儿童尿路结石是一个棘手的临床问题。根据最新流行病学调查表明,西方国家儿童尿路结石的发病率呈逐年上升趋势[1-4]。在泌尿系统结石患儿中,70%以上为草酸钙结石,而婴儿中则以感染性结石多见[5]。由于儿童结石具有高复发率,其治疗与成人存在很大不同。迄今为止,体外冲击波碎石因其安全高效的特点仍是大部分儿童结石的首选治疗方式[6, 7]。近年来随着内镜技术的进步,更为纤细的输尿管软镜和经皮肾镜逐渐应用于儿童上尿路结石的治疗,取得良好的效果[8-10]。然而,部分合并先天畸形、感染或者多发、铸型的复杂性上尿路结石患儿,单一采用体外冲击波碎石术或内镜碎石难以取得理想的治疗效果。本文旨在通过回顾性分析采用双镜联合方式治疗的9例复杂性上尿路结石患儿的治疗过程,探讨双镜联合方式在儿童复杂性上尿路结石治疗中的可行性及安全性。
材料与方法 一、临床资料回顾性分析2017年1月至2020年1月由上海交通大学医学院附属上海儿童医学中心收治的9例复杂性上尿路结石患儿临床资料,其中男童7例,女童2例;平均(45±47)个月,中位年龄27个月。结石最大直径平均(8±6)mm。5例输尿管末端狭窄合并肾结石患儿行腹腔镜下输尿管再植术联合输尿管软镜下钬激光碎石取石术;1例右肾重复畸形下半肾积水合并结石行腹腔镜下下半肾肾盂成形术联合输尿管软镜下钬激光碎石取石术;1例双侧输尿管结石伴右肾重度积水行左侧输尿管软镜下钬激光碎石术联合右侧腹腔镜下切开取石离断成形术;1例肾盂输尿管连接部狭窄合并下盏结石行F11超细经皮肾镜碎石取石术联合腹腔镜下肾盂成形术;1例鹿角状结石患儿行F14微通道经皮肾镜联合输尿管软镜钬激光碎石术。具体临床资料见表 1。
|
|
表 1 9例复杂性上尿路结石患儿的临床资料 Table 1 Clinical profiles of 9 children with complicated upper urinary calculi |
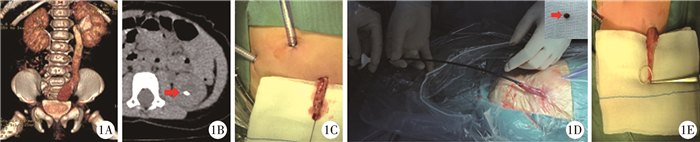
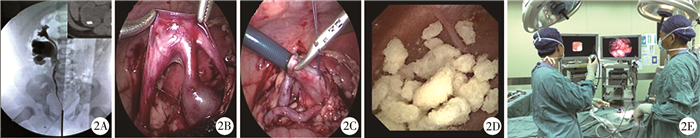
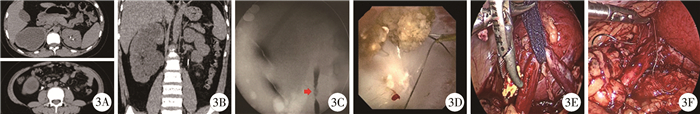
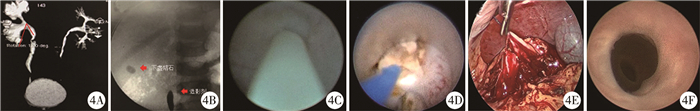
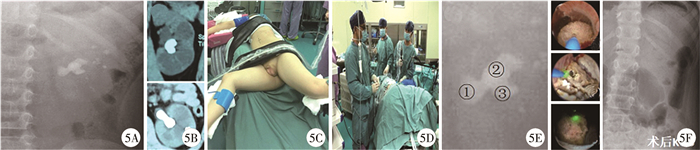
① 输尿管末端狭窄合并肾结石患儿采用平卧位,经脐部穿刺套管置入观察镜。游离输尿管末端至膀胱壁内段后切断,将输尿管自同侧腹壁穿刺孔提出体外(图 1A、图 1B、图 1C)。将F9.5/11.5输尿管软镜鞘自输尿管末端插入至肾脏,并导入输尿管软镜行碎石取石术(图 1D)。取石结束后裁剪输尿管末端,将输尿管重新回纳腹腔后完成输尿管再植术(图 1E)。②肾重复畸形下半肾积水合并结石患儿采用平卧位,患侧垫高45°。经脐部穿刺套管置入观察镜。游离下半肾肾盂输尿管,切开肾盂(图 2B、图 2C)。自下腹部穿刺套管引入F12/14输尿管鞘至腹腔内,并自肾盂切口插入至下半肾集合系统。导入输尿管软镜行碎石取石术(图 2D、图 2E)。随后在腹腔镜下完成下半肾肾盂成形术。③双侧输尿管结石伴右肾重度积水患儿于外院留置左侧DJ管后转入我院(右侧置管失败)(图 3A、图 3B)。入院检查提示右侧分肾功能仅30%。完成左侧输尿管软镜下碎石术后(图 3D),行右侧造影发现右侧输尿管结石上下方输尿管壁狭窄,输尿管导管及黑泥鳅导丝均无法跨过结石,考虑为嵌顿性结石(图 3C),遂改平卧位行腹腔镜下右侧输尿管切开取石术,术中纵向切开输尿管见结石周围输尿管肉芽增生包裹,夹出结石后将嵌顿段输尿管切除再吻合(图 3E、图 3F)。④肾盂输尿管连接部狭窄合并下盏结石患儿因发热性尿路感染行B超检查发现右肾结石合并右肾积水。术前CT提示肾盂输尿管连接部存在明显腔内狭窄,结石位于肾下盏内,且肾盂肾下盏漏斗夹角(infundibulopelvic angle,IPA)较小(图 4A)。入手术室后首先在截石位下行逆行造影见造影剂无法逆行通过肾盂输尿管连接部(ureteropelvic junction,UPJ),集合系统不显影(图 4B)。输尿管镜检查见UPJ几乎闭锁,无法通过F3输尿管导管(图 4C)。遂改俯卧位在第11肋间穿刺下盏,成功扩张至F11超细通道完成钬激光碎石取石术(图 4D)。同时顺行探查UPJ,见UPJ几近闭锁,球囊扩张后由肾镜进入输尿管。探查发现狭窄段输尿管为腔内狭窄,长度约0.5 cm。遂改平卧位行腹腔镜下肾盂输尿管成形术(图 4E)。术后3个月拔除DJ管重新探查见吻合口宽敞(图 4F)。⑤鹿角状结石患儿术前经CT平扫提示结石主体位于肾盂及中盏,部分结石深入下盏,下盏的IPA夹角较小(图 5A、图 5B)。故采用侧卧截石体位在输尿管软镜下清除肾盂结石及肾中盏结石,同时在第12肋下成功穿刺肾下盏,扩张至F14微通道后成功清除肾下盏结石(图 5C~图 5F)。术后留置F3输尿管导管,1 d后拔管复查腹部平片未见明显结石残留(图 5G)。
|
Download:
|
| 图 1 腹腔镜下输尿管再植术联合输尿管软镜碎石术 Fig. 1 Laparoscopic ureteral replantation plus flexible ureteroscopic lithotripsy | |
|
Download:
|
| 图 2 腹腔镜下肾盂成形术联合输尿管软镜碎石术 Fig. 2 Laparoscopic pyeloplasty plus flexible ureteroscopic lithotripsy | |
|
Download:
|
| 图 3 腹腔镜下右侧输尿管切开取石离断成形联合对侧输尿管软镜取石术 Fig. 3 Laparoscopic ureterotomy and lithotomy (right) plus flexible ureteroscopic lithotripsy (left) | |
|
Download:
|
| 图 4 腹腔镜下肾盂成形术联合经皮肾镜碎石术 Fig. 4 Laparoscopic pyeloplasty plus percutaneous nephrolithotripsy | |
|
Download:
|
| 图 5 经皮肾镜碎石术联合输尿管软镜碎石术 Fig. 5 Percutaneous nephrolithotripsy plus flexible ureteroscopic lithotripsy | |
9例患儿均成功完成手术并取净结石,平均手术时间为(138± 37)min,且无明显手术相关并发症。5例输尿管末端狭窄合并肾结石患儿结石成分均为草酸钙,术后随访期间未见结石复发。1例重复肾下半肾积水患儿结石成分为草酸钙,术后随访期间未见结石复发。1例双侧输尿管结石伴右肾重度积水患儿结石成分为尿酸,目前该患儿尚未拔除DJ管。1例肾盂输尿管连接部狭窄合并肾下盏结石患儿结石成分为碳酸磷灰石和一水草酸钙,随访至今未见复发。1例鹿角状结石患儿结石成分为草酸钙,随访1年后结石复发。
讨 论迄今为止,体外冲击波碎石术仍是儿童结石治疗的首选。近年越来越纤细的输尿管软镜和经皮肾镜的应用给儿童上尿路结石的治疗提供了更多选择。其中输尿管软镜经过尿道进行手术,具有损伤小、可重复等优点。研究表明,输尿管软镜下碎石取石术可安全高效地应用于上尿路结石<2 cm的婴幼儿[11]。而经皮肾镜取石术是2 cm以上肾结石的治疗方法之一。随着F14~F16微通道经皮肾镜,F11~F13超微通道经皮肾镜,F4.85针式肾镜的普及应用,经皮肾镜取石术的出血风险日趋下降,在儿童中的应用也更为安全[12]。除此以外,腹腔镜下切开取石在儿童结石治疗中并不能作为一种常规治疗方式,仅限于部分嵌顿性输尿管结石或常规治疗失败的补救手段[13, 14]。然而,部分复杂性结石患儿采用单一手段无法取得理想的治疗效果,包括合并先天畸形的上尿路结石、反复尿路感染继发的上尿路结石、鹿角状结石等。
先天性输尿管末端狭窄是导致肾积水的第二个常见病因[15]。输尿管梗阻导致尿液瘀滞浓缩,容易继发上尿路结石[16]。普通的腹腔镜下输尿管再植术无法同时处理合并的肾结石。在再植术中往往需要将输尿管末端提出切口进行裁剪,这为经皮软镜的实施提供了可行性。本研究5例患儿将输尿管末端自同侧Trocar穿刺孔提出腹壁,通过排空气腹以及向脚侧牵引输尿管可使输尿管近端趋近于平直。此时可以不需要导丝的引导直接将输尿管软镜鞘自输尿管末端开口插入至集合系统,导入输尿管软镜后将集合系统结石取出。这类继发结石多为尿液瘀滞浓缩形成的含钙结石。输尿管末端狭窄治愈,上尿路尿流动力学引流恢复正常后结石往往不易复发。
肾盂输尿管连接部狭窄合并肾结石是临床常见的问题。有研究表明采用腹腔镜同时完成肾盂成形术和取石术是可行的,不仅可以重建肾盂输尿管连接部,且该术式结石清除率高[17]。然而在肾脏异位、盏颈细长或多发结石、下盏结石等特殊情况下腹腔镜难以取净集合系统结石。此时则需要联用输尿管软镜或经皮肾镜提高取石效率[18, 19]。本研究中腹腔镜联用输尿管软镜治疗重复肾下半肾积水合并肾结石、腹腔镜联用经皮肾镜治疗肾积水合并下盏结石均取得了良好的效果。由于该类结石多为继发于尿路梗阻的草酸钙结石,故矫正肾盂输尿管连接部狭窄后,结石复发率低。
儿童输尿管嵌顿性结石并不多见,处理却最为棘手[20, 21]。输尿管嵌顿性结石可以导致结石周围黏膜肉芽增生,造成输尿管瘢痕狭窄并最终导致肾积水。对于儿童肾盂输尿管连接部嵌顿性结石合并肾积水,往往无法区分结石和狭窄的原发顺序[17]。与普通输尿管结石处理不同,嵌顿性结石的处理常常需要同时切除瘢痕段输尿管。对于儿童输尿管嵌顿性结石,术前提前预警尤为重要。对于病史较长、结石长时间未移动、周围管壁明显增厚或插管失败等情况均应考虑存在嵌顿性结石的可能性[22]。因此,本研究中图 3所示的右侧输尿管嵌顿性结石患儿入院后即和家属交代了可能需行右侧输尿管离断成形术,术中造影和腹腔镜下所见均证实了嵌顿性结石的诊断。
鹿角状结石在儿童中相对少见,随着经皮肾镜和高效碎石工具在儿童中的推广,绝大部分鹿角状结石可以通过标准单通道或者多个微通道Ⅰ期清除结石[23, 24]。本研究中图 5所示的鹿角状结石患儿在取侧卧截石位之前,首先在常规截石位下进行了输尿管镜检查,术中发现输尿管较为松弛,可直接上镜至集合系统。故退镜改体位为侧卧截石位,软镜下清除肾盂及中盏结石主体的同时联用微通道经皮肾镜清除下盏结石。该方式的优点是尽可能缩小了皮肾通道的型号以及数量,减轻了肾脏的穿刺损伤。
随着经皮肾镜和软镜的迭代改进以及各类碎石工具的应用,儿童上尿路结石的治疗逐渐变得微创和高效。对于复杂性结石的处理,不仅需要积极探索多镜联合的可行性,术后预防结石复发仍然同样重要。本研究纳入病例数较少,双镜联合治疗儿童复杂上尿路结石的可行性仍需要进一步增加病例数来证实。
| 1 |
Tasian GE, Ross ME, Song L, et al. Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012[J]. Clin J Am Soc Nephrol, 2016, 11(3): 488-496. DOI:10.2215/CJN.07610715. |
| 2 |
Sas DJ, Hulsey TC, Shatat IF, et al. Increasing incidence of kidney stones in children evaluated in the emergency department[J]. J Pediatr, 2010, 157(1): 132-137. DOI:10.1016/j.jpeds.2010.02.004. |
| 3 |
Bush NC, Xu L, Brown BJ, et al. Hospitalizations for pediatric stone disease in United States, 2002-2007[J]. J Urol, 2010, 183(3): 1151-1156. DOI:10.1016/j.juro.2009.11.057. |
| 4 |
Novak TE, Lakshmanan Y, Trock BJ, et al. Sex prevalence of pediatric kidney stone disease in the United States:an epidemiologic investigation[J]. Urology, 2009, 74(1): 104-107. DOI:10.1016/j.urology.2008.12.079. |
| 5 |
Kirejczyk JK, Porowski T, Filonowicz R, et al. An association between kidney stone composition and urinary metabolic disturbances in children[J]. J Pediatr Urol, 2014, 10(1): 130-5. DOI:10.1016/j.jpurol.2013.07.010. |
| 6 |
Akin Y, Yucel S. Long-term effects of pediatric extracorporeal shockwave lithotripsy on renal function[J]. Res Rep Urol, 2014, 6: 21-25. DOI:10.2147/RRU.S40965.eCollection2014. |
| 7 |
Aksoy Y, Ozbey I, Atmaca AF, et al. Extracorporeal shock wave lithotripsy in children:experience using a mpl-9000 lithotriptor[J]. World J Urol, 2004, 22(2): 115-119. DOI:10.1007/s00345-003-0385-5. |
| 8 |
Farouk A, Tawfick A, Shoeb M, et al. Is mini-percutaneous nephrolithotomy a safe alternative to extracorporeal shockwave lithotripsy in pediatric age group in borderline stones? a randomized prospective study[J]. World J Urol, 2018, 36(7): 1139-1147. DOI:10.1007/s00345-018-2231-9. |
| 9 |
Sarica K, Eryildirim B, Tuerxun A, et al. Super-mini percutaneous nephrolithotomy for renal stone less than 25mm in pediatric patients:Could it be an alternative to shockwave lithotripsy?[J]. Actas Urol Esp, 2017, 19(17): 30224-30223. DOI:10.1016/j.acuro.2017.08.005. |
| 10 |
Li JH, Yu HQ, Zhou P, et al. Application of flexible ureteroscopy combined with holmium laser lithotripsy and their therapeutic efficacy in the treatment of upper urinary stones in children and infants[J]. Urol J, 2019, 16(4): 343-346. DOI:10.22037/uj.v0i0.4640. |
| 11 |
李钧, 肖荆, 陈恒润, 等. 输尿管软镜钬激光碎石术治疗儿童和婴幼儿上尿路结石:单中心92例经验总结[J]. 中华泌尿外科杂志, 2016, 37(11): 851-854. DOI:10.3760/cma.j.issn.1000-6702.2016.11.016. Li J, Xiao J, Chen HR, et al. Flexible ureteroscopy and holmium laser lithotripsy for children and infants with upper urinary stones:single-center experience of 92 cases[J]. Chin J Urol, 2016, 37(11): 851-854. DOI:10.3760/cma.j.issn.1000-6702.2016.11.016. |
| 12 |
石博文, 徐科, 黄云腾. 经皮肾镜取石术在儿童肾结石中的应用及进展[J]. 临床小儿外科杂志, 2017, 16(6): 617-621. DOI:10.3969/j.issn.1671-6353.2017.06.021. Shi BW, Xu K, Huang YT. Application and progress in percutaneous nephrolithotomy for pediatric kidney stones[J]. J Clin Ped Sur, 2017, 16(6): 617-621. DOI:10.3969/j.issn.1671-6353.2017.06.021. |
| 13 |
Srivastava A, Dhayal IR, Rai P. Laparoscopic ureterolithotomy in children:with and without stent-initial tertiary care center experience with more than 1-year follow-up[J]. Eur J Pediatr Surg, 2017, 27(2): 150-154. DOI:10.1055/s-0036-1572551. |
| 14 |
Casale P, Grady RW, Joyner BD, et al. Transperitoneal laparoscopic pyelolithotomy after failed percutaneous access in the pediatric patient[J]. J Urol, 2004, 172(2): 680-683. DOI:10.1097/01.ju.0000129462.23322.e0. |
| 15 |
Brown T, Mandell J, Lebowitz RL. Neonatal hydronephrosis in the era of sonography[J]. AJR Am J Roentgenol, 1987, 148(5): 959-963. DOI:10.2214/ajr.148.5.959. |
| 16 |
Tenkorang S, Omana JP, Mellas S, et al. Urolithiasis secondary to primary obstructive megaureter in an adult:a case report[J]. J Med Case Rep, 2017, 11(1): 177. DOI:10.1186/s13256-017-1342-z. |
| 17 |
Skolarikos A, Dellis A, Knoll T. Ureteropelvic obstruction and renal stones:etiology and treatment[J]. Urolithiasis, 2015, 43(1): 5-12. DOI:10.1007/s00240-014-0736-2. |
| 18 |
Yin Z, Wei YB, Liang BL, et al. Initial experiences with laparoscopy and flexible ureteroscopy combination pyeloplasty in management of ectopic pelvic kidney with stone and ureter-pelvic junction obstruction[J]. Urolithiasis, 2015, 43(3): 255-260. DOI:10.1007/s00240-015-0753-9. |
| 19 |
Yang C, Zhou J, Lu ZX, et al. Simultaneous treatment of ureteropelvic junction obstruction complicated by renal calculi with robotic laparoscopic surgery and flexible cystoscope[J]. World J Urol, 2019, 37(10): 2217-2223. DOI:10.1007/s00345-018-2608-9. |
| 20 |
Adanur S, Aydin HR, Ozkaya F, et al. Holmium laser lithotripsy with semi-rigid ureteroscopy:a first-choice treatment for impacted ureteral stones in children?[J]. Med Sci Monit, 2014, 20: 2373-2379. DOI:10.12659/msm.891173. |
| 21 |
Akhtar J, Ahmed S, Zamir N. Management of impacted urethral stones in children[J]. J Coll Physicians Surg Pak, 2012, 22(8): 510-513. DOI:08.2012/JCPSP.510513. |
| 22 |
Tran TY, Bamberger JN, Blum KA, et al. Predicting the impacted ureteral stone with computed tomography[J]. Urology, 2019, 130: 43-47. DOI:10.1016/j.urology.2019.04.020. |
| 23 |
Rashid AO, Amin SH, Al Kadum MA, et al. Mini-percutaneous nephrolithotomy for complex staghorn stones in children[J]. Urol Int, 2019, 102(3): 356-359. DOI:10.1159/000499491. |
| 24 |
Purkait B, Kumar M, Sokhal AK, et al. Percutaneous nephrolithotomy of bilateral staghorn renal calculi in pediatric patients:12 years experience in a tertiary care centre[J]. Urolithiasis, 2017, 45(4): 393-399. DOI:10.1007/s00240-016-0920-7. |
 2020, Vol. 19
2020, Vol. 19


