ, Li LZ, et al. Outcomes of surgical intervention for necrotizing enterocolitis with different pathological ranges[J]. Chinese Journal of Applied Clinical Pediatrics, 2016, 31(23): 1783-1786. DOI:10.3760/cma.j.issn.2095-428X.2016.23.006 (in Chinese) |
 2020, Vol. 19
2020, Vol. 19


