2. 青岛大学附属医院外科(山东省青岛市, 266000);
3. 青岛市黄岛区妇幼保健计划生育服务二中心(山东省青岛市, 266000);
4. 青岛大学附属医院小儿外科(山东省青岛市, 266000)
2. Department of General Surgery, Affiliated Hospital, Qingdao University, Qingdao, 266000, China;
3. Maternal & Child Health Care of Family Planning Service Center, Qingdao 266000, China;
4. Department of Pediatric Surgery, Affiliated Hospital, Qingdao University, Qingdao 266000, China
脐膨出是一种新生儿腹壁缺损的先天畸形,病情复杂,常并发多种畸形,病死率高,已严重威胁新生儿的健康[1]。据统计, 脐膨出发生率为1.16/10 000, 病死率高达52%,而巨大危重型脐膨出的病死率更是高达67%[2, 3]。近年来国外报道新生儿脐膨出的发病率并没有降低,反而呈现上升趋势[4]。随着医学及相关学科的发展,对于脐膨出的认识及治疗都得到了不断的提高,其治疗方法繁多,不仅要求高治愈率, 还应争取一期或在短期内完成治疗[5]。对于巨型脐膨出的治疗多采用Ⅱ期和分期整复修补术,也有人采用广泛游离腹膜及腹壁皮肤的方法行Ⅰ期修补术,但手术并发症多,且腹腔间隔综合征的发生率高,存活率低[6, 7]。本研究自2010年10月至2017年4月收集青岛市妇女儿童医院收治的16例巨型脐膨出患儿的病例资料,采用保留羊膜囊硅胶袋整复与局部压迫治疗,取得较好的治疗效果,现报道如下。
材料与方法 一、临床资料收集青岛市妇女儿童医院2010年10月至2017年4月收治的16例巨型脐膨出患儿的临床资料,其中男童10例,女童6例,年龄为生后5 min至48 h,体重1 800~4 500 g。所有患儿腹壁缺损直径在6 cm以上, 最大直径10 cm。膨出物为肠管和肝、脾等内脏器官,表面囊膜透明,无破裂。1例合并左侧膈疝,其余15例均未发现有其它脏器发育异常情况。
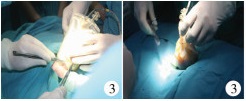
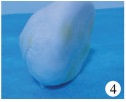
二、手术方法患儿取仰卧位,严格按照无菌原则,局部消毒,将部分膨出物还纳入腹腔,紧缩羊膜囊,结扎切除远端多余羊膜囊组织,将体外膨出脏器纳入无菌硅胶袋,并与腹壁缺损皮缘处间断缝合,术后逐渐挤压收紧硅胶袋还纳肠管等脏器(图 1至图 3)。每日从硅胶袋顶端注入碘伏。一般术后1~2个月去除硅胶袋后,根据腹壁缺损大小及膨出物情况改用自制半球形纱布袋加压包扎(图 4、图 5),创面用湿润烧伤膏外敷,观察治疗效果。

|
Download:
|
| 图 1 新生儿巨型脐膨出外观 Fig. 1 Neonatal giant omphalocele | |

|
Download:
|
| 图 2 紧缩羊膜囊,结扎切除远端多余羊膜囊组织 Fig. 2 Tightening amniotic sac and excising distal extra-amniotic sac | |
|
Download:
|
| 图 3 硅胶袋整复,边缘缝合 Fig. 3 Reconstruction with silica bag and suturing with edge of abdominal wall | |
|
Download:
|
| 图 4 自制半球形纱布袋 Fig. 4 Semi-spherical gauze bag | |

|
Download:
|
| 图 5 加压包扎,局部压迫 Fig. 5 Local pressing | |
16例巨型脐膨出患儿中,12例膨出物逐渐完全还纳,腹壁逐渐生长直至缺损处完全愈合形成接近自然脐部形态(图 6)。1例合并膈疝的巨型脐膨出,在入院后按上述方法行“巨型脐膨出硅胶袋整复术”。术后2个月患儿膨出脏器完全还纳,在气管插管全身麻醉下行“巨型脐膨出Ⅱ期修补术+膈疝修补术”。3例巨型脐膨出患儿未完全回纳,但创面完全上皮化,2~3年后行脐部修补整形术。所有病例随访5个月至6年, 脐部外观满意,发育良好,无并发症和死亡病例。

|
Download:
|
| 图 6 愈合形成接近自然脐部形态 Fig. 6 Healing naturally | |
脐膨出是新生儿常见的腹壁发育畸形,是指先天性腹壁发育不全,腹壁中心缺损,腹腔内脏通过脐部缺损疝出腹壁为特征的先天畸形。研究表明,脐膨出是由于胚胎在发育过程中腹壁的4个褶中某个褶发育停顿或发育不良而形成[1]。随着产前诊断、麻醉、手术技术的提高以及术后呼吸管理和静脉高营养的应用, 该病的治疗效果明显改善,但如处理不及时或处理不当,其病死率仍高达25.8% ~43%[8]。因此,正确认识该病,积极予以有效的治疗,有助于进一步提高新生儿脐膨出的治愈率,并改善预后。
按照腹壁缺损大小,脐膨出可分为小型脐膨出及巨型脐膨出,对于治疗方案的选择,主要根据腹壁缺损大小、囊膜破裂及感染与否、有无合并严重畸形等情况,选择最佳治疗方法。小型脐膨出,囊腔不大,膨出物仅为肠管,无肝脏及其它器官,可将囊膜去除,在没有过度腹内压下,将腹壁Ⅰ期缝合即可治愈。而巨型脐膨出,通常腹壁缺损直径>6 cm,膨出物为胃、肝、脾、胰等脏器,手术修补时需广泛游离腹膜及腹壁皮肤,但如果勉强将囊膜内容物推回狭小的腹腔内,会提高腹内压力而产生不良的后果,如横膈位置提高导致呼吸障碍;下腔静脉受压而减少静脉血回流;肾脏的血流减少而引发肾衰竭等致死性腹高压[9]。近年来多主张行分期或Ⅱ期修补术,如使用手术手套、输血袋、纱巾、涤纶袋等替代材料扩大腹腔行分期手术治疗, 也有用硅胶袋修复巨型脐膨出的报道[10, 11]。对于无手术条件的患儿, 腹壁缺损较大,出生时间>72 h,身体一般情况不佳或膨出囊膜有感染倾向的患儿,国内外有学者采用各种保守治疗方法,如van Eijck等[12]对11例巨大脐膨出采用组织分离技术;Kilbride等[13]采用封闭式负压引流技术,均缓慢还纳脐膨出物,促进小腹腔容量扩张;也有学者采用2%红汞、70%酒精和0.25%硝酸银混合液或硝酸银溶液及70%乙醇溶液等消毒结痂剂预防感染,促进上皮生长,瘢痕组织覆盖囊膜,最后择期再行手术修补治疗[14];Ein等[15]对20例巨大脐膨出采用早期局部覆盖磺胺嘧啶银而形成瘢痕组织,延缓脐膨出的关闭;2006年,Tran等[16]使用皮维酮碘外涂囊膜成功救治了巨大脐膨出患儿;同样,Adetayo等[17]使用腹内组织膨胀剂治疗巨大脐膨出患儿也取得了成功。
本研究中,脐膨出患儿出生后将体外膨出脏器纳入无菌硅胶袋,并与腹壁缺损皮缘处间断缝合,逐渐挤压收紧硅胶袋,约1~2个月后脏器可逐渐还纳,摘除硅胶袋后继续利用自制半球形纱布袋加压包扎,仍然每日消毒,外涂湿润烧伤膏。对于缺损相对较小,新生儿早期腹壁肌肉有向腹中线靠拢的生长机制,随着生长发育,脐环逐渐缩小,类似于脐疝缺口通过两侧直肌筋膜的延伸而关闭的机理,约6~12个月后腹壁逐渐生长直至缺损处完全愈合形成接近自然脐部形态。对于缺损大的患儿,出生后利用此方法,虽然腹壁肌肉不能完全愈合,但6~12个月创面完全上皮化。因此,与目前治疗巨型脐膨出的诸多方法相比,该方法主要优势如下:一是采用此种方法,虽然患儿成长至1岁后仍面临着二次手术,但对于手术的耐受力明显提高,同时该方法对新生儿呼吸、循环系统影响较小,一般不需要机械通气,避免了因缝合修补腹壁引起腹内压过大对呼吸、循环造成影响,防止发生腹腔间隔综合征及手术相关并发症,减少脐膨出病死率[18]。二是该方法保留了羊膜囊,避免膨出物暴露,减少感染及器官粘连几率。三是使用该方法的患儿可早期进食,减少肠外营养时间。但在治疗过程中,应注意脐部局部护理,逐渐还纳过程中注意观察患儿呼吸循环等生命体征。因此,在新生儿脐膨出临床治疗过程中,保留羊膜囊的同时应用硅胶袋整复及局部压迫治疗相结合的方法,能够提高新生儿巨型脐膨出的治愈率,降低该病的病死率。
| 1 |
Baird R, Gholoum S, Laberge JM, et al. Management of a giant omphalocele with an external skin closure system[J]. J Pediatr Surg, 2010, 45(7): e17-e20. DOI:10.1016/j.jpedsurg.2010.05.004. |
| 2 |
施诚仁, 刘国华, 金惠明, 等. 新生儿外科学[M]. 上海: 上海科学普及出版社, 2002: 496-502. Shi CR, Liu GH, Jin HM, et al. Neonatal Surgery[M]. Shanghai: Shanghai Popular Sciences Publishing House, 2002: 496-502. |
| 3 |
Danzer E, Victoria T, Bebbington MW, et al. Fetal MRI-calculated total lung volumes in the prediction of short-term outcome in giant omphalocele:preliminary findings[J]. Fetal Diagn Ther, 2012, 31(4): 248-253. DOI:10.1159/000334284. |
| 4 |
Collins SR, Griffin MR, Arbogast PG, et al. The rising prevalence of gastroschisis and omphalocele in Tennessee[J]. J Pediat Surg, 2007, 42(7): 1221-1224. DOI:10.1016/j.jpedsurg.2007.02.012. |
| 5 |
Ledbetter DJ. Congenital abdominal wall defects and reconstruction in pediatric surgery:gastroschisis and omphalocele[J]. Surg Clin North Am, 2012, 92(3): 713-727. DOI:10.1016/j.suc.2012.03.010. |
| 6 |
刘敏, 彭明惺, 罗启成. 先天性脐膨出的诊断和治疗[J]. 中国临床医生, 2003, 31(3): 13-15. DOI:10.3969/j.issn.1008-1089.2003.03.007. Liu M, Peng MX, Luo QC. Diagnosis and treatment of congenital omphalocele[J]. Chinese Journal for Clinicians, 2003, 31(3): 13-15. DOI:10.3969/j.issn.1008-1089.2003.03.007. |
| 7 |
Mitanchez D, Walter-Nicolet E, Humblot A. Neonatal care in patients with Giant ompholocele:arduous management but favorable outcomes[J]. J Pediatr Surg, 2010, 45(8): 1727-1733. DOI:10.1016/j.jpedserg.2010.04.011. |
| 8 |
Mortellaro VE, StPeter SD, Fike FB, et al. Review of the evidence on the closure of abdominal wall defects[J]. Pediatr Surg Int, 2011, 27(4): 391-397. DOI:10.1007/s00383-010-2803-2. |
| 9 |
朱小春, 葛午平, 林炎坤. 新生儿脐膨出手术预后因素分析[J]. 临床小儿外科杂志, 2004, 3(2): 121-127. DOI:10.3969/j.issn.1671-6353.2004.02.012. Zhu XC, Ge WP, Lin YK, et al. Evaluation of prognostic factors of neonatal omphalocele operation[J]. J Clin Ped Sur, 2004, 3(2): 121-127. DOI:10.3969/j.issn.1671-6353.2004.02.012. |
| 10 |
Esquirol Caussa J, Herrero Vila E. Epidermal growth factor, innovation and safety[J]. Med Clin (Barc), 2015, 145(7): 305-312. DOI:10.1016/j.medcli.2014.09.012. |
| 11 |
刘翔, 郑训淮, 戚士芹, 等. 用硅胶袋修复巨型脐膨出与腹裂13例报告[J]. 临床小儿外科杂志, 2007, 6(3): 19-20. DOI:10.3969/j.issn.1671-6353.2007.03.008. Liu X, Zheng XH, Qi SQ, et al. Application of silica gel bag staged repair abdominal wall deficiency[J]. J Clin Ped Sur, 2007, 6(3): 19-20. DOI:10.3969/j.issn.1671-6353.2007.03.008. |
| 12 |
van Eijck FC, van Vlimmeren LA, Wijnen RM, et al. Functional, motor developmental, and long-term Outcome after the component separation technique in children with giant omphalocele:a case control study[J]. J Pediatr Surg, 2013, 48(3): 525-532. DOI:10.1016/j.jpedsurg.2012.08.010. |
| 13 |
Kilbride KE, Cooney DR, Custer MD. Vacuum-assisted closure:a new method for treating patients with giant omphalocele[J]. J Pediatr Surg, 2006, 41(1): 212-215. DOI:10.1016/j.jpedsurg.2005.10.003. |
| 14 |
姜子非, 徐旭华, 贺华. 巨型脐膨出的治疗探讨[J]. 中华小儿外科杂志, 2005, 26(5): 279-280. DOI:10.3760/cma.j.issn.0253-3006.2005.05.019. Jiang ZF, Xu XH, He H. The treatment of giant omphalocele[J]. Chin J Pediatr Surg, 2005, 26(5): 279-280. DOI:10.3760/cma.j.issn.0253-3006.2005.05.019. |
| 15 |
Ein SH, Langer JC. Delayed management of giant omphalocele using silver sulfadiazine cream:an 18 year experience[J]. J Pediatr Surg, 2012, 47(3): 494-500. DOI:10.1016/j.jpedsurg.2011.08.014. |
| 16 |
Tran DA, Truong QD, Nguyen MT. Topical application of povidone-iodine solution (Betadine) in the management of giant omphaloceles[J]. Dermatology, 2006, 212(1): 88-90. DOI:10.1159/000089205. |
| 17 |
Adetayo OA, Aka AA, Ray AO. The use of intra-abdominal tissue expansion for the management of giant omphaloceles:review of literature and a case report[J]. Ann Plast Surg, 2012, 69(1): 104-108. DOI:10.1097/SAP.0b013e31822128f5. |
| 18 |
庄岩, 王克莱. 脐膨出的外科治疗[J]. 罕少疾病杂志, 2003, 10(1): 26-27. DOI:10.3969/j.issn.1009-3257.2003.01.012. Zhuang Y, Wang KL. Surgical treatment of omphalocele[J]. Journal of Rare & Uncommon Disease, 2003, 10(1): 26-27. DOI:10.3969/j.issn.1009-3257.2003.01.012. |
 2018, Vol. 17
2018, Vol. 17

