2. 中南大学湘雅二医院超声科(湖南省长沙市, 410007)
2. Department of Ultrasound the second Xiangya Hospital of central south university, Changsha 410007, China
Berry综合征是一种非常罕见的心血管组合畸形,主要包括主动脉-肺动脉间隔缺损(aortopulmonary septal defect, APSD)、右肺动脉异常起源于主动脉(aortic origin of right pulmonary artery, AORPA)、主动脉弓离断(interruption of aortic arch, IAA)或主动脉弓狭窄(coarctation of aorta, COA),其室间隔完整,常合并动脉导管未闭(patent ductus arteriosus, PDA)、房间隔缺损或卵圆孔未闭[1-5]。如未能及时发现,容易导致患儿早期合并肺动脉高压,严重者可在新生儿期及婴幼儿期死亡[6-8]。彩色多普勒超声心动图因具有操作简单、无创、检查成本低等优势,是目前公认的先天性心血管疾病主要诊断方法之一。本研究旨在初步总结Berry综合征彩色多普勒超声心动图特点。
材料与方法 一、研究对象收集2010年4月至2019年11月在湖南省儿童医院经超声心动图诊断为Berry综合征的8例患儿为研究对象,所有病例经CT血管成像或手术确诊,其中男童5例,女童3例;年龄1~12个月,平均(4.06±3.72)个月;体重2.5~4.6 kg,平均(3.5±1.8)kg。
二、仪器与方法采用PHILIPS IE33型及PHILIPS EPIQ 7C型彩色多普勒超声心动图诊断仪,配S5-1、S8-3、X7-2探头, 频率2.5~7.5MHz。除常规扫查切面外,重点扫查大动脉短轴切面、右室流出道肺动脉长轴切面、胸骨上窝主动脉弓长轴切面、剑突下切面等,仔细观察主动脉与肺动脉的间隔连续情况,肺动脉主干走形及左、右肺动脉分支起源,主动脉弓顶端分支结构及远端与降主动脉延续情况等。
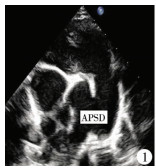
结 果 一、彩色多普勒超声心动图结果8例中7例直接提示Berry综合征,1例提示动脉导管未闭,主动脉弓狭窄,其共性如下:①二维超声心动图显示左心室、右心室不同程度增大,肺动脉主干增宽,肺动脉主干远端近分叉处的右侧壁与主动脉左侧壁之间无分隔,右肺动脉大部分或全部起源于主动脉左后壁,呈“蝴蝶征”(图 1)。主动脉弓于左锁骨下动脉水平发出3个分支,远端闭锁7例,呈“鹿角征”(图 2),1例为主动脉弓狭窄。8例患儿主动脉与肺动脉之间可见导管交通。室间隔连续且完整。②彩色多普勒显示主动脉与肺动脉之间主干可见暗淡交通血流信号,呈红色、蓝色或红蓝双色血流信号,其中1例漏诊,主动脉与肺动脉之间间隔缺损分流信号不明显。右肺动脉血流全部或部分来源于升主动脉,胸骨上窝主动脉弓长轴切面显示主动脉弓血流与顶端3根分支血流连续,远端未见明显与降主动脉血流延续。降主动脉与肺动脉主干左侧可见暗淡蓝色交通血流,8例均合并轻至中度三尖瓣反流信号。③频谱多普勒显示主动脉与肺动脉主干之间间隔缺损处呈双向湍流频谱,降主动脉与肺动脉之间导管内可见负向湍流频谱。通过频谱及三尖瓣反流速度估测8例均合并肺动脉高压、7例合并卵圆孔未闭。
|
Download:
|
| 图 1 主动脉与肺动脉间隔缺损,右肺动脉起源主动脉,主动脉、右肺动脉及肺动脉主干、左肺动脉构成“蝴蝶征” Fig. 1 Aortic and pulmonary artery septal defect.Right pulmonary artery originated from the aorta.Aorta, right pulmonary artery, main pulmonary artery and left pulmonary artery constituted the "butterfly sign" | |

|
Download:
|
| 图 2 主动脉弓离断,主动脉弓顶端分出分支,分支比较紧密,远端不延续,呈“鹿角征” Fig. 2 Aortic arch was broken, the top of aortic arch branched off, the branches were relatively dense and distal end was discontinuous, showing an "antler sign" | |
8例均进行了CT血管重建,其中7例与超声诊断完全符合,1例术前超声检查过程中因患儿哭吵造成主动脉与肺动脉之间间隔缺损分流不明显而未能确诊,外科医师申请CT进一步检查后明确诊断为Berry综合征。8例Berry综合征中7例经手术治疗痊愈出院,除1例4个月男童因合并重度肺动脉高压、重症肺炎、呼吸衰竭于术前死亡外,其余均手术,术中发现远端型APSD 7例、AORPA 7例、A型IAA 6例、COA 1例、合并肺动脉高压(pulmonary hypertension, PH)7例、卵圆孔未闭(patent foramen oval,PFO)6例、三尖瓣反流(tricuspid regurgitation,TR)7例。详见表 1。
|
|
表 1 8例Berry综合征患儿一般情况、超声、CT、是否手术及预后 Table 1 General profiles, ultrasound, CT, surgery and prognosis of 8 children |
Berry综合征是一组复杂罕见心血管畸形组合,发病人数约占先天性心脏病的0.46‰,据报道该病与13号染色体之间存在一定关联[9, 10]。本研究8例患儿有6例进行染色体检查,结果未见明显异常,估计与样本例数少有关。自胚胎发育第5周开始,动脉干远端内膜演变成动脉干嵴将动脉干远端分隔成升主动脉及肺动脉;第Ⅵ对弓演变成左、右肺动脉,连接肺动脉侧,在发展过程中,如动脉干远端的嵴未将主动脉与肺动脉分隔开,导致远端型主动脉与肺动脉间隔缺损,同时第Ⅵ对弓迁徙异常,导致右肺动脉起源于升主动脉,肺动脉主干远端延续为左肺动脉;因升主动脉一部分血液直接流入右肺动脉,而室间隔完整,主动脉的血流只来自左心室,无其他来源,使流入主动脉弓血流明显减少,主动脉弓被“窃血”,导致主动脉弓离断或狭窄。
该组畸形主要包括APSD、AORPA、IAA或COA、室间隔完整,常合并PH、PDA、PFO等。本研究8例患儿中7例术前经彩色多普勒超声心动图确诊,1例检查时非安静状态,超声仅仅提示动脉导管未闭、主动脉弓缩窄,但临床血氧饱和度低,呼吸困难,发绀无法解释,外科医师申请CT血管重建,提示Berry综合征。根据缺损口的位置,可将APSD分为3型:Ⅰ型又名近端型,主动脉与肺动脉之间间隔缺口位于升主动脉与肺动脉主干的根部,靠近两组半月瓣,距离肺动脉分叉较远,此型最常见,约占70%;Ⅱ型为远端型,缺口位于升主动脉与肺动脉远端,临近肺动脉分叉,约占25%,易出现AORPA,超声心动图声像表现右肺动脉起源于升主动脉左后方或骑跨在主肺动脉间隔缺损上,大部分起源主动脉,呈“蝴蝶征”,主动脉与后方发出的右肺动脉像蝴蝶的左翅膀;肺动脉主干及其延续的左肺动脉像蝴蝶的右翅膀,此征像具有特异性,而本研究的8例Berry综合征患儿均为Ⅱ型APSD并AORPA;Ⅲ型为混合型,缺口大,升主动脉与肺动脉之间无间隔,类似共同动脉干,约占5%,此型与共同动脉干主要鉴别点为共同动脉干只有一组半月瓣,而Ⅲ型APSD存在两组半月瓣[11]。根据主动脉弓离断位置,将IAA分为3型:A型为常见型,离断位置位于左锁骨下动脉远端,本次研究7例Berry综合征患儿的IAA均为A型,1例主动脉弓狭窄,狭窄处位于主动脉弓峡部;B型,主动脉弓离断位置位于左颈总动脉与左锁骨下动脉之间;C型,离断位置位于头臂干与左颈总动脉之间[12]。
由于该病同时存在或合并APSD、AORPA、PDA、PFO等心内分流,缺口比较大,存在大量左向右分流,致新生儿期出现严重肺动脉高压,如果未能得到及时救治,患儿将死于充血性心力衰竭、重症肺炎、呼吸衰竭等。因此早期诊断,及时手术治疗对Berry综合征的预后尤为重要[13, 15]。彩色多普勒超声心动图以其无创、方便、经济、操作灵活作为筛查先天性心脏疾病的首选方法,通过获取胸骨旁左室长轴切面,二尖瓣短轴切面、大动脉短轴切面、心尖四腔、五腔切面、剑突下两房切面等,结合心脏三节段分析法,分析心房与心室关系、心室与大动脉关系、主动脉与肺动脉关系、房室间隔及瓣膜情况,从而准确作出心脏疾病超声诊断,由于Berry综合征患儿出生后早期合并肺动脉高压,主动脉与肺动脉压差接近,主动脉与肺动脉间隔缺损处血流缓慢、颜色暗淡,且超声声束方向与缺损口完全平行,故容易漏诊[16, 18]。本次研究中1例12个月患儿因非安静状态检查,合并肺动脉高压,主动脉与肺动脉间隔回声失落及彩色血流分流不明显,从而漏诊APSD、AORPA,仅仅诊断为主动脉弓缩窄、动脉导管未闭、肺动脉高压,最终通过CT血管造影确诊为Berry综合征,经手术治疗痊愈出院,分析原因主要以下两点:一方面超声诊断医师对该疾病的诊断经验不足,另一方面是由于大动脉短轴切面主动脉与肺动脉间隔缺口与声束线方向平行,导致假阴性结论,因此对于哭吵患儿应先行常规镇静,待安静后再行检查;对于不明原因的肺动脉高压,用单纯的动脉导管未闭、房间隔缺损、卵圆孔未闭无法解释时,要多切面连续顺序扫查,除需获得以上描述的必须的标准切面外,还要结合非标准切面,重复扫查,调节合适灰度及彩色增益,或请多个医师会诊,做出准确诊断,减少误诊、漏诊的概率。由于主动脉弓离断或缩窄,降主动脉供血不足,需要依靠动脉导管或侧支循环供血,故导管一般较粗大,由于主动脉弓离断,故血流自肺动脉方向流至降主动脉,呈暗淡蓝色血流,频谱多普勒显示负向单期或连续湍流频谱,此时应注意将彩色多普勒增益调高,速度标尺调低,并结合右室流出道、肺动脉长轴切面及胸骨上窝高位动脉导管切面仔细扫查。胸骨上窝主动脉弓长轴切面的获取亦非常重要,此切面可以清晰地显示升主动脉后方是否发出右肺动脉,主动脉弓形态,顶端三个分支情况,主动脉弓离断或缩窄的位置,主动脉弓内下缘是否存在体肺侧支循环,数目多少。总之,术前充分的超声心动图评估对手术顺利实施具有重要的指导意义。
Senzaki等[19]报道1例Berry综合征患儿的左冠状动脉异常起源于肺动脉,术前未确诊,术后死于心源性休克。上海儿童医学中心胡仁杰等[20]曾报道19例Berry综合征患儿的外科治疗情况,术后3例死亡,未见明显冠状动脉起源异常。而本组患儿左、右冠状动脉起源及主干走形未见明显异常,但提示超声医师对于心脏多发、复杂畸形患儿,应注意关注冠状动脉起源及走形,做好充分的术前评估,提高手术成功率。
虽然彩色多普勒超声心动图能直观多切面扫查心脏结构,提供丰富血流信息,可诊断绝大部分心脏畸形,但不可否认其存在以下局限性,如重症肺炎患儿,因气体干扰严重,胸骨旁切面无法清晰获得;肥胖患儿经胸超声心动图切面显示不满意;主动脉弓长轴切面对侧支循环的显示与操作者的手法及认识程度有关。对于以上情况,建议补充食管超声心动图或CT血管重建检查,CT对于心脏周围血管、空间位置的显示明显强于超声心动图,但其存在电离辐射,并且不能动态显示心内大血管内血流方向、流速等信息,对瓣膜的反流速度、跨瓣压差的估计及肺动脉高压程度的判断缺乏量化指标;高档MRI成像技术近年来广泛应用于先天性心脏病的诊断,其优点是图像清晰,分辨率高,尤其在冠状动脉疾病诊断方面具有优势,但是其缺点如操作时间长,图像后处理、心功能分析较繁琐,检查费用高等,使该检查方法广泛应用于临床受制约。综合各种检查优缺点,不难得出彩色多普勒超声心动图是诊断Berry综合征的首选筛查方法,对于疑似病例,建议行CT血管重建或者MRI成像检查,以提高对该病诊断符合率,为手术方式的选择提供重要指导。
| 1 |
Li W, Bin G, Jiang W, et al. Prenatal diagnosis of aortopulmonary window by 2-dimensional echocardiography:summary of 8 cases[J]. J Ultrasound Med, 2019, 38(3): 795-803. DOI:10.1002/jum.14756. |
| 2 |
Bu H, Zhao T. Berry syndrome diagnosed by three-dimensional computed tomographic angiography[J]. Acta Cardiol, 2020, 75(2): 160-161. DOI:10.1080/00015385.2018.1557408. |
| 3 |
Zhang X, Liu XW, Gu XY, et al. Prenatal diagnosis of Berry syndrome by fetal echocardiography:A report of four cases[J]. Echocardiography, 2018, 35(4): 563-565. DOI:10.1111/echo.13832. |
| 4 |
Kumar SR. A potential window into surgical outcomes for Berry syndrome[J]. J Thorac Cardiovasc Surg, 2017, 153(5): 1148. DOI:10.1016/j.jtcvs.2017.01.041. |
| 5 |
Remon JI, Briston DA, Stern KW. Berry syndrome:the importance of genetic evaluation before surgical intervention[J]. Cardiol Young, 2016, 26(1): 188-190. DOI:10.1017/S1047951115000256. |
| 6 |
徐彦成, 刘祎秀, 杨静. 6例主肺动脉窗合并主动脉弓离断的超声心动图及心脏造影诊断价值[J]. 中国心血管病研究, 2018, 16(9): 816-819. DOI:10.3969/j.issn.1672-5301.2018.09.010. Xu YC, Liu YX, Yang J. Diagnostic value of ultrasound and cardiac angiography in 6 cases of aorto-pulmonary window combined with interrupted aortic arch[J]. Chinese Journal of Cardiovascular Research, 2018, 16(9): 816-819. DOI:10.3969/j.issn.1672-5301.2018.09.010. |
| 7 |
赵梦峤, 任卫东, 胡金玲. 7例主肺间隔缺损患者超声特征分析[J]. 中国医科大学学报, 2018, 47(2): 171-174. DOI:10.12007/j.issn.02584646.2018.02.017. Zhao MJ, Ren WD, Hu JL. Characterization of ultrasonic echocardiography in seven patients with aortopulmonary septal defect[J]. Journal of China Medical University, 2018, 47(2): 171-174. DOI:10.12007/j.issn.02584646.2018.02.017. |
| 8 |
缪伟, 姜伊娜, 王翠翠. Berry综合征产前超声心动图表现1例[J]. 中国临床医学影像杂志, 2017, 28(1): 48. DOI:10.3969/j.issn.1008-1062.2017.01.013. Liao W, Jiang YN, Wang CC. Prenatal echocardiographic findings of Berry syndrome:report of one case[J]. Journal of China Clinic Medical Imaging, 2017, 28(1): 48. DOI:10.3969/j.issn.1008-1062.2017.01.013. |
| 9 |
王佳莉, 任卫东, 胡金玲. 超声心动图诊断罕见Berry综合征二例[J]. 中华医学超声杂志(电子版), 2017, 14(3): 239-240. DOI:10.3877/cma.j.issn.1672-6448.2017.03.015. Wang JL, Ren WD, Hu JL. Echocardiographic diagnosis of rare Berry syndrome:a report of two cases[J]. Chinese Journal of Medical Ultrasound (Electronic Edition), 2017, 14(3): 239-240. DOI:10.3877/cma.j.issn.1672-6448.2017.03.015. |
| 10 |
Berry TE, Bharati S, Muster AJ, et al. Distal aortopulmonary septal defect, aortic origin of the right pulmonary artery, intact ventricular septum, patent ductus arteriosus and hypoplasia of the aortic isthmus:a newly recognized syndrome[J]. Am J Cardiol, 1982, 49(1): 108-116. DOI:10.1016/0002-9149(82)90284-3. |
| 11 |
Soquet J, Barron DJ, d'Udekem Y. A review of the management of pulmonary atresia, ventricular septal defect and major aortopulmonary collateral arteries[J]. Ann Thorac Surg, 2019, 108(2): 601-612. DOI:10.1016/j.athoracsur.2019.01.046. |
| 12 |
Talwar S, Agarwal P, Choudhary SK, et al. Aortopulmonary window:morphology, diagnosis, and long-term results[J]. Journal of Cardiac Surgery, 2017, 32(2): 138-144. DOI:10.1111/jocs.12936. |
| 13 |
Friedman, Kevin. Preoperative physiology, imaging, and management of interrupted aortic arch[J]. Seminars in Cardiothoracic & Vascular Anesthesia, 2017, 22(3): 265-269. DOI:10.1177/1089253218770198. |
| 14 |
Houssa MA, Atmani N, Bamous M, et al. Persistence of the 5th Aortic Arch Associated With Interruption of the Aortic Arch[J]. Pan Afr Med J, 2017, 27: 265. DOI:10.11604/pamj.2017.27.265.4249. |
| 15 |
Ghelani SJ, Quinonez LG, Rathod RH. Prenatal diagnosis and management of Berry syndrome, a rare conotruncal anatomy[J]. Circulation, 2015, 132(16): 1593-1594. DOI:10.1161/CIRCULATIONAHA.115.017366. |
| 16 |
Jayaram N, Knowlton J, Shah S, et al. Berry syndrome:a possible genetic link[J]. Pediatr Cardiol, 2013, 34(6): 1511-1513. DOI:10.1007/s00246-012-0412-7. |
| 17 |
Presnell LB, Blankenship A, Cheatham SL, et al. An overview of pulmonary atresia and major aortopulmonary collateral arteries[J]. World J Pediatr Congenit Heart Surg, 2015, 6(4): 630-639. DOI:10.1177/2150135115598559. |
| 18 |
Morito H, Masuzawa A, Kobayashi J, et al. One-stage surgical repair for Berry syndrome with preoperative diagnosis by 3-dimensional CT[J]. World J Pediatr Congenit Heart Surg, 2011, 2(3): 491-494. DOI:10.1177/2150135111405347. |
| 19 |
Senzaki H, Asano H, Masutani S, et al. Anomalous origin of the Left coronary artery from the main pulmonary artery associated with Berry syndrome[J]. J Thorac Cardiovasc Surg, 2003, 126(5): 1645-1647. DOI:10.1016/s0022-5223(03)00957-7. |
| 20 |
胡仁杰, 张文, 刘鑫荣, 等. 19例Berry综合征的外科治疗[J]. 中华胸心血管外科杂志, 2018, 34(12): 713-716. DOI:10.3760/cma.j.issn.1001-4497.2018.12.002. Hu RJ, Zhang W, Liu XR, et al. Surgery treatment of Berry syndrome:a report of 19 cases[J]. Chinese Journal of Thoracic and Cardiovascular Surgery, 2018, 34(12): 713-716. DOI:10.3760/cma.j.issn.1001-4497.2018.12.002. |
 2020, Vol. 19
2020, Vol. 19


