先天性支气管胆管瘘(congenital broncho biliary-fistula,CBBF)是由于支气管与胆管之间异常连接形成的瘘管畸形,可伴发胆道闭锁、食道闭锁、膈疝等其他先天性畸形[1]。该病为临床罕见疾病,容易因漏诊而延误治疗,造成患儿不良预后,为分析其原因,减少漏诊,现将首都医科大学附属北京儿童医院2017年11月收治的1例CBBF患儿进行报告。
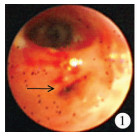
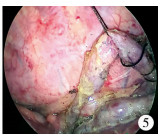
病例摘要患儿女,3岁5个月,足月剖宫产,出生体重3 200 g。患儿生后5 d出现咳嗽,有痰不易咳出,痰液为黄色胆汁样,后出现呼吸困难、拒食、嗜睡,当地县人民医院查胸部CT提示:双肺散在斑片影,右肺中下叶不张,以“重症肺炎”转入上级市妇幼保健医院ICU,给予吸氧、吸痰、抗感染治疗。考虑同时合并胃食管反流,遂改变体位,2周后肺部炎症得到控制,4周后呼吸道症状好转出院,出院后患儿偶尔出现溢奶,奶中仍伴有黄色物质,味苦,量少,每日2~4次,与进食无关,哭闹时显著。夜间有阵发呛咳,发热,呼吸困难,偶见口角、鼻腔金黄色物质,大便色黄,10天后就诊于北京市中医院,查胸片后仍考虑为重症肺炎,诊断为“过敏导致的特殊类型肺炎,先天性食管狭窄”,继续抗感染治疗,追查上消化道造影未见异常提示,症状逐渐缓解出院。患儿呼吸道症状虽好转,但溢奶伴黄色物质情况较前无明显变化。3年来反复间断咳嗽,咳出黄绿色物经抗炎治疗后症状改善不够彻底,于我院就诊,入院查体:生命体征平稳,精神反应可,呼吸平稳,未见鼻扇,三凹征阴性。右侧胸廓塌陷,左侧肋间间隙正常,右侧肋间隙狭窄。双肺呼吸音粗,可闻及湿啰音及哮鸣音。心律齐,心音有力,各瓣膜听诊区未及病理性杂音。腹软,全腹无压痛、反跳痛,未触及明显异常。脊柱稍向左凸,四肢可见杵状指。电子支气管镜提示:右主气管开口内侧壁接近隆突水平可见一异常开口,不断有金黄色粘液溢出。右上、右中、右下各支开口位置正常(图 1);食管造影示食管通畅,未见造影剂外溢;胸部CT示右中间段支气管内侧壁异常开口,向下可见一含气管腔,沿脊柱右前方下行,达食管远端前方,呈不规则含气囊腔,肝内可见少量气体密度影,提示支气管胆管瘘(图 2、图 3),双肺支气管壁增厚,扩张明显,右肺高密度影,其内可见支气管充气征,提示肺炎;胸部MR示薄层原始图肝左右叶交界处可见细条高信号,斜行向上走行,上端观察不清;SPECT结果提示右中间段支气管内侧异常开口,并与左胆管相通,存在支气管胆管瘘。入院诊断为:“先天性支气管胆管瘘,慢性肺炎,肺不张,支气管扩张”。入院抗感染控制3周后行胸腔镜下支气管胆管瘘切除术,术中探查右中下肺与胸膜纤维膜状黏连,松解黏连游离右肺,打开胸膜,切断结扎奇静脉,奇静脉稍下方后纵膈可见一大小约1.5 cm×0.8 cm淋巴结,轻柔游离该淋巴结;位于淋巴结右侧后方可见一异常条索管道(瘘管),长约5 cm,直径约0.7 cm,头侧3/5为硬质软骨结构,余2/5为软质胆管样结构,透壁可见黄绿色胆汁,瘘管左后方脊柱前可见食管,沿瘘管上下游离,上方到T4气管隆突水平,瘘管头端与右主支气管相连,向下游离至膈肌食管裂孔处。术中瘘管造影(图 4)显示通向肝左管、胆总管,至十二指肠显影。远端紧贴食管裂孔结扎两道,近端瘘管质硬, 边剪断边以5 - 0普理灵线缝合封闭残端,完整切除瘘管,胸腔注水膨肺,检查气管残端无漏气,无活动性出血后取出瘘管,置入1根胸腔闭式引流管,拔出Trocar,缝合皮肤切口,术中图片见图 5。术后病理提示:送检管样组织大部内衬鳞状上皮,局灶柱状上皮,上皮下可见混合性腺体、软骨、纤维组织及灶状异位胰腺腺泡,全段管壁可见淋巴细胞为主的慢性炎细胞浸润,符合先天性支气管胆管瘘特征。术后患儿恢复顺利,无咳嗽,无咳胆汁样痰,无恶心及呕吐,无气短、胸闷,精神饮食良好,大便色黄,术后2周痊愈出院。
|
Download:
|
| 图 1 支气管镜检查结果(箭头所示为支气管瘘管异常开口,周围可见黄色胆汁样液溢出,其上方为右中下段支气管主干) Fig. 1 Bronchoscope(The arrow showed the abnormal opening of the bronchial fistula with yellow biliary fluid, and the upper part was the main branch of the right bronchus.) | |

|
Download:
|
| 图 2 胸部CT检查结果(箭头所示支气管瘘管,通向膈肌、肝脏方向) Fig. 2 Chest CT(The arrow showed a bronchial fistula leading to the diaphragm and liver.) | |

|
Download:
|
| 图 3 CT重建结果(可见右肺支气管异常瘘管存在) Fig. 3 CT reconstruction(CT showed the existence of abnormal fistula in the right bronchus.) | |

|
Download:
|
| 图 4 术中X线片结果(胸腔异常瘘管,远端膈肌,近端气管隆突水平) Fig. 4 Intraoperative(The operation revealed abnormal thoracic fistula, distal diaphragm, and proximal tracheal carina.) | |
|
Download:
|
| 图 5 术中造影结果(胸腔瘘管通向肝左管、胆总管,至到十二指肠) Fig. 5 Intraoperative radiography(The operation revealed revealed a thoracic fistula leading to the left hepatic duct, common bile duct and duodenum.) | |
CBBF是临床上较为罕见的疾病,1952年由Neuhauser等首次报道[2],婴儿及成人均可发病[3],女性多见,以呼吸道症状和反复肺部感染为主要表现。本例患儿为3岁5个月女性,出生5 d后发病,出现反复咳嗽、咳黄痰、呼吸困难、胆汁样痰或呕吐,甚至出现肺炎、肺不张,曾多次因肺部感染辗转多家医院住院接受抗菌药物治疗,均未找到致病根本原因。分析该病漏诊原因我们认为:由于CBBF罕见,临床以肺炎或支气管炎表现为主,极易与先天性消化道畸形、重症肺炎、气管食管瘘、胃食管返流等疾病相混淆;除早期排出黄色胆汁样痰液外,后续症状均为肺炎相关症状,无典型特征。其次,因本例患儿每次症状发作时与肺炎表现相似,造成诊治过程中医生忽视了其他系统疾病的病史采集, 仅局限于对症支持治疗,未能进一步就肺炎反复发作且咳黄色痰液进行深究(如查找痰液中的胆红素检查等)[4],治标不治本,诊疗上形成惯性和局限性思维,也是导致该病漏诊的客观因素。
CBBF发病机制尚不明确,目前主要有两种理论:一是上消化道重复畸形,气管与肝内胆管憩室发生异常连接;二是肺芽和肝芽之间发生异常连接[5]。本例患儿瘘管病理近端有呼吸道结构,远端组织类似消化道,支持第二种发病机制假说。由于瘘管的存在,使胆汁通过瘘管引流至气管,持续的胆汁刺激使支气管、肺组织发生慢性炎症,进而导致肺实变和肺不张,因此表现为反复发作、持续难治性肺炎,久而久之引起慢性缺氧, 影响儿童及婴儿生长发育、智力发育[6]。本例患儿也出现杵状指、体重、发育较同龄儿童偏低等继发临床表现,同样证明了这一点。本例患儿虽最终在支气管镜检查中发现黄色粘液溢出的异常开口位置,但前期就诊多家医院均未进行该项检查,胸部CT、MRI检查结果也未能提供有力的诊断依据,明确病因的过程受到一定制约,也是漏诊原因之一。本例患儿先后多次CT、MRI检查结果均提示肺部病变严重程度发生了变化,但均未观察到异常瘘管结构,可能是因为本病虽为先天性疾病,但新生儿时期瘘管尚未发育成熟,受周围条件影响,难以直接发现瘘管,因此极易漏诊[7]。PTC和ERCP虽为有创检查,但较CT及MRCP具有不可替代的优势,注射造影剂后可直接观察到瘘管的存在[8],但上述检查均未在本例患儿中得到应用。此外,核素检查还可为诊断及术中处理瘘管提供依据,但并非临床常规检查,常在考虑该疾病后行此项检查。此例患儿在初步诊断为该疾病后进行核素检查,使得微创手术顺利完成,因此完善的影像学检查是该病诊断及治疗的保障。最后,提高对本病的认识,使患儿能够及早得到有效治疗是减少漏诊的关键。
| 1 |
Sachdev A, Chugh K, Krishana A, et al. Congenital tracheobiliary fistula:acase report with review of literature[J]. Pe-diatr Surg Int, 2011, 27(8): 899-905. DOI:10.1007/s00383-011-2879-3. |
| 2 |
Neuhauser EB, Elkin M, Landing B. Congenital direct commu-nication between biliary system and respiratory tract[J]. AMA Am J Dis Child, 1952, 83(5): 654-659. DOI:10.1111/j.1651-2227.1952.tb17855.x. |
| 3 |
Uramoto H, Kawano O, Sugimoto M, et al. Congenital bron-chobiliary fistula in a 65-year-old woman[J]. Intern Med, 2008, 47(14): 1367-1370. DOI:10.2169/internalmedicine.47.0943. |
| 4 |
Liao GQ, Wang H, Zhu GY, et al. Management of acquired bronchobiliary fistula:A systematic literature review of 68 cases pubished in 30 years[J]. World J Gastroenterol, 2011, 17(33): 3842-3849. DOI:10.3748/wjg.v17.i33.3842. |
| 5 |
Croes F, Van Nieuwaal NH, Van Heijst AF, et al.Congenital tracheobiliary fistula J Pediatr Surg, 2010, 45(4): E9-E11.
|
| 6 |
Ferkol T, McDowell KM, Gauderer MW, et al. Sinopulmonary manifestations of congenital bronchobiliary fistula[J]. Clin Pediatr(Phila), 1994, 33(3): 181-184. DOI:10.1177/000992289403300314. |
| 7 |
Yoon DH, Shim JH, Lee WJ, et al. Percutaneous management of a bronchobiliary fistula after radiofrequency ablation in a patient with hepatocellular carcinoma[J]. Korean J Radiol, 2009, 10(4): 411-415. DOI:10.3348/kjr.2009.10.4.411. |
| 8 |
Artunduaga M, Patel NR, Wendt JA, et al. Bronchobiliary fistula localized by cholescintigraphy with single-photon emission computedtomography[J]. World J Nucl Med, 2015, 14(1): 60-62. DOI:10.4103/1450-1147.150556. |
 2019, Vol. 18
2019, Vol. 18


