早发性脊柱侧凸(early onset scoliosis,EOS)是指发病年龄 < 10岁的脊柱侧凸,该病可导致患儿身材矮小、躯干畸形及胸廓发育受限, 也可间接造成患儿心肺功能受损,严重者可引起胸廓功能不全综合征(thoracic insufficiency syndrome,TIS),甚至造成呼吸衰竭[1-4]。目前,传统生长棒系统(椎体-椎体撑开)和基于肋骨的撑开系统[如纵向可撑开型人工钛肋技术(vertical expandable prosthetic titanium rib,VEPTR)]均被广泛用于EOS所致脊柱侧凸治疗,可在增加脊柱高度的同时帮助患儿肺功能得到改善[5-12]。VEPTR技术通过固定肋骨后实行纵向撑开增加患儿胸腔容积,为肺脏生长提供空间。同时,撑开系统的作用力也可传导至脊柱,使脊柱侧凸状况得到改善[13]。近年来,VEPTR技术也开始逐步应用治疗其他无合并肋骨畸形的早发性脊柱侧凸[8, 10]。但VEPTR器械昂贵,较易出现并发症[14],因此其临床应用也存在一定的局限性。本研究将从疗效、安全性等方面探讨椎体-肋骨撑开技术的临床应用价值。
材料与方法 一、临床资料以2005—2010年于首都医科大学附属北京儿童医院行椎体-肋骨撑开术或传统生长棒椎体-椎体撑开术治疗的28例EOS患儿为研究对象。纳入标准:①进展性EOS(年平均Cobb角增长>10°)且年龄>5岁;②接受椎体-肋骨撑开术或椎体-椎体撑开术;③脊柱侧凸的主弯部位位于胸椎;④随访时间≥3年。排除标准:①既往有脊柱相关手术病史;②远端固定点位于骶骨或骨盆;③撑开期间更换过其它内固定系统。患儿初次手术前、初次手术后及末次随访时均拍摄站立位脊柱正侧位X线片,测量冠状位主弯Cobb角、矢状位胸椎后凸角及胸廓高度;初次手术前均行脊柱CT及MRI检查以明确脊柱侧凸类型,了解脊柱及脊髓的发育情况;初次手术前和末次随访时均测量胸廓(T1至T12)高度,并进行肺功能检查。采用肺功能检测仪记录患儿用力肺活量(forced vital capacity,FVC),一秒用力呼气容积(forced expiratory volume in 1 second,FEV1)及两项指标实际值占预测值的百分比,同时记录患儿术中、术后并发症情况。与植入物相关的并发症包括肋骨骨折、生长棒断裂、椎弓根钉拔出及肋骨钩脱出;一般并发症包括胸膜破损、切口感染。
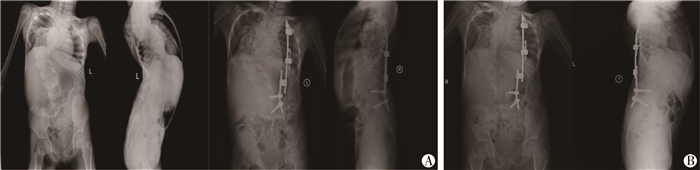
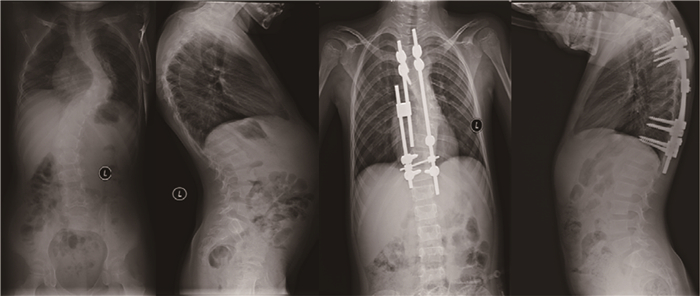
二、手术方法根据患儿脊柱侧凸情况行双侧或单侧撑开术。两组均采用气管插管全身麻醉,术中患儿取俯卧位,按照体表定位切口位置,剥离腰背筋膜,分离椎旁肌。椎体-肋骨撑开组中,于切口上端剥离显露预定撑开的肋骨(通常为靠近上端椎旁的肋骨),剥离骨膜后用特制的肋骨抱钩固定肋骨(图 1)。椎体-椎体撑开组剥离显露上端椎的椎弓根位置,置入椎弓根螺钉(图 2)。下方剥离显露下端椎弓根位置,通常在下端椎两个椎体的双侧椎弓根置入4枚椎弓根螺钉,以增加结构的稳定性,应注意尽量避免剥离椎板外骨膜,防止不必要的自发融合。C形臂确认位置良好后,截取适当长度棒,预弯生理性胸椎后突和腰椎前突,将生长棒分别置入椎弓根钉和特制的椎板钩,两棒间连接处置一多米诺联系装置,便于后续行生长棒撑开手术,凹侧适当撑开后锁紧内固定装置。根据患儿脊柱侧凸和生长情况,每年行1~2次生长棒撑开手术,术中显露生长棒阀,用撑开器械撑开生长阀,撑开长度为0.5~1.0 cm,如发现内植入物并发症则同时行内固定调整更换。
|
Download:
|
| 图 1 椎体-肋骨-生长棒系统治疗EOS患儿脊柱正侧位X线片 注 A.患儿女,6岁,初次术前和初次术后脊柱正侧位X线片;B.末次随访时脊柱正侧位X线片,可见胸廓高度增加,凹侧胸腔容积增大,主弯Cobb角得到改善 Fig. 1 Typical case of spine-rib distraction system A.Frontal and lateral spinal films of a 6-year-old girl using spine-rib-growth rod system at before and after initial surgery; B.On frontal and lateral spinal films the last follow-up, height of thoracic spine increased, volume of caved cage expanded and main curvature's Cobb's angle improved. | |
|
Download:
|
| 图 2 椎体-椎体-生长棒系统治疗EOS患儿脊柱正侧位X线片 注 患儿男,5岁,初次术前和初次术后脊柱正侧位X线片。 Fig. 2 Typical case of spine-spine distraction system 5-year-old boy was treated with a spine-spine distraction before and after the index surgery. | |
采用SPSS 22.0统计学软件进行统计学分析。对患儿临床资料采用均数、标准差、率、构成比进行描述;椎体-肋骨撑开组和椎体-椎体撑开组患儿脊柱侧凸影像学角度、平均胸廓(T1~T12)高度、肺功能指标的比较采用两独立样本t检验;两组患儿初次手术前与末次随访时肺功能的组内比较采用配对t检验;两组患儿并发症发生率的比较采用χ2检验或Fisher确切概率法;以P<0.05为差异有统计学意义。
结 果 一、临床资料椎体-肋骨撑开组中,男童2例,女童12例,初次手术年龄5~7岁;椎体-椎体撑开组中,男童4例,女童10例,初次手术年龄5~7岁。脊柱侧凸类型包括先天性脊柱侧凸20例(椎体-肋骨撑开组10例,椎体-椎体撑开组10例),神经肌肉性脊柱侧凸1例(椎体-椎体撑开组1例),综合征型脊柱侧凸5例(椎体-肋骨撑开组2例,椎体-椎体撑开组3例),特发性脊柱侧凸2例(椎体-肋骨撑开组1例,椎体-椎体撑开组1例。患儿平均年龄(5.8±0.5)岁,平均随访时间(4.1±0.5)年。两组患儿EOS类型分布、初次手术年龄及随访时间差异均无统计学意义(P>0.05), 详见表 1。
|
|
表 1 椎体-肋骨撑开组和椎体-椎体撑开组患儿人口学资料(n=28) Table 1 Demographic profiles of spine-rib distraction and spine-spine distraction groups(n=28) |
初次手术后,椎体-肋骨撑开组主弯Cobb角大于椎体-椎体撑开组(P < 0.05),椎体-肋骨撑开组初次手术矫正率高于椎体-椎体撑开组(P < 0.05);末次随访时,椎体-肋骨撑开组主弯Cobb角大于椎体-椎体撑开组(P < 0.05),椎体-肋骨撑开组末次随访时主弯Cobb角矫正率低于椎体-椎体撑开组(P < 0.05)。而两组初次手术前胸椎主弯Cobb角、初次手术后胸椎后凸角及末次随访胸椎后凸角均无统计学差异(P>0.05),见表 2。
|
|
表 2 椎体-肋骨撑开组和椎体-椎体撑开组患儿脊柱侧凸影像学资料的比较(x±s) Table 2 Comparisons of imaging angles for spine-rib distra-ction and spine-spine distraction groups(x±s) |
初次手术前,两组平均胸廓高度无统计学差异(P>0.05);末次随访时,两组平均胸廓高度有统计学差异(P < 0.05)。两组末次随访时胸廓(T1至T12)高度与初次手术前相比均增加(P < 0.05),见表 3。
|
|
表 3 两组初次手术前、末次随访时平均胸廓(T1~T12)高度比较(x±s) Table 3 Comparisons of mean height of thoracic spine (T1-T12) at before initial surgery and the final follow-up for spine-rib distraction and spine-spine distraction groups (x±s) |
两组初次手术前与末次随访时肺功能比较结果显示,两组末次随访时FVC、FEV1值显著高于初次手术前水平(P < 0.05),而FVC%、FVEV1%值没有显著变化(P>0.05),见表 4。
|
|
表 4 两组初次手术前与末次随访时肺功能比较(x±s) Table 4 Comparison of intrapulmonary function between the vertebral body-rib cage group and the vertebral body-vertebral body distraction group before and after the initial operation(x±s) |
两组并发症比较,椎体-肋骨撑开组肋骨骨折、肋骨钩脱出的发生率显著高于椎体-椎体撑开组(P < 0.05),而两组椎弓根螺钉拔出、生长棒断裂、胸膜破损的发生率差异没有统计学意义(P>0.05),见表 5。
|
|
表 5 两组并发症的发生率比较(例) Table 5 Comparisons of operative complications for spine-rib distraction and spine-spine distraction groups(n) |
生长棒技术现已广泛应用于早发性脊柱侧凸的手术治疗中,其疗效已得到证实,可在控制畸形进展的同时延续脊柱生长,使胸廓不对称的情况得到改善[15, 16]。VEPTR技术最初由Robert Campbell[17]报道,在当时被用于先天性脊柱侧凸、肋骨畸形合并胸廓机能不全综合征患儿的治疗,达到纠正胸壁畸形和脊柱侧弯的目的。随后有学者通过研究证实VEPTR技术可有效增加患儿肺功能和肺容积,在控制脊柱畸形进展的同时保持脊柱的生长功能, 也可改善胸廓发育不全综合征患儿的呼吸功能[18, 19]。但VEPTR器械昂贵,仪器规格型号与我国儿童体型的匹配性差,出现并发症的概率也较高。本院自2003年开始采用椎体-肋骨撑开系统治疗早发性脊柱侧凸,近端肋骨锚定点均使用特殊结构的肋骨抱钩器械,与VEPTR器械相比体积更小巧,安装更简便。
本研究中,椎体-肋骨撑开组和椎体-椎体撑开组患儿接受初次手术后,主弯Cobb角均得到明显改善,说明两种手术方式对EOS患儿的脊柱畸形均有良好的矫正效果,与其他文献报道结果大致相同[20]。Bess等[21]曾报道,以脊柱为锚定点的撑开系统对早发性脊柱侧凸患儿的矫正率高于以肋骨为锚定点的撑开系统。本组病例中,脊柱-肋骨撑开术对EOS患儿主弯Cobb角矫正率与传统生长棒椎体-椎体撑开术相比略低,也在一定程度上证实了这一观点。两组初次手术矫正率及末次随访矫正率没有差异,提示两种手术方式对EOS后凸畸形的矫形效果相同。末次随访时,椎体-肋骨撑开组和椎体-椎体撑开组的主弯Cobb角及胸椎后凸角均较初次手术后增加,说明两组撑开技术均对脊柱侧凸畸形有良好的矫形维持效果,可有效控制脊柱侧凸的进展。但椎体-肋骨撑开组在末次随访时的主弯Cobb角仍大于椎体-椎体撑开组,可能是因为随着撑开次数的增多,椎体-肋骨撑开组的撑开作用逐渐减弱,对胸椎后凸和主弯Cobb角的矫正效果逐渐减低。
初次手术时,椎体-肋骨撑开组和椎体-椎体撑开组的平均胸廓高度均小于正常儿童平均高度,由于胸廓高度与肺活量大致呈正相关,因此胸廓高度可用于预测患儿的肺功能情况[22]。末次随访时,椎体-肋骨撑开组和椎体-椎体撑开组的胸廓高度均较术前明显增长,说明椎体-肋骨撑开术可有效维持胸廓的正常生长,并间接促进肺脏的发育,对呼吸系统的生长过程起促进作用。
末次随访时,两组患儿的用力肺活量(FVC)和一秒钟用力呼气容积(FEV1)与初次手术前相比均有所提高,说明两种手术方式均可促进早发性脊柱侧凸患儿的肺脏发育。而两组患儿的FVC%和FEV1%末次随访时与初次术前相比无明显变化,且初次手术前和末次随访时均低于正常儿童肺功能水平,说明随着患儿年龄增长及胸廓发育,两组患儿肺功能只是得到了相对的改善,仍不能达到正常同龄儿童水平。但是两组患儿的FVC%和FEV1%无明显降低,也说明了两种手术方式均可在一定程度上阻止肺功能进一步恶化。根据两组患儿初次手术前、末次随访时胸廓高度的对比结果可知,两组手术方式均可促进胸椎的生长和胸廓的发育,但肺功能的改善相对有限,可能与凸侧肺脏代偿等原因有关。
两组患儿均未出现伤口感染,但椎体-肋骨撑开组的并发症出现概率仍明显高于椎体-椎体撑开组,而并发症一旦出现,往往需要通过手术调整内固定器械,这无疑增加了患儿的痛苦和家庭的经济负担。肋骨钩脱出主要与肋骨钩松动有关,也与肋骨在撑开力的长时间作用于下产生疲劳性骨折有关。因此,从力学角度考虑,可以尝试增加近端肋骨锚定点,分散撑开力,也可考虑双侧(凸侧及凹侧)同时置入肋骨钩并行双侧撑开,达到有效分散撑开力、减少并发症的目的。
| 1 |
El-Hawary R, Akbarnia BA. Early Onset Scoliosis-Time for Consensus[J]. Spine Deformity, 2015, 3(2): 105-106. DOI:10.1016/j.jspd.2015.01.003. |
| 2 |
Skaggs DL, Guillaume T, El-Hawary R. Early Onset Scoliosis Consensus Statement, SRS Growing Spine Committee, 2015[J]. Spine Deformity, 2015, 3(2): 107. DOI:10.1016/j.ispd.2015.001.002. |
| 3 |
Canavese F, Dimeglio A. Normal and abnormal spine and thoracic cage development[J]. World J Orthop, 2013, 4(4): 167-174. DOI:10.5312/wjo.v4.i4.167. |
| 4 |
Pehrsson K, Larsson S, Oden A, et al. Long-term follow-up of patients with untreated scoliosis.A study of mortality, causes of death, and symptoms[J]. Spine, 1992, 17(9): 1091-1096. DOI:10.1097/00007632-199209000-00014. |
| 5 |
Akbarnia BA, Breakwell LM, Marks DS, et al. Dual growing rod technique followed for three to eleven years until final fusion:the effect of frequency of lengthening[J]. Spine, 2008, 33(9): 984-990. DOI:10.1097/BRS.0b013e31816c8b4e. |
| 6 |
Akbarnia BA, Marks DS, Boachie-Adjei O, et al. Dual growing rod technique for the treatment of progressive early-onset scoliosis:a multicenter study[J]. Spine, 2005, 30(17 Suppl): 46. |
| 7 |
Campbell MR Jr, Hellvocke AK. Growth of the thoracic spine in congenital scoliosis after expansion thoracoplasty[J]. Spine Journal, 2003, 2(5): 71-72. |
| 8 |
El-Hawary R, Samdani A, Wade J, et al. Rib-based Distraction Surgery Maintains Total Spine Growth[J]. J Pediatr Orthop, 2016, 36(8): 841-846. DOI:10.1097/BPO.0000000000000567. |
| 9 |
Emans JB, Caubet JF, Ordonez CL, et al. The treatment of spine and chest wall deformities with fused ribs by expansion thoracostomy and insertion of vertical expandable prosthetic titanium rib:growth of thoracic spine and improvement of lung volumes[J]. Spine, 2005, 30(17 Suppl): 58. DOI:10.1097/01.brs.0000175194.31986.2f. |
| 10 |
Flynn JM, Emans JB, Smith JT, et al. VEPTR to treat nonsyndromic congenital scoliosis:a multicenter, mid-term follow-up study[J]. J Pediatr Orthop, 2013, 33(7): 679-684. DOI:10.1097/BPO.0b013e31829d55a2. |
| 11 |
Hasler CC, Mehrkens A, Hefti F. Efficacy and safety of VEPTR instrumentation for progressive spine deformities in young children without rib fusions[J]. Eur Spine J, 2010, 19(3): 400-408. DOI:10.1007/s00586-009-1253-9. |
| 12 |
Skaggs DL, Sankar WN, Albrektson J, et al. Weight gain following vertical expandable prosthetic titanium ribs surgery in children with thoracic insufficiency syndrome[J]. Spine, 2009, 34(23): 2530-2533. DOI:10.1097/BRS.0b013e3181bd09f5. |
| 13 |
Dede O, Motoyama EK, Yang CI, et al. Pulmonary and Radiographic Outcomes of VEPTR (Vertical Expandable Prosthetic Titanium Rib) Treatment in Early-Onset Scoliosis[J]. J Bone Joint Surg Am, 2014, 96(15): 1295-1302. DOI:10.2106/JBJS.M.01218. |
| 14 |
Waldhausen JH, Redding G, White K, et al. Complications in using the vertical expandable prosthetic titanium rib (VEPTR) in children[J]. J Pediatr Surg, 2016, 51(11): 1747-1750. DOI:10.1016/j.jpedsurg.2016.06.014. |
| 15 |
Farooq N, Garrido E, Altaf F, et al. Minimizing complications with single submuscular growing rods:a review of technique and results on 88 patients with minimum two-year follow-up[J]. Spine, 2010, 35(25): 2252-2258. DOI:10.1097/BRS.0b013e3181ecf41a. |
| 16 |
Watanabek K, Uno K, Suzuki T, et al. Risk factors for complications associated with growing-rod surgery for early-onset scoliosis[J]. Spine, 2013, 38(8): 464-468. DOI:10.1097/BRS.0b013e318288671a. |
| 17 |
Campbell RM Jr, Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis[J]. J Bone Joint Surg Am, 2004, 86(8): 1659-1674. |
| 18 |
Motoyama EK, Yang CL. Thoracic malformation with early-onset scoliosis:effect of serial VEPTR expansion thoracoplasty on lung growth and function in children[J]. Paediatr Respir Rev, 2009, 10(1): 12-17. DOI:10.1016/j.prrv.2008.10.004. |
| 19 |
Campbell RM, Smith MD, Hell-Vocke AK. Expansion Thoracoplasty:The Surgical Technique of Opening-Wedge Thoracostomy[J]. The Journal of Bone and Joint Surgery, 2004, 86(Suppl 1): 51-64. |
| 20 |
Gomez JA, Lee JK, Kim PD, et al. "Growth friendly" spine surgery:management options for the young child with scoliosis[J]. J Am Acad Orthop Surg, 2011, 19(12): 722-727. DOI:10.5435/00124635-201112000-00002. |
| 21 |
Bess S, Akbarnia BA, Thompson GH, et al. Complications of growing-rod treatment for early-onset scoliosis:analysis of one hundred and forty patients[J]. Journal of Bone & Joint Surgery American Volume, 2010, 92(15): 2533. DOI:10.2106/JBJS.I.01471. |
| 22 |
Karol LA, Johnston C, Mladenov K, et al. Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis[J]. J Bone Joint Surg Am, 2008, 90(6): 1272-1281. DOI:10.2106/JBJS.G.00184. |
 2019, Vol. 18
2019, Vol. 18


