新生儿脐膨出是先天性腹壁发育不全的疾病,腹腔内容物膨出,发病率约1/4 000,有超过50%的患儿合并其他系统畸形,并有可能合并染色体综合征,其中巨型脐膨出腹壁缺损广泛,处理更加困难,生后如不及时治疗,可能导致患儿死亡[1]。2014年以来,广西壮族自治区儿童医院采用生物补片同种异体脱细胞真皮(human acellular dermal mantrix, HADM)修补术治疗31例巨型脐膨出患儿,现将治疗效果报告如下。
材料与方法 一、临床资料收集2014年3月至2019年11月广西壮族自治区儿童医院31例巨型脐膨出患儿的临床资料,其中男童18例,女童13例,体重1.8~3.5 kg,腹壁缺损直径均>5 cm,就诊时间1 h至1 d,手术均在就诊后3~12 h内完成,31例均羊膜囊内有小肠、结肠、肝脏。合并先天性心脏病12例(法洛四联症,室间隔缺损,房间隔缺损,动脉导管未闭),合并21-三体畸形1例,合并多指1例,合并肠闭锁1例,合并梅克尔憩室2例,合并肠旋转发育不良3例,见表 1。
|
|
表 1 31例巨型脐膨出患儿的临床资料 Table 1 Clinical profiles for 31 giant omphalocele children |
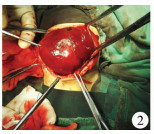
31例均采用生物补片行一期修补术。气管插管全身麻醉下,沿腹壁缺损边缘做环形切口,分离羊膜囊与肝脏粘连,避免损伤肝脏。将皮肤向外侧提起,充分游离皮肤与腹直肌前鞘,直到外侧斜肌腱膜暴露于双侧,然后将膨出物还纳入腹腔,中间缺损部分用生物补片HADM(北京清源伟业生物组织工程科技有限公司)覆盖在脏器表面,与刚游离的四周肌肉间断缝合,修补腹壁缺损[2]。如果患儿机械通气压力<25 cmH2O,则关闭腹腔是安全的,或者膀胱和胃内压力<20 cmH2O也是安全的[3]。皮下与肌层之间放置引流管,皮肤间断缝合,腹壁整形(图 1至图 4)。合并心脏畸形者先观察暂不予处理;合并多指者待患儿3个月再手术切除,合并肠闭锁者直接行肠切除、肠吻合术,合并梅克尔憩室但肠道通畅者未作处理;合并肠旋转不良行Ladd矫治术。术后呼吸机辅助通气2~5 d,7 d后慢慢开奶。

|
Download:
|
| 图 1 巨型脐膨出患儿外观图 Fig. 1 External appearance of giant omphalocele | |
|
Download:
|
| 图 2 分离巨型脐膨出患儿羊膜囊后 Fig. 2 Separating amniotic sac | |

|
Download:
|
| 图 3 HADM补片与肌层缝合修补缺损 Fig. 3 HADM mesh was sutured with muscle for repairing defect | |

|
Download:
|
| 图 4 巨型脐膨出患儿脐部整形术 Fig. 4 Umbilicus plastic surgery | |
31例患儿均治愈出院,出院后随访1年,患儿家属对腹壁外观较满意(图 5)。1例术后发生补片排斥反应,反复发热、渗液,伤口裂开,对症治疗后慢慢好转。2例脐部伤口愈合欠佳,形成巨大瘢痕填充。1例出现腹壁疝,腹腔容积扩张不满意,脐部肿物突出明显,择期再次行手术治疗。2例术后发生肠梗阻,保守治疗后好转。

|
Download:
|
| 图 5 巨型脐膨出患儿术后1年外观 Fig. 5 Appearance of giant omphalocele at 1 year post-operation | |
脐膨出是指患儿先天性腹壁发育缺损,腹腔脏器通过缺损疝出腹壁的先天性畸形,是胚胎发育过程中腹壁的四个褶皱发育不良所致[4]。16世纪,Ambrose Pare描述了脐膨出,1802年Hey首次报道了1例脐膨出修补术。巨型脐膨出主要有3种治疗方式:非手术延迟闭合、分期手术、一期手术。各手术方式都存在优缺点,故一直存在争议。因此,选择正确有效的治疗方法能挽救巨型脐膨出患儿的生命,改善预后。
非手术延迟闭合最常见的是直接在脐膨出膜上局部用药,以促进痂皮形成,然后形成肉芽和新上皮,紧接着是间隔修补余下的腹壁疝[5]。局部涂抹药物包括磺胺嘧啶银、聚维酮碘、70%酒精溶液、硝酸银等。用银离子材料外涂的优点包括易于应用(可以在家里进行),广泛的抗菌覆盖,经济负担轻,可为快速形成肉芽组织提供一个潮湿和有效的环境[6]。聚维碘酮外涂,具有效果好,副作用小,并发症低,在院外使用方便等优点;缺点是该药可导致甲状腺刺激激素升高[7]。2019年,有文献报道22例巨型脐膨出用聚维碘酮加抗生素治疗,后期间隔行闭合手术,得到了比较满意的疗效[8]。甚至有学者建议将非手术延迟闭合作为新生儿巨型脐膨出的主要治疗方法[9]。以上治疗都取得了一定的疗效,但如果在治疗过程中发生羊膜囊破溃,会产生很多并发症并危及患儿生命。此外,后期腹壁外观难看,需要行二次手术修复,在修复过程中,羊膜囊与肠管、肝脏粘连分离困难,增加了手术难度。所有非手术延迟闭合虽然可以在新生儿期避免手术打击,但会增加后期治疗的难度,且整个过程会拖延较长时间,对患儿和家属都是考验。
分期手术是采用不同的方法使腹腔容积扩大,包括放置硅橡胶体、腹腔内组织扩张器、合成夹层网片、皮瓣转移等,让膨出物暂时能容纳,是一种暂时的闭合,必须在二期手术中闭合腹壁筋膜。2018年孙健等[10]报道了硅胶袋整复16例巨型脐膨出患儿, 1~2个月后再行二期手术,患儿住院时间偏长,易发生感染。和腹裂一样,巨型脐膨出也能用硅橡胶筒仓,将筒仓固定在皮肤上,将筒仓提高,在重力作用下帮助膨出物复位,逐步地拧紧筒仓,直至可以关闭腹腔[2]。唐小捷等[11]报道采用皮肤牵引器治疗巨型脐膨出1例,因膨出物太大,采用分期手术,用皮肤牵引器逐步牵引腹腔,将腹腔容积扩大,经3次手术将脏器还纳入腹腔,此方法过程太长,需多次手术才能完成。总之,分期手术是暂时让腹腔容积增大,后续待腹腔可以容纳膨出物后再行二期关闭手术,具有耗时较长、花费高等缺点。
随着时代的发展及材料学和技术的进步,有些学者开始应用一些材料来修补缺损,一期完成手术。2005年,姜子非等[12]报道了用涤纶补片修补巨型脐膨出缺损9例,但涤纶补片是异物,组织相容性差,容易产生粘连,远期疗效堪忧。随着组织工程学的发展,HADM被应用于临床,本组报道31例,均采用HADM作为材料来修补缺损,该材料是同种异体组织,经脱细胞技术去除引起免疫排斥反应的成分,完整保留细胞外支架结构,在宿主体内修复后,可以让宿主肌纤维细胞、淋巴细胞、巨噬细胞等在支架上生长并重建血管和组织,形成新的自身组织,完成对缺损的修复。HADM已经在口腔黏膜修复、瘢痕创伤修复、膀胱外翻腹壁缺损修复等方面得到了广泛应用,并取得了良好效果[13-15]。本组应用HADM修补巨型脐膨出患儿31例,其中1例出现了排斥反应,经保守治疗好转,2例出现肠梗阻,对症处理后缓解。经过HADM修补巨型脐膨出腹壁缺损,扩充了腹腔容积,降低了腹腔压力,患儿术后常规上呼吸机2~5 d,7 d后开奶,进食快,恢复好。术后随访1年,未见明显不良反应。因为腹腔扩容满意,腹壁外观未见明显凸起,腹壁疝少见,组织相容性好,肠粘连少。远期来看,采用HADM修补巨型脐膨出外观及功能均较其他修补材料优越,具有很好的应用前景。
综上所述,HADM材料修补巨型脐膨出可一期完成,其治疗时间短,感染机会少,腹腔扩容满意,组织相容性好,排斥反应少,腹壁张力可,外观美观,是治疗巨型脐膨出的一种比较理想的方法。
| 1 |
Hijkoop A, Peters NCJ, Lechner RL, et al. Omphalocele:from diagnosis to growth and development at 2 years of age[J]. Arch Dis Child Fetal Neonatal Ed, 2019, 104(1). DOI:10.1136/archdischild-2017-314700. |
| 2 |
Gonzalez KW, Chandler NM. Ruptured omphalocele:Diagnosis and management[J]. Semin Pediatr Surg, 2019, 28(2): 101-105. DOI:10.1053/j.sempedsurg.2019.04.009. |
| 3 |
吴晔明. 小儿外科学[M]. 6版.北京: 北京大学医学出版社, 2009: 1157-1188. Wu YM. Pediatric Surgery[M]. Sixth Edition.Beijing: Peking University Medical Press, 2009: 1157-1188. |
| 4 |
Cheung M, Kakembo N, Muzira A, et al. Not gastroschisis or omphalocele or anything in between:a novel congenital abdominal wall defect[J]. Pediatr Surg Int, 2017, 33(7): 813-816. DOI:10.1007/s00383-017-4076-5. |
| 5 |
Hatch EJ, Baxter R. Surgical options in the management of large omphaloceles[J]. AM J Surg, 1987, 153(5): 449-452. DOI:10.1016/0002-9610(87)90791-4. |
| 6 |
Oquendo M, Agrawal V, Reyna R, et al. Silver impregnated hydrofiber dressing followed by delayed surgical closure for management of infants born with giant omphaloceles[J]. J Pediatr Surg, 2015, 50(10): 1668-1672. DOI:10.1016/j.jpedsurg.2015.06.011. |
| 7 |
Binet A, Scalabre A, Amar S, et al. Operative versus conservative treatment for giant omphalocele:Study of French and Ivorian management[J]. Ann Chir Plast Esthet, 2019(pii): S0294-1260. DOI:10.1016/j.anplas.2019.03.004. |
| 8 |
Dörterler ME. Management of giant omphalocele leading to early fascial closure[J]. Cureus, 2019, 11(10): e5932. DOI:10.7759/cureus.5932. |
| 9 |
Bauman B, Stephens D, Gershone H, et al. Management of giant omphaloceles:A systematic review of methods of stagedsurgical vs.nonoperative delayed closure[J]. J Pediatr Surg, 2016, 51(10): 1725-1730. DOI:10.1016/j.jpedsurg.2016.07.006. |
| 10 |
孙健, 祁泳波, 张磊, 等. 硅胶袋整复与局部压迫治疗巨型脐膨出的疗效分析[J]. 临床小儿外科杂志, 2018, 17(10): 774-777. DOI:10.3969/j.issn.1671-6353.2018.10.011. Sun J, Qi YB, Zhang L, et al. Clinical experience for giant neonatal omphalocele adopting with silica bag plus local pressing[J]. J Clin Ped Sur, 2018, 17(10): 774-777. DOI:10.3969/j.issn.1671-6353.2018.10.011. |
| 11 |
唐小捷, 吉毅, 向波. 皮肤牵引器分期治疗幼儿巨型脐膨出1例[J]. 临床小儿外科杂志, 2019, 18(9): 800-802. DOI:10.3969/j.issn.1671-6353.2019.09.019. Tang XJ, Ji Y, Xiang B. One case report of giant omphalocele treated with skin distraction device[J]. J Clin Ped Sur, 2019, 18(9): 800-802. DOI:10.3969/j.issn.1671-6353.2019.09.019. |
| 12 |
姜子非, 徐旭华, 贺华. 巨型脐膨出的治疗探讨[J]. 中华小儿外科杂志, 2005, 26(5): 279-280. DOI:10.3760/cma.j.issn.0253-3006.2005.05.019. Jiang ZF, Xu XH, He H. Treatments of giant omphalocele[J]. Chin J Pediatr Surg, 2005, 26(5): 279-280. DOI:10.3760/cma.j.issn.0253-3006.2005.05.019. |
| 13 |
Garcia OJ, Scott JR. Analysis of acellular dermal matrix integration and revascularization following tissue expander breast reconstruction in a clinically relevant large-animal model[J]. Plast Reconstr Surg, 2013, 131(5): 741e-751e. DOI:10.1097/PRS.0b013e3182865c6d. |
| 14 |
刘琳. 口腔修复膜在口腔黏膜缺损中的应用[J]. 河北医药, 2015, 37(17): 2592-2594. DOI:10.3969/j.issn.1002-7386.2015.17.009. Liu L. Application of oral prosthesis for oral mucosal defect[J]. Heibei Medical Journal, 2015, 37(17): 2592-2594. DOI:10.3969/j.issn.1002-7386.2015.17.009. |
| 15 |
Bonitz RP, Hanna MK. Use of human acellular dermal matrix during classic bladder exstrophy repair[J]. J Pediatr Urol, 2016, 12(2): 111-114. DOI:10.1016/j.jpurol.2015.10.005. |
 2020, Vol. 19
2020, Vol. 19


