先天性Ⅳ型食管闭锁的定义为近端食管为盲端,食管远近端均与气管相通。在先天性食管闭锁的分型中最少见。因其发病率低,文献以个案报道多见,临床诊疗经验不足,易导致漏诊、误诊。为探讨其临床特点及诊治方法,现将首都医科大学附属北京儿童医院新生儿外科2017年6月至2018年6月收治的6例先天性Ⅳ型食管闭锁患儿的临床资料总结如下。
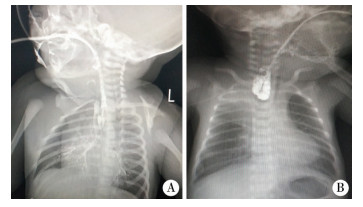
材料与方法 一、临床资料本组6例患儿中,男童4例,女童2例;年龄在2 d至4岁7个月;其中新生儿1例,1~10个月4例,>1岁1例。1例因吐沫伴吞咽及呼吸困难入院,完善食管造影、CT、电子纤维支气管镜检查后考虑为Ⅳ型食管闭锁(图 1)。其余5例均为Ⅲ型食管闭锁术后,出现饮水、奶后呛咳,反复肺炎,体重增长缓慢,进一步行食管造影及电子纤维支气管镜检查明确诊断为Ⅳ型先天性食管闭锁;3例经造影明确诊断;6例经电子纤维支气管镜明确诊断。6例先天性Ⅳ型食管闭锁患儿的临床资料见表 1。
|
Download:
|
| 图 1 先天性Ⅳ型食管闭锁与先天性Ⅲ型食管闭锁的造影对比图 A:先天性Ⅳ型食管闭锁,可见近端食管盲端细小,经胃管注入少量造影剂,气管与肺部可见显影;B:先天性Ⅲ型食管闭锁,近端食管盲端膨大,未见造影剂进入气管 Fig. 1 A:Congenital type Ⅳ esophageal atresia:proximal end of esophagus appeared slender after injecting a small amount of contrast agent via a nasogastric tube.Both trachea and lungs were visualized; B:Congenital type Ⅲ esophageal atresia:proximal end of esophagus became swollen and there was no entry of no contrast agent into trachea. | |
|
|
表 1 6例先天性Ⅳ型食管闭锁患儿临床资料 Table 1 Clinical profiles of six patients |
6例患儿中1例术前明确诊断,术中游离近端食管时,可见近端食管盲端较细,气体充盈,继续向上游离,胸腔内未见食管与气管相通,吻合食管时可见近端气体涌出。术中明确诊断为Ⅳ型先天性食管闭锁。决定先行胸腔镜下远端食管气管瘘结扎术+食管端端吻合术,待远端吻合口愈合后再经颈部修补近端食管气管瘘。其余5例患儿中,4例经颈部行食管气管瘘修补术,游离出瘘管,靠近食管侧结扎,靠近气管侧离断瘘管,修补气管及食管,用周围组织间隔气管与食管;1例经胸腔镜下食管气管瘘修补,游离暴露,分别修补气管食管。术后转至ICU病房,呼吸机支持治疗,5~7 d后拔除气管插管。
结 果本组6例患儿,1例术前明确诊断后行胸腔镜下远端食管气管瘘结扎术+食管端端吻合术,因近端瘘口位于颈部,远端位于胸腔,未一期处理2个瘘口,术后转入NICU予以呼吸机支持治疗,家长因经济原因放弃治疗。其余5例患儿,术后于PICU呼吸支持治疗5~7 d,术后食管造影均无吻合口漏,恢复良好。
5例均获得随访,随访时间6~18个月。3例食管无狭窄,喂养正常,1例食管狭窄,扩张4次治愈。
讨 论先天性食管闭锁(congenital esophageal atresia, CEA)合并食管气管瘘(tracheo-esophageal fistula, TEF)是新生儿期的先天性消化道畸形,发病率为1/2 500~1/4 500[1-4];先天性Ⅳ型食管闭锁是指食管闭锁合并远、近端食管气管瘘,在所有食管闭锁类型中占比不足1%,多见于个案报道。曾有文献报道1例食管闭锁患儿合并远端一个瘘口,近端2个瘘口[5];亦有报道食管的膜式闭锁,在闭锁水平有一个单纯的食管气管瘘[6]。
一、临床表现先天性Ⅳ型食管闭锁临床表现缺乏特异性。常常表现为出生进食后出现呛咳、呛奶、口鼻反溢,同时伴有发绀及呼吸困难;术前诊断较为困难,多数被误诊为Ⅲ型食管闭锁[7-9]。本组5例患儿新生儿期被漏诊近端食管气管瘘。按Ⅲ型食管闭锁治疗,术后出现呛咳,反复肺炎再次入院。
二、诊断与鉴别诊断对于食管气管瘘的诊断,食管造影和电子纤维支气管镜检查是常用的检查手段[10, 11]。食管造影简单易行,对食管的形态、瘘口的位置有直观的了解。但在实际操作中,容易因造影剂误吸进入气管干扰诊断。明确诊断需要反复多次检查,患儿不仅接受大量辐射线,而且容易产生吸入性肺炎。同样新生儿呼吸道发育异常缺乏典型的临床表现和影像学检查,常常容易误诊、漏诊,此时需要借助电子纤维支气管镜检查明确诊断[12]。电子纤维支气管镜联合经胃管注入美兰是诊断食管气管瘘的一种较为可靠的检查方法,电子纤维支气管镜检查亦可发现气管畸形,如气管软化、狭窄、喉裂、喉气管食管裂等[13, 14]。本组患儿食管造影明确近端气管食管瘘3例,食管气管瘘位于T2水平,远端可见食管轻度狭窄,除复发性食管气管瘘以外,可疑的2例患儿在造影过程中不能排除造影剂是由于呛咳进入气管内;5例患儿均行电子纤维支气管检查,可见气管后壁异常开口,美兰实验阳性。1例新生儿期患儿,术前食管造影可见近端盲端偏细,气管及肺内显影,考虑近端存在食管气管瘘,行电子纤维支气管检查,可见气管后壁有2个异常开口,明确诊断先天性Ⅳ型食管闭锁。
但对于新生儿期食管闭锁患儿,术前是否常规行电子纤维支气管镜检查仍存在争议[15]。先天性Ⅳ型食管闭锁发病率低,近端食管气管瘘位置较为隐蔽,新生儿耐受差,需经验丰富的内镜医生仔细检查才能明确,阳性检出率低[7, 9];以上因素限制了新生儿期电子纤维支气管镜的应用。本组1例新生儿期患儿,因术前食管造影考虑近端食管气管瘘的可能性大,行电子纤维支气管镜检查,在气管后壁可见2个瘘口,术前即明确诊断。若术前考虑存在近端食管气管瘘,可行电子纤维支气管镜检查,协助临床医师决定手术方案。随着胸腔镜在先天性食管闭锁合并食管气管瘘中的应用,胸腔镜具有视野清晰、开阔,术中游离近端食管更为方便等优点。若近端食管盲端位置偏高,因颈胸入口空间限制,可采用食管盲端卷曲下拉的办法(即用另外一把操作钳或电钩分离食管周边组织,边卷曲边下拉游离,可解决近侧游离时空间不够的困难)充分游离近端,尽可能早期发现近端遗漏的食管气管瘘[16]。有学者认为手术过程中能够发现食管造影和电子纤维支气管镜检查遗漏的近端食管气管瘘,但因经验不足,近端游离不够,导致很多患儿漏诊和误诊。术中吻合食管时,若近端食管有大量气体漏出时,应高度怀疑近端食管气管瘘[17]。本组5例患儿第一次手术均在外院完成,1例本院手术,术中可见近端食管盲端偏细,切开盲端后可见气体涌出。
三、治疗方案先天性Ⅳ型食管闭锁术前常常遗漏近端食管气管瘘诊断,经过手术治疗的患儿,与其临床表现复发性食管气管瘘相似。手术治疗的关键是明确食管气管瘘的位置。术前可结合食管造影和电子纤维支气管镜检查,综合评估,决定手术入路问题。有学者报告在电子纤维支气管镜下经瘘口放入导丝或者球囊导尿管,术中通过麻醉师的牵拉配合,使术者发现瘘管[18]。近端遗漏的食管气管瘘治疗原则与H型食管闭锁相似。Rothenberg建议近端的食管气管瘘首选胸腔镜手术治疗,具有美观,视野清晰,喉返神经损伤少等优势,但颈部的瘘口处理缝合极为困难[19]。本组5例患儿处理了近端食管气管瘘,其中4例经颈部入路,1例经胸腔入路。我们综合术前食管造影和电子纤维支气管镜检查结果,对食管气管瘘位置T2水平,瘘口位置位于气管隆突上3.5 cm,采用经颈部入路。较高位置的瘘口,胸腔镜操作需打开胸膜顶,操作空间异常狭小。位于胸腔内的食管气管瘘,确定近端气管食管瘘位置困难时,可术中行电子纤维支气管镜检查,通过体表投影明确瘘口位置,决定手术入路。本组1例经胸腔入路的患儿,术前食管造影和电子纤维支气管镜检查均提示瘘口位于胸腔;术中发现瘘口周围无明显粘连,位置明显高于原吻合口位置。关于术前明确诊断先天性Ⅳ型食管闭锁的手术治疗经验的报道不多,以个案报道多见[7]。若远近端瘘口位置较近,可经胸腔一期行手术治疗,术中游离近端食管时要注意食管与气管之间的间隙,近端盲端位置越低,与气管粘连越紧密,游离近端食管盲端时特别小心,避免损伤气管,警惕近端食管气管瘘[16]。若近端瘘口位于颈部,则先行远端食管气管瘘的处理和食管端端吻合术;术后确定无吻合口漏的情况,再行近端食管气管瘘的处理[7]。先天性Ⅲ型食管闭锁术后无明显原因的呼吸机脱离困难者,需考虑近端食管气管瘘的可能性,进一步行电子纤维支气管镜检查来明确诊断。若证实则行手术治疗。
总之,先天性Ⅳ型食管闭锁临床较为罕见,近端食管气管瘘容易漏诊。术前影像学检查缺乏特异性,食管造影、电子纤维支气管镜检查有助于明确诊断。手术方案要根据食管气管瘘的位置选择胸腔镜一期治疗或分期治疗。明确诊断后经手术治疗,预后良好。
| 1 |
Pedersen RN, Calzolari E, Husby S, et al. Oesophageal atresia:prevalence, prenatal diagnosis and associated anomalies in 23 European regions[J]. Arch Dis Child, 2012, 97(3): 227-232. DOI:10.1136/archdischild-2011-300597. |
| 2 |
Oddsberg J, Lu Y, Lagergren J. Aspects of esophageal atresia in a population-based setting:incidence, mortality and cancer risk[J]. Pediatr Surg Int, 2012, 28(3): 249-257. DOI:10.1007/s00383-011-3014-1. |
| 3 |
Sfeir R, Bonnard A, Khen-Dunlop N, et al. Esophagealatresia:Data from a National cohort[J]. J Pediatr Surg, 2013, 48(8): 1664-1669. DOI:10.1016/j.jpedsurg.2013.03.075. |
| 4 |
Leoncini E, Bower C, Nassar N. Oesophageal atresia and tracheo-oesophageal fistula in Western Australia:Prevalence and trends[J]. J Paediatr Child Health, 2015, 51(10): 1023-1029. DOI:10.1111/jpc.12909. |
| 5 |
Kane TD, Atri P, Potoka DA. Triple fistula:management of a double tracheoesoophageal fistula with a third H-type proximal fistula[J]. J Pediatr Surg, 2007, 42(6): e1-e3. DOI:10.1016/j.jpedsurg.2006.11.009. |
| 6 |
Touloukian RJ. Membranous esophageal obstruction simulating atresia with a double tracheoesophageal fistula in a neonate[J]. J Thorac Cardiovasc Surg, 1973, 65(2): 191-194. DOI:10.1016/0022-2828(73)90008-4. |
| 7 |
Shoshany G, Vatzian A, Ilivitzki A, et al. Near-missed upper tracheoesophageal fistula in esophageal atresia[J]. Eur J Pediatr, 2009, 168(10): 1281-1284. DOI:10.1007/s00431-009-0926-z. |
| 8 |
Lloreda-García JM, Sevilla-Denia S, Leante-Castellanos JL, et al. Type Ⅳ esophageal atresia with nasogastric tube in stomach[J]. J Neonatal Surg, 2017, 6(2): 582. DOI:10.21699/JNS.V6I2.582. |
| 9 |
Koivusalo AI, Pakarinen MP, Lindahl HG. Revisional surgery for recurrent tracheoesophageal fistula and anastomotic complications after repair of esophageal atresia in 258 infants[J]. J Pediatr Surg, 2015, 50(2): 250-254. DOI:10.1016/j.jpedsurg.2014.11.004. |
| 10 |
李樱子, 黄金狮, 杜京斌, 等. 先天性食管闭锁手术后并发症及处理[J]. 临床小儿外科杂志, 2018, 17(7): 45-48. DOI:10.3969/j.issn.1671-6353.2018.07.010. Li YZ, Huang JS, Du JB, et al. Analysis and management of short-term postoperative complications after esophageal atresia repair[J]. J Clinl Ped Sur, 2018, 17(7): 45-48. DOI:10.3969/j.issn.1671-6353.2018.07.010. |
| 11 |
Ng J, Antao B, Bartram J, et al. Diagnostic difficulties in the management of H-type tracheoesophagealfistula[J]. Acta Radiol, 2006, 47(8): 801-805. DOI:10.1080/02841850600854902. |
| 12 |
温洋, 彭芸, 翟仁友, 等. 小儿先天性H型气管食管瘘的诊断[J]. 医学影像学杂志, 2012, 22(10): 1665-1669. DOI:10.3969/j.issn.1006-9011.2012.10.022. Wen Y, Peng Y, Zhai RY, et al. Diagnosis of congenital H-type tracheoesophageal fistula in Infants[J]. J Med Imaging, 2012, 22(10): 1665-1669. DOI:10.3969/j.issn.1006-9011.2012.10.022. |
| 13 |
Lepeytre C, Roquelaure B, de Lagausie P, et al. Recurrent tracheoesophageal fistula in type Ⅲ esophageal atresia:Diagnosis and treatment are not easy[J]. Arch Pediatr, 2014, 21(7): 716-721. DOI:10.1016/j.arcped.2014.04.010. |
| 14 |
Katsura S, Shono T, Yamanouchi T, et al. Esophageal atresia with double tracheoesophageal fistula:a case report and review of the literature[J]. Eur J Ped Surg, 2005, 15(5): 354-357. DOI:10.1005/s-2005-865754. |
| 15 |
Erica RG, Ari R, Gander JW, et al. The role of fiberoptic endoscopy in the evaluation and management of long gap isolated esophageal atresia[J]. Pediatr Surg Int, 2010, 26(12): 1223-1227. DOI:10.1007/s00383-010-2731-1. |
| 16 |
黄金狮, 陈快, 陶俊峰, 等. 胸腔镜手术治疗先天性食管闭锁并食管气管瘘69例报告[J]. 中华小儿外科杂志, 2014, 35(6): 414-418. DOI:10.3760/cma.j.issn.0253-3006.2014.06.004. J S, Chen K, Tao JF, et al. Thoracoscopic repair of congenital esophageal atresia in neonates:a report of 69 cases[J]. Chin J Pediatric Surg, 2014, 35(6): 414-418. DOI:10.3760/cma.j.issn.0253-3006.2014.06.004. |
| 17 |
Spitz L. Oesophageal atresia[J]. Orphanet J Rare Dis, 2007, 2(1): 24. DOI:10.1186/1750-1172-2-24. |
| 18 |
Mattei P. Double H-type tracheoesophageal fistulas identified and repaired in 1 operation[J]. J Pediatr Surg, 2012, 47(11): 11-13. DOI:10.1016/j.jpedsurg.2012.06.012. |
| 19 |
Rothenberg SS. Thoracoscopic management of non-type C esophageal atresia and tracheoesophagealatresia[J]. J Pediatr Surg, 2018, 53(1): 121-125. DOI:10.1016/j.jpedsurg.2017.10.025. |
 2019, Vol. 18
2019, Vol. 18


