2. 川北医学院附属医院内分泌科(四川省南充市, 637000)
2. Department of Endocrinology, Affiliated Hospital, North Sichuan Medical College, Nanchong 637000, China
尿道口周围的管状腺体发生阻塞可导致腺体分泌物无法排出,进而形成尿道旁腺囊肿,其总体发病率较低,多见于20~40岁女性;新生女婴尿道旁腺囊肿较罕见,目前多以国外文献病例报道为主[1-3]。我们对四川大学华西医院小儿泌尿外科收治的2例新生女婴尿道旁腺囊肿患儿进行随访,并结合相关文献复习,探讨该类疾病可能的病因以及相关的诊治方案。
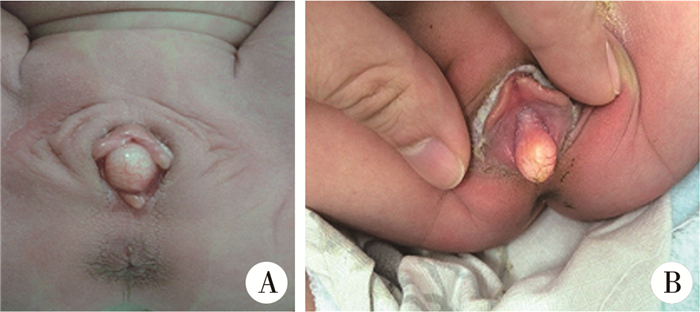
材料与方法 一 临床资料 一 临床表现病例1 女,6日龄,因生后发现尿道口包块就诊。患儿无发热、畏寒、寒战、排尿困难及尿路刺激症状。局部查体:尿道口旁可见一直径约10 mm的黄白色卵圆形囊性包块,表面可见血管,质地柔软,无明显触痛,挤压时尿道口无明显分泌物溢出(图 1A)。泌尿系统B超显示双肾、输尿管及膀胱未见明显异常,尿常规未见异常。
|
图 1 新生女婴尿道旁腺囊肿外观(A为病例1;B为病例2) Fig.1 Paraurethral cysts in female neonates (A:Case 1; B:Case 2) |
病例2 女,生后6 h,因生后未排小便,通过查体发现尿道口周围包块就诊。局部查体:尿道口旁可见1.2 cm×1.0 cm大小的黄白色梭形包块1突出体表,质地柔软,无触痛及脓血性分泌物(图 1B)。门诊留观4 h后患儿自行排尿,未行进一步检查。
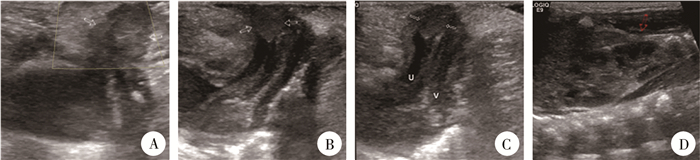
二 影像学特征对于首次接诊的病例1,除安排常规的泌尿系统超声和尿常规检查外,还进行了经体表的尿道局部超声检查(图 2)。局部B超显示:尿道稍扩张,尿道口见大小约1.0 cm×0.7 cm低回声结节,边界清楚,内部未见明显血流信号。
|
图 2 病例1泌尿系统彩超表现 A:尿道口旁皮下低回声病灶,CDFI示内部无血流信号;B:尿道口旁病灶与尿道、膀胱关系;C:局部放大显示病灶与尿道关系,可见尿道轻度扩张呈无回声,宽约1.0 cm;D:超声提示双肾及输尿管未见积水扩张。白色箭头示囊肿,红色箭头示肾脏 Fig.2 Urinary ultrasonography of case 2 A:subcutaneous hypoechoic lesions besides urethral orifice and no internal hemodynamic signal according to CDFI; B:It depicted the relationship between paraurethral lesions, urethra and bladder.C:It denoted the relationship between lesions and urethra through partial enlargement and mild urethral expansion of around 1.0 cm wide; D:ultrasound revealed no hydronephrosis or ureterohydronephrosis.Note:white arrow indicated cyst; red arrow kidney |
2例通过病史询问、查体及相关检查评估后,考虑其尿道口旁局部病变暂未导致不良影响,遂未进一步采取临床干预措施。予门诊随访其临床症状、囊肿大小等,囊肿分别在2个月(病例1)和6个月(病例2)后自然消散,后期随访期间未再复发。
二 文献检索及结果以“新生儿”“女婴”“尿道旁腺囊肿”“paraurethral cyst”“Skene's duct”“neonate, newborn”为检索词检索PubMed、中国知网、万方数据库、中国生物医学文献数据库以及维普数据库的文献资料(发表时间截至2019年2月),检索到的文献均为外文文献。一项研究总结了2000—2011年的病例资料,所以本文将在此文基础上继续补充女婴尿道旁腺囊肿的病例报道。排除临床资料不完整的报道后,最终纳入8篇文献[4-11]。本文根据治疗决策的不同进行分组总结和分析,其中观察随访的病例共14例(表 1),选择外科治疗的病例共15例(表 2)。29例中无症状患儿共23例,其中13例选择随访观察,10例选择外科手术治疗。6例存在排尿异常、肿块增大等临床表现,其中1例选择临床观察,另外5例选择手术治疗。
| 表 1 新生女婴尿道旁腺囊肿病例报告文献分析:观察随访组 Table 1 Summary of reported cases of paraurethral cyst in the past 18 years:observation follow-up group |
|
|
| 表 2 新生女婴尿道旁腺囊肿病例报告文献分析:外科治疗组 Table 2 Summary of reported cases of paraurethral cyst in the past 18 years:surgical group |
|
|
女性尿道周围有尿道海绵体环绕,约有6~30个腺体开口于尿道,其中最大的两个腺体称为尿道旁腺,又称为Skene腺[12, 13]。尿道旁腺囊肿(Skene腺囊肿)与处女膜囊肿合称为唇间囊肿,是形成唇间肿块的原因之一[14]。成年女性常因局部炎症导致导管阻塞,进而形成尿道旁腺囊肿,而新生女婴尿道旁腺导管阻塞的病因尚不明确。有学者认为,新生女婴的发病可能是因为发育过程中尿路上皮细胞易位造成导管口阻塞了Skene腺管,进而导致囊肿形成[14, 15]。
新生女婴尿道旁腺囊肿仅表现为尿道口两侧出现黄色光滑的卵圆形囊性包块,表面有明显的血管分布,无触痛,质地柔软,常不伴明显的分泌物[16-18]。在文献资料中以及本文收集的病例中,患儿的囊肿多为单侧,但Gottesman等[19]也曾报道了双侧尿道口囊肿的病例。且大多数尿道旁腺囊肿的直径约10~20 mm,但Blaivas等[18]报道了一例3 cm×3 cm大小的病例,而Yilmaz等[9]报道的囊肿大小为19.9 mm×56.2 mm。根据囊肿的大小及其相对于尿道口位置的不同,患儿也可能会出现尿线异常、排尿困难及尿路梗阻等表现[3]。同时受到来自母体雌激素的影响,少数患儿可能会出现乳房增大、阴道肿胀、阴道流血等临床表现,但其与局部囊肿的相关性尚不明确[20]。这与Soyer等[20]研究结果相契合,该研究发现女婴尿道旁腺囊肿的出现和自愈似乎与其来自母体的雌激素变化同步,这提醒我们雌激素在该疾病的发生发展中可能存在一定的作用。目前多数学者认为,新生儿尿道旁腺囊肿是一种自限性疾病,大部分可在数天至数月自动消退[4, 21]。
诊断新生儿尿道旁腺囊肿首先应进行仔细查体,判断囊肿外观是否为黄白色卵圆形囊性包块;其次需要判断囊肿性质,质地是否柔软,有无触痛;最后判断囊肿位置,是否遮挡阴道或尿道[20-22]。对于部分病例来讲,超声或造影等影像学检查在评估囊肿性质方面也很重要,并且可以排除可能存在的肾积水、尿路梗阻等泌尿生殖系统合并症[23]。针吸囊肿也是必要时可选择的诊断性操作,如穿刺液为乳白色黏液,则可临床诊断为Skene's囊肿[10, 24]。在临床诊治过程中,新生儿尿道旁腺囊肿还需要与多种泌尿生殖系统疾病相鉴别,如处女膜闭锁、Gardner管囊肿、苗勒管囊肿、尿道脱垂、阴道积液、阴道横纹肌肉瘤、输尿管囊肿、湿疣、尿道憩室、尿道息肉、先天性脂肪瘤和阴道脱垂等[25, 26]。
文献资料显示,新生女婴尿道旁腺囊肿可选择的治疗方法包括观察随访和外科治疗,虽然目前国外学者对于新生儿尿道旁腺囊肿治疗策略的选择尚有争议,但根据患儿的实际情况选择合适的方案是肯定的;无特殊临床症状的患儿多数可采用临床观察,而合并有排尿异常、肿块增大等表现的患儿可采用外科手术治疗[4, 27]。在本文的病例中,病例1无临床不适表现,遂选择观察随访以等待囊肿自然消退;而病例2可能系暂时生理性未排尿,但仍需高度警惕尿路梗阻的可能,经观察4 h后患儿自行排尿,故未行进一步干预处理。但若由于囊肿导致局部梗阻而影响了患儿排尿,甚至可能存在引起上尿路梗阻等情况时,应及时选择临床干预措施解除尿路梗阻(如行导尿术或采取适当的外科手术进行干预)。外科手术治疗的优势主要包括:可缓解囊肿引起的尿路梗阻,缩短病程以减轻父母观察等待期间的焦虑,部分病例还可获得囊肿壁的组织病理学检查机会等。目前可选择的外科术式主要包括针吸术、去顶术、切开引流术以及囊肿切除术等。由于囊肿切除术存在损伤尿道的可能,所以该术式主要应用于成年女性;而针吸术相对操作简便、安全,且侵入性较其他干预措施小,所以得到了部分学者的推荐[20, 24, 28],甚至有学者认为其可以作为首选的治疗方案[9];但也有学者认为针吸术后,囊肿存在复发的可能,更偏向损伤小、恢复较快且安全有效的囊肿去顶或造口术作为小儿Skene's囊肿的治疗首选[10, 29]。
综上,新生女婴尿道旁腺囊肿是一种临床比较罕见的疾病,常导致部分医护人员以及患儿家长的过度忧虑和担心。目前的临床资料显示,该类疾病多不具有临床不良影响,且具有较大的自然缓解率。因此,对该类患儿(尤其是不合并有临床不适表现者),可选择随访观察,以等待囊肿自然消退;对囊肿较大或合并有排尿困难等不适者,可选择外科手术处理,但术式应尽可能微创。
| [1] |
Chong Y, Eom M, Park KH, et al. Adenofibroma of Skene's duct:a case report[J]. Patholog Res Int, 2010, 2010: 318973. DOI:10.4061/2010/318973 |
| [2] |
Fujimoto T, Suwa T, Ishii N, et al. Paraurethral cyst in female newborn:is surgery always advocated?[J]. J Pediatr Surg, 2007, 42(2): 400-403. DOI:10.1016/j.jpedsurg.2006.10.030 |
| [3] |
Shaw SC, Vinod MS, Devgan A. Parameatal urethral cyst[J]. Med J Armed Forces India, 2018, 74(1): 76-77. DOI:10.1016/j.mjafi.2017.02.007 |
| [4] |
Nakamura E, Shintaku S, Horii M, et al. Early regression of paraurethral cyst in a neonate[J]. Pediatr Neonatol, 2014, 55(3): 225-227. DOI:10.1016/j.pedneo.2012.12.005 |
| [5] |
Johnson CT, Millard SE, Wang MH, et al. Prenatal diagnosis of a paraurethral cyst[J]. J Pediatr Urol, 2013, 9(1): e91-e93. DOI:10.1016/j.jpurol.2012.10.003 |
| [6] |
Mino A, Rodriguez J. Skene duct cyst in female newborns-case reports[J]. Rev Chil Pediatr, 2014, 85(5): 584-587. DOI:10.4067/S0370-41062014000500009 |
| [7] |
Kuipers BC, Jansen EJ, van Mil EG. A neonate with an interlabial cyst[J]. Ned Tijdschr Geneeskd, 2015, 159: A8355. |
| [8] |
Costantino E, Ganesan GS. Paraurethral cysts in newborn girls[J]. BMJ Case Rep, 2016. DOI:10.1136/bcr-2016-216689 |
| [9] |
Yilmaz Y, Celik IH, Dizdar EA, et al. Paraurethral cyst in two female newborns:which therapy option?[J]. Scand J Urol Nephrol, 2012, 46(1): 78-80. DOI:10.3109/00365599.2011.599337 |
| [10] |
Moralioglu S, Bosnali O, Celayir AC, et al. Paraurethral Skene's duct cyst in a newborn[J]. Urol Ann, 2013, 5(3): 204-205. DOI:10.4103/0974-7796.115754 |
| [11] |
Tseng M, Lin S. Interlabial mass in a neonate with paraurethral cyst[J]. World Journal of Pediatrics, 2016, 12(1): 121. DOI:10.1007/s12519-015-0051-1 |
| [12] |
Huffman, John W. The detailed anatomy of the para-urethral ducts in the adult human female[J]. Am J Obstet Gynecol, 1948, 55(1): 86-101. DOI:10.1016/0002-9378(48)90157-4 |
| [13] |
Ogihara S, Kato H. Endocrine cell distribution and expression of tissue-associated antigens in human female paraurethral duct:possible clue to the origin of urethral diverticular cancer[J]. Int J Urol, 2000, 7(1): 10-15. DOI:10.1046/j.1442-2042.2000.00125.x |
| [14] |
Berkman DS, McHugh MT, Shapiro E. The other interlabial mass:hymenal cyst[J]. J Urol, 2004, 171(5): 1914-1915. DOI:10.1097/01.ju.0000120149.63384.b1 |
| [15] |
杨军, 陈敏, 鞠文, 等. 女性尿道旁腺囊肿及尿道憩室的临床特征[J]. 临床泌尿外科杂志, 2005, 20(11): 652-653. Yang J, Chen M, Ju W, et al. Clinical features of female paraurethral cysts and urethral diverticula[J]. Journal of Clinical Urology, 2005, 20(11): 652-653. DOI:10.3969/j.issn.1001-1420.2005.11.002 (in Chinese) |
| [16] |
Bergner DM. Paraurethral cysts in the newborn[J]. South Med J, 1985, 78(6): 749-750. DOI:10.1097/00007611-198506000-00035 |
| [17] |
Nussbaum AR, Lebowitz RL. Interlabial masses in little girls:review and imaging recommendations[J]. AJR Am J Roentgenol, 1983, 141(1): 65-71. DOI:10.2214/ajr.141.1.65 |
| [18] |
Blaivas JG, Pais VM, Retik AB. Paraurethral cysts in female neonate[J]. Urology, 1976, 7(5): 504-507. DOI:10.1016/0090-4295(76)90191-6 |
| [19] |
Gottesman JE, Sparkuhl A. Bilateral Skene duct cysts[J]. J Pediatr, 1979, 94(6): 945-946. DOI:10.1016/S0022-3476(79)80229-2 |
| [20] |
Soyer T, Aydemir E, Atmaca E. Paraurethral cysts in female newborns:role of maternal estrogens[J]. J Pediatr Adolesc Gynecol, 2007, 20(4): 249-251. DOI:10.1016/j.jpag.2007.04.007 |
| [21] |
Badalyan V, Burgula S, Schwartz RH. Congenital paraurethral cysts in two newborn girls:differential diagnosis, management strategies, and spontaneous resolution[J]. J Pediatr Adolesc Gynecol, 2012, 25(1): e1-e4. DOI:10.1016/j.jpag.2011.02.012 |
| [22] |
Fathi K, Pinter A. Paraurethral cysts in female neonates[J]. Acta Paediatr, 2003, 92(6): 758-759. DOI:10.1111/j.1651-2227.2003.tb00615.x |
| [23] |
Breysem L, Rayyan M, Bogaert G, et al. High-resolution perineal ultrasound of a paraurethral cyst in a neonate (2008:8b)[J]. Eur Radiol, 2008, 18(11): 2701-2703. DOI:10.1007/s00330-008-1007-9 |
| [24] |
Kusama Y, Ito K, Suzuki T. Skene's duct cyst[J]. J Gen Fam Med, 2017, 18(5): 299-300. DOI:10.1002/jgf2.64 |
| [25] |
Nickles SW, Burgis JT, Menon S, et al. Prepubertal Skene's abscess[J]. J Pediatr Adolesc Gynecol, 2009, 22(1): e21-e22. DOI:10.1016/j.jpag.2007.11.004 |
| [26] |
Sharifi-Aghdas F, Ghaderian N. Female paraurethral cysts:experience of 25 cases[J]. BJU Int, 2004, 93(3): 353-356. DOI:10.1111/j.1464-410x.2003.04615.x |
| [27] |
Fujimoto T, Suwa T, Ishii N, et al. Paraurethral cyst in female newborn:is surgery always advocated?[J]. J Pediatr Surg, 2007, 42(2): 400-403. DOI:10.1016/j.jpedsurg.2006.10.030 |
| [28] |
Lee NH, Kim SY. Skene's duct cysts in female newborns[J]. J Pediatr Surg, 1992, 27(1): 15-17. DOI:10.1016/0022-3468(92)90094-N |
| [29] |
Kimbrough HJ, Vaughan EJ. Skene's duct cyst in a newborn:case report and review of the literature[J]. J Urol, 1977, 117(3): 387-388. |
 2020, Vol. 19
2020, Vol. 19


