腹腔镜输尿管再植术主要用以治疗膀胱输尿管反流(vesicoureteral reflux, VUR)和膀胱输尿管交界处梗阻,该技术最先由Lakshmanan等[1]报道,随后Yeung等[2]报道气膀胱下完成跨三角区输尿管再植术(Cohen术),目前该技术已被广泛应用,且成功率较高,但是Cohen术是将输尿管交叉及开口于对侧,给未来上尿路疾病的处理带来不便。Politano-Leadbetter术保留了原始输尿管的走形位置及开口,解决了上述问题。但以往报道均用于传统开放式手术中,因其手术难度大,目前国内尚无以微创方式行Politano-Leadbetter术治疗小儿输尿管膀胱连接部异常的报道。厦门市妇幼保健院小儿外科近年来对原发性膀胱输尿管连接部异常患儿进行了气膀胱腹腔镜下Politano-Leadbetter术,手术顺利,实现了此术式的微创化,解决了Cohen术的弊端,并提出了新的操作方法以降低手术难度,提高手术成功率。本文旨在介绍该方法的操作细节,并记录了短期随访结果,现将结果报道如下。
材料与方法 一、临床资料本研究共纳入10例输尿管膀胱连接部异常患儿,其中男童6例,女童4例;单侧6例,双侧4例,共14侧输尿管;膀胱输尿管反流6例10侧,Ⅲ度反流1侧,Ⅳ度反流6侧,Ⅴ度反流3侧;输尿管狭窄4例;年龄1.76~24个月。本组患儿以反复尿路感染、发热为首发症状,经逆行排泄性膀胱尿道造影(voiding cystourethrography,VCUG)、静脉泌尿系统造影(intravenous pyelography,IVP)、泌尿系统彩超及磁共振检查明确诊断,待泌尿系统感染控制后行手术治疗。患儿均常规行尿常规、肾功能检查、泌尿系统彩超、IVP、VCUG、放射性核素肾动态和静态显像检查。其中1例存在轻度肾功能损伤;放射性核素肾动态显像检查发现4例肾小球滤过率下降,静态显像提示均无肾瘢痕形成。10例患儿临床特点及转归见表 1。
|
|
表 1 10例输尿管膀胱连接部异常患儿临床特点及转归 Table 1 Clinical characteristics and outcomes of 10 children with congenital malformation of vesicoureteral junction |
手术指征:本组10例患儿共14侧输尿管,其中5例膀胱输尿管反流病例为Ⅳ度以上,所有患儿于第一次感染控制后均口服预防量抗生素,在巩固治疗过程中出现再次感染或多次感染后,决定手术治疗,另外4例膀胱输尿管狭窄患儿经明确诊断后即行手术治疗。
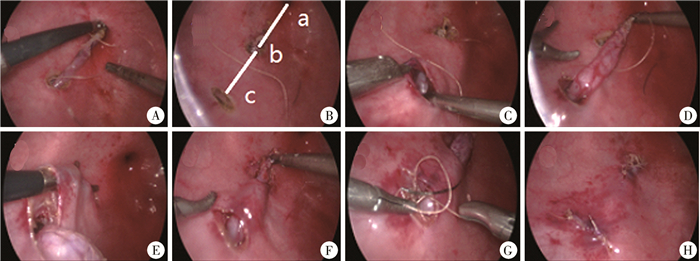
二、手术方法所有患儿术前禁食4 h,禁水2 h,在全身麻醉下进行气膀胱腹腔镜下Politano-Leadbetter术。首先建立气膀胱:患儿取仰卧位,插入膀胱镜,注入CO2,压力维持在8~10 mmHg,使膀胱高度膨胀,在膀胱镜引导下,于膀胱顶部(脐下1~2 cm处)置入5 mm Trocar,自此Trocar置入腹腔镜,于其左、右外下方分别置入2个3 mm Trocar,置入手术操作器械,拔出膀胱镜,经Trocar侧孔注入CO2建立气膀胱,术中压力维持在6~8 mmHg,流量控制在3.0~5.0 L/min;为解决气体外漏腹腔,常规于脐部置入F12号尿管引流腹腔气体,无需置入Trocar。首先用电钩在异常侧输尿管口外周0.3 cm做环状黏膜切口,电凝功率20~25 W,逐层分离黏膜下层,游离膀胱壁段输尿管及膀胱外输尿管,游离中应防止灼伤输尿管壁及保护管壁血管。输尿管游离完成后,末端缝合5 - 0可吸收线1针以备其回缩膀胱外时回牵。沿输尿管在膀胱内投影,距输尿管口2.5~3.0 cm处(输尿管直径的4~5倍),与原输尿管口、尿道内口三点连线,切开膀胱壁进入膀胱外间隙,可见膜状结缔组织,切开并找到输尿管,直视下将其牵入膀胱内,向近端进一步完成输尿管的游离。输尿管进入膀胱处应充分松解输尿管前方束缚结缔组织,确保输尿管进入膀胱处无压迫及角度适宜,此步骤对于男性患儿多会显露毗邻的输精管,对于女性则会显露输卵管,较易分辨,注意避免损伤(如输尿管增粗显著需裁剪至适合口径后连续缝合重塑管型)。将原输尿管口处肌层缝合关闭,再经上方切口向原输尿管开口处做一黏膜下隧道,将输尿管经黏膜下隧道送至原开口处,剪除多余输尿管末段,缝合建立新输尿管口。输尿管应剪除远端狭窄段,直至管径正常处,输尿管后壁应缝至原位切口的最远端,仅在输尿管过于细小或行裁剪病例留置双J管或支架管,其他情况下不常规留置输尿管支架。手术过程见图 1。
|
Download:
|
| 图 1 输尿管膀胱连接部异常患儿行气膀胱腹腔镜下Politano-Leadbetter术的手术过程图 注 A:游离患侧(左侧)输尿管; B:a尿道口;b原输尿管开口;c于原输尿管口外上放切开新的输尿管膀胱入口。a-b-c三点连成直线; C:切开膀胱壁直视下逐层分离找到输尿管; D:将输尿管经c口迁入膀胱壁; E:建立黏膜下隧道(从c口向b口方向);F:将输尿管经黏膜下隧道重新迁回原输尿管口处(b口);G:缝合C口;H:将修剪后的输尿管末端与原输尿管开口(b口)吻合 Fig. 1 Politano-Leadbetter procedure of children with abnormal ureteral bladder junction under pneumatic bladder laparoscopy A:Liberating left ureter; B:a urethral opening; b original ureteral opening; c cutting a new ureteral bladder inlet outside original ureteral opening.a-b-c connecting three points in a straight line; C:Cutting bladder wall under direct vision for separating ureter layer-by-layer; D:Moving ureter into bladder wall through port C; E:Establishing a submucosal tunnel (from port c to port b); F:relocating ureter through submucosal tunnel back to original ureteral port (port b); G:Suture port C; H:End of trimmed ureter was matched with original ureteral opening (port b) | |
术后给予预防感染、解痉、止血、补液及对症治疗,第8天拔除尿管,术后均应用抗生素至尿常规恢复正常,如留置双J管支架管,则于术后1个月取出。记录患儿手术时间、住院时间、术后并发症及输尿管反流及扩张情况。随访时间6~12个月,分别于术后1个月、术后3个月复查泌尿系统超声。
结 果10例均顺利完成手术,所有患儿术后无尿漏、膀胱输尿管反流、输尿管膀胱连接部梗阻等并发症发生。
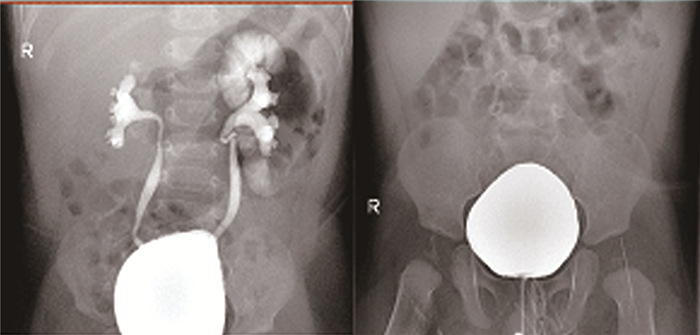
术后1个月、3个月复查泌尿系统超声提示患儿患侧肾积水均减轻,输尿管扩张好转;8侧术前输尿管扩张明显,术后3个月复查超声提示输尿管直径已恢复正常。6例术后复查逆行造影检查均未见复发。1例左侧输尿管狭窄患儿术后第2个月因尿路感染住院治疗,治愈后出院,随访至今未复发,目前仍在随访中;其余9例术后随访均无尿路感染, 见图 2。
|
Download:
|
| 图 2 术后6个月复查造影未见反流复发 Fig. 2 At 6 months post-operation, angiography revealed no recurrent reflux | |
目前,小儿输尿管再植的微创手术主要包括膀胱外输尿管再植术(Lich-Gregoir术)和膀胱内输尿管再植术(Cohen术、Glenn-Anderson术、Politano-Leadbetter术)。由于腹腔镜下Lich-Gregoir术在膀胱外盆腔内操作,易损伤盆腔神经丛,术后发生尿潴留的概率较高[3]。此外,术中易损伤腹腔脏器,对胃肠道功能干扰较大,术后肠道功能恢复较慢[4, 5]。2006年上海复旦大学附属儿科医院毕允力等[6]报道了11例Cohen术后反流治愈率达90.9%,现Cohen术已广泛应用于治疗膀胱输尿管连接部异常疾病(膀胱输尿管反流、狭窄、囊肿等),但手术改变了输尿管走行轨迹与输尿管开口位置,不能最大限度保持膀胱壁的原始解剖结构[7]。同时由于输尿管解剖结构和走行发生改变,术后将不能经尿道外口行膀胱镜输尿管逆行插管检查及治疗,给术后上尿路结石等并发症及其他疾病的处理带来一定困难[8]。Glenn-Anderson术将新输尿管开口前移至近膀胱颈处而保留了正常的尿路解剖走形,处理上尿路结石较为方便,但黏膜下隧道长度不够,一定程度上影响了抗反流效果,限制了这一术式在婴幼儿及输尿管扩张较严重患儿中开展[8, 9]。据文献报道目前开放式Politano-Leadbetter术的整体疗效良好,术后并发症较少。但创建新的输尿管裂孔仍是此术式的难点,导致近些年此术式学习曲线较长,开展速度较慢[9]。曾莉等[10]亦报道了开放式改良的Politano-Leadbetter术,将膀胱壁全层切开,降低了此术式的难度,但手术创伤较大,严重膀胱痉挛引起的术后疼痛是较常见的并发症,需要额外使用镇痛药和抗毒蕈碱药物。该术式最常见并发症主要包括尿漏、输尿管膀胱连接部梗阻、尿路感染、膀胱输尿管反流复发或持续存在,因开放手术对膀胱肌层创伤较大,继而影响了输尿管在膀胱壁内段的走行,不能充分舒展,导致输尿管扭曲或成角造成梗阻[11, 12]。Shigehiro等[13]亦报道了气膀胱腹腔镜下Politano-Leadbetter术,但需借助膀胱镜寻找膀胱外输尿管,并结合其他手术方式进行治疗,过程较为复杂,手术时间较长。
本组10例患儿均取得满意的治疗效果,术后随访中1例1.76月龄小婴儿于胚胎期发现肾积水,输尿管反流扩张严重,生后1月余反复出现泌尿系统感染,并伴有急性肾功能衰竭,抗感染治疗控制良好后于1.76月龄行气膀胱下双侧Politano-Leadbetter术治疗,手术时间稍长于年长儿,但术后仅发生一次泌尿系统感染,随访6个月未见复发。刘颖等[14]也曾报道气膀胱下输尿管再植术在小婴儿中手术时间长于较年长儿。本研究病例数相对较少,未进行对比研究,但和其他双侧再植时间对比并没有明显延长,其余并发症均未发生,也未发现存在明显膀胱痉挛的病例,是否与微创手术对膀胱牵拉程度及损伤较小有关,有待今后进一步总结。该术式既最大限度地保留了膀胱壁输尿管的原始解剖结构,符合输尿管走形的生理结构特点,也能够保证建立足够长度的黏膜下隧道,从而起到抗反流的作用,尤其是不经过腹腔操作,减少了腹腔损伤与肠管粘连的机会,术后胃肠道恢复更快。而本术式将手术步骤简化,缩短了手术时间,为日后的初学者缩短学习曲线提供了捷径。曾有文献报道气膀胱下输尿管再植术不适用于6月龄以下的患儿[15]。气膀胱下行输尿管剪裁需要更长时间,对输尿管口径较大的患儿更加困难。而且气膀胱建立对膀胱容量有一定要求,在膀胱容量小的患儿中似乎具有更高的并发症发生率,诸如操作时间长、手术难度大和学习曲线相对较长等缺点使气膀胱镜手术没有得到预期的普及[16]。但本组中2例(年龄分别为1.76月龄和3.8月龄)同样实施了手术,术中操作难度并未因患儿年龄小而明显增加,手术时间较年长儿稍有延长,但术后恢复是一样的。因此,笔者认为在操作技术熟练后,亦可尝试在较小婴儿中开展气膀胱Politano-Leadbetter输尿管再植术。
手术体会:对于所有类型的输尿管再植术,术中保持膀胱黏膜完整建立足够长的隧道、避免输尿管扭曲成角是手术成功的两个关键因素。笔者认为术前应根据造影结果了解输尿管迂曲程度并预判待游离长度,术中充分松解伸展输尿管、防止术后仍然迂曲导致尿液潴留也是手术关键所在,尤其是输尿管扩张显著的病例。以往的Politano-Leadbetter术在创建新的输尿管裂孔寻找膀胱外输尿管是此术式最难操作的部分,本术式沿输尿管在膀胱内投影,距输尿管口2.5~3.0 cm处与原输尿管口、尿道内口三点连线定位新的输尿管裂孔,可准确寻找膀胱外输尿管,手术成功率高,明显降低了此术式的难度。此外,气膀胱腹腔镜下输尿管再植术的瓶颈还包括输尿管裁剪、输尿管包埋以及输尿管直径过细时新输尿管口的建立,需要一定的腹腔镜手术技巧,但只要能够熟练操作Cohen术,结合本术式的新方法,气膀胱下Politano-Leadbetter术的学习曲线可明显缩短。考虑小儿本身发育特点以及输尿管伸缩性较大,有学者研究对比后认为术中裁剪与否对手术效果并无明显影响,除非输尿管过于扩张、远端输尿管过粗,以至无法建立适当比例的膀胱黏膜隧道[17]。当输尿管扩张严重时,应果断裁剪输尿管,5 - 0抗菌薇乔连续缝合,术后留置支架管。该术式能充分保证黏膜下隧道长度,而且由于更接近输尿管腹腔段,利于迂曲输尿管的彻底松解,保证输尿管的充分伸展。在建立新输尿管口(尤其是输尿管口径极细时),笔者建议用3 mm直角钳反复无损伤扩撑新开口,以防止结扎线捆绑更多管口组织,确保输尿管口组织的伸展,防止人为因素使输尿管口进一步变小。此外输尿管新入膀胱口处的操作应注意保护男童的输精管(或女童的输卵管)。
本术式为原位输尿管再植术,相较Cohen术更符合解剖生理,且隧道长度同样充裕,具有较好的抗反流性,可广泛应用于治疗各类膀胱输尿管连接部异常疾病。开展手术早期,虽然输尿管寻找经验不足会在一定程度上导致手术时间增加,但随着技术熟练,手术时间逐渐缩短。目前手术例数尚少,技术环节尚待进一步完善(如引入输尿管膀胱切口的更精准定位及寻找技巧等),相信随着该术式的逐渐完善将会越来越多地被采用,有效克服气膀胱Cohen术对上尿路疾病治疗的局限性。
| 1 |
Lakshmanan Y, Fung LC. Laparoscopic extravesicular ureteral reimplantation for vesicoureteral reflux:recent technical advances[J]. Endourol, 2000, 14: 589-593. DOI:10.1089/08927790050152203. |
| 2 |
Yeung CK, Sihoe JD, Borzi PA. Endoscopic cross-trigonal ureteral reimplantation under carbon dioxide bladder insufflation:a novel technique[J]. Endourol, 2005, 19: 295-299. DOI:10.1089/end.2005.19.295. |
| 3 |
Heidebreih A, Ozgur E, Becker T, et al. Surgical management of vesicoureteral reflux in pediatric patients[J]. World J Urol, 2004, 22(2): 96-106. DOI:10.1007/s00345-004-0408-x. |
| 4 |
Casale P, Patel RP, Kolon TF. Nerve sparing robotic extravesical ureteral reimplantation[J]. J Urol, 2008, 179(5): 1987-1990. DOI:10.1016/j.juro.2008.01.062. |
| 5 |
Lopez M, Varlet F. Laparoscopic extravesical transperitoneal approach following the Lich-Gregoir technique in the treatment of vesicoureteral reflux in children[J]. J Pediatr Surg, 2010, 45(4): 806-810. DOI:10.1016/j.jpedsurg.2009.12.003. |
| 6 |
毕允力, 阮双岁. 气膀胱腹腔镜输管移植术[J]. 中华小儿外科杂志, 2006, 27(2): 78-80. DOI:10.3760/cma.j.issn.0253-3006.2006.02.007. Bi YL, Ruan SS. Pneumocystoscopic Cohen ureteric reimplantation:a report of 11 cases[J]. Chin J Pediatr Surg, 2006, 27(2): 78-80. DOI:10.3760/cma.j.issn.0253-3006.2006.02.007. |
| 7 |
Krambeck AE, Gettman MT, BaniHani AH, et al. Management of nephrolithiasis after Cohen cross-trigonal and Glenn-Anderson advancement ureteroneocystostomy[J]. J Urol, 2007, 177(1): 174-178. DOI:10.1016/j.juro.2006.08.112. |
| 8 |
Liu X, Liu JH, Zhang DY, et al. Retrospective study to determine the short-term outcomes of a modified pneumovesical Glenn-Anderson procedure for treating primary obstructing megaureter[J]. J Pediatr Urol, 2015, 11(5): 266.e1-e6. DOI:10.1016/j.jpurol.2015.03.020. |
| 9 |
Chung MS, Han SW, Jung HJ, et al. Transvesicoscopic ureteral reimplantation in children with bilateral vesicoureteral reflux:surgical technique and results[J]. J Laparoendosc Adv Surg Tech A, 2012, 22(3): 295-300. DOI:10.1089/lap.2011.0318. |
| 10 |
曾莉, 黄一东, 康磊, 等. 改良Politano-Leadbetter术治疗儿童原发性输尿管膀胱连接处异常[J]. 中国修复重建外科杂志, 2015, 29(10): 1279-1283. DOI:10.7507/1002-1892.20150277. Zeng L, Huang YD, Kang L, et al. Modified Politano-Leadbetter technique for treating children with primary ureteral bladder junction abnormalities[J]. Chinese Journal of Reconstructive Surgery and Reconstruction, 2015, 29(10): 1279-1283. DOI:10.7507/1002-1892.20150277. |
| 11 |
Weiss DA, Shukla AR. The robotic-assisted ureteral reimplantation:the evolution to a new standard[J]. Urol Clin North Am, 2015, 42(1): 99-109. DOI:10.1016/j.ucl.2014.09.010. |
| 12 |
Grimsby GM, Dwyer ME, Jacobs MA, et al. Multi-institutional review of outcomes of robot-assisted laparoscopic extravesical ureteral reimplantation[J]. J Urol, 2015, 193(5 Suppl): 1791-1795. DOI:10.1016/j.juro.2014.07.128. |
| 13 |
Shigehiro S, Yoshitomo K, Takeshi S, et al. Transvesicoscopic ureteral reimplantation:Politano-Leadbetter versus Cohen technique[J]. Int J Urol, 2015, 22(4): 394-399. DOI:10.1111/iju.12702. |
| 14 |
刘颖, 毕允力. 气膀胱输尿管再植术治疗婴儿输尿管膀胱连接部梗阻临床分析[J]. 临床小儿外科杂志, 2014, 13(4): 287-290. DOI:10.3969/j.isn.1671-6353.2014.04.007. Liu Y, Bi YL. Clinical analysis of pneumovesicoscopy ureteral reimplantation for infantile vesicoureteral junction obstruction[J]. J Clin Ped Sur, 2014, 13(4): 287-290. DOI:10.3969/j.isn.1671-6353.2014.04.007. |
| 15 |
Valla JS, Steyaert H, Griffin SJ, et al. Transvesicoscopic Cohen ureteric reimplantation for vesicoureteral reflux in children:a single-centre 5-year experience[J]. J Pediatr Urol, 2009, 5(6): 466-471. DOI:10.1016/j.jpurol.2009.03.012. |
| 16 |
李怡, 张潍平, 杨庆林. 儿童原发性膀胱输尿管反流手术治疗的新进展[J]. 临床小儿外科杂志, 2019, 18(10): 805-810. DOI:10.3969/j.issn.1671-6353.2019.10.001. Li Y, Zhang WP, Yang QL. Recent advances of surgery for primary vesicoureteral reflux in children[J]. J Clin Ped Sur, 2019, 18(10): 805-810. DOI:10.3969/j.issn.1671-6353.2019.10.001. |
| 17 |
张潍平. 输尿管再植手术治疗原发输尿管反流[J]. 临床小儿外科杂志, 2014, 13(4): 341-343. DOI:10.3969/j.issn.1671-6353.2014.04.024. Zhang WP. Ureteral replantation surgery for primary ureteral reflux[J]. J Clin Ped Sur, 2014, 13(4): 341-343. DOI:10.3969/j.issn.1671-6353.2014.04.024. |
 2020, Vol. 19
2020, Vol. 19
