发育性髋关节脱位(developmental dysplasia of the hip, DDH)是儿童骨科常见的下肢骨关节畸形,治疗的关键是早期诊断并且获得满意复位。对于6~24个月的DDH患儿,麻醉下闭合复位石膏固定术是目前公认的首选方案,但是术中闭合复位质量的评价标准尚不统一,常用的方法有临床查体、安全区测定、关节造影、术中磁共振等[1-4]。
关节造影评估闭合复位已被小儿骨科医师广泛应用,但可行闭合复位的造影标准尚存在较多争议[5]。临床常用的是Bowen标准,然而满足该标准闭合复位的髋关节仍可能发生再脱位[6]。为进一步提高闭合复位成功率,本研究回顾性分析了88例DDH患儿的术中髋关节造影X线平片,发现在人类位髋关节造影X线平片上,股骨头软骨内缘与坐骨外缘重叠的程度不同,故将二者的关系分为3度,重叠为Ⅰ度,相接为Ⅱ度,分离为Ⅲ度,而7髋术后再脱位患儿均为Ⅲ度。所以,本文提出“坐骨重叠征(ischium overlap sign, IOS)”的概念,并回顾性研究IOS与DDH术后再脱位的关系,现报道如下。
材料与方法 一、临床资料回顾性分析2013年9月至2017年5月山东大学附属省立医院治疗的97例DDH患儿,其中88例资料完整。88例中男童16例,女童72例,平均年龄12(5~24)个月,平均随访时间34(15~59)个月;双侧17例,左右两侧分别计算,共计105髋,左侧63髋,右侧42髋。按照“三线一点”法进行分型[7],1髋为髋臼发育不良,11髋半脱位,93髋全脱位(Ⅰ度72髋,Ⅱ度21髋)。23髋曾行吊带/支具治疗,其余82髋为初次治疗。
患儿入院后完善相关术前准备,气管插管全麻下尝试闭合复位,保持髋关节屈曲100° ~110°、外展50° ~60°,行关节造影术。常规消毒铺巾,髋关节内侧入路进针,关节腔内注射用生理盐水1 : 1稀释的泛影葡胺1.0 mL,适度活动髋关节使其充分显影。根据Bowen关节造影标准[6]选择闭合或切开复位人类位石膏固定术,即满足以下条件:①复位后股骨近端干骺端低于H线;②软骨股骨头水平半径的2/3位于Perkin线内;③股骨头复位后位于盂唇外缘以下时采用闭合复位,否则采用切开复位。
闭合复位者直接行人类位石膏固定。切开复位者采用SP入路,切断髂腰肌腱、清理增厚的圆韧带、髋臼纤维脂肪组织,切断横韧带,复位股骨头,紧缩关节囊,逐层缝合,然后再行人类位石膏固定。
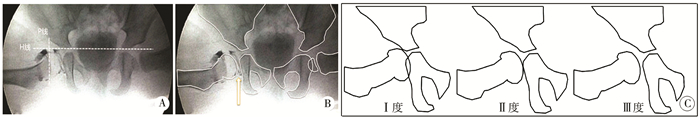
二、术后处理及分组IOS是指在人类位髋关节造影X线平片上,股骨头软骨内缘与坐骨外缘的重叠关系,二者重叠为Ⅰ度,相接为Ⅱ度,分离为Ⅲ度(图 1)。
|
Download:
|
| 图 1 坐骨重叠征及分度示意图 注 A:15月龄女童,右侧髋关节全脱位,术中试行闭合复位,人类位髋关节造影X线平片显示复位符合Bowen标准;B:分别勾勒出股骨头软骨内缘线与坐骨外缘线,二者分离(箭头所示);C:IOS分度示意图,在人类位髋关节造影X线平片上,股骨头软骨内缘与坐骨外缘重叠为Ⅰ度,相接为Ⅱ度,分离为Ⅲ度 Fig. 1 Arthrographic diagrams of IOS for DDH children | |
术后患儿定期随访,重点记录再脱位的病例。回顾性分析术中髋关节造影平片,按照IOS将105髋进行分度,并将93髋全脱位患儿分为Ⅰ度(n=14)、Ⅱ度(n=39)、Ⅲ度(n=40)3组,比较组间术后再脱位发生率(组内再脱位髋数/组内总髋数)的差异,在此基础上进一步分析再脱位与性别、侧别、复位方式、家族史、既往治疗、“三线一点”分型等影响因素的关系。
三、统计学处理应用SPSS 21.0统计软件进行数据整理与分析。对于不同性别、侧别、复位方式、家族史、既往治疗和“三线一点”分型等计数资料采用n(%)表示,两组间比较采用Pearson χ2检验或者Fisher确切概率法。对于不同复位方式再脱位率的比较采用Pearson χ2检验。以α=0.05为检验水准,P<0.05为差异有统计学意义。
结 果1例髋臼发育不良(1髋)和11例半脱位(11髋)患儿的IOS均为Ⅰ度。
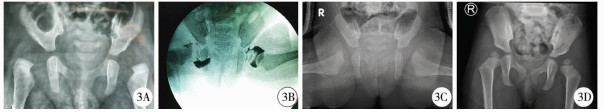
93髋全脱位中,IOS Ⅰ度14髋、Ⅱ度39髋,此两组均行闭合复位石膏固定术,无再脱位病例;IOS Ⅲ度40髋,该组中17髋行闭合复位石膏固定术,6髋再脱位;其余23髋行切开复位石膏固定术,1髋再脱位;共7髋发生再脱位。典型病例详见图 2、图 3。

|
Download:
|
| 图 2 15月龄女童DDH的系列X线片 A:15月龄女童的术前骨盆正位X线片,显示右侧髋关节全脱位;B:术中关节造影显示复位符合Bowen标准,故采用闭合复位石膏固定术,但IOS为Ⅲ度;C:术后发生再脱位;D:改行切开复位石膏固定术;E:术后2年复位良好 Fig. 2 Serial radiography films of a 15-month-old DDH girl | |
|
Download:
|
| 图 3 5月龄女童DDH的系列X线片 A:5月龄女童患有双侧DDH,根据“三线一点”法[7]分型,左侧全脱位,右侧半脱位;B:术中关节造影显示左侧IOS为Ⅲ度,右侧为Ⅰ度;C:给予左髋切开复位、右髋闭合复位联合人类位石膏固定,双髋复位良好;D:术后2年复位良好 Fig. 3 Serial radiography films of a 5-month-old girl with bilateral DDH | |
93髋全脱位术后再脱位的相关因素分析详见表 1。不同性别、侧别、复位方式、家族史、既往治疗及“三线一点”分型的髋关节再脱位发生率无统计学差异(P>0.05)。而针对IOS分度,Ⅲ度组再脱位发生率为17.5%,高于Ⅰ、Ⅱ度两组,且差异有统计学意义(P=0.006),见表 1。
|
|
表 1 93髋全脱位术后再脱位的相关因素分析[n(%)] Table 1 Analysis of correlation factors for redislocation in 93 hips with DDH[n(%)] |
IOS为Ⅲ度的40髋中,闭合复位的再脱位发生率(6/17,35.3%)高于切开复位者(1/23,4.4%),差异有统计学意义(χ2=4.518,P=0.034),见表 2。
|
|
表 2 IOS为Ⅲ度的髋关节不同复位方式再脱位发生率比较[n(%)] Table 2 Comparison of redislocation rates between different reducing modes for DDH with IOS Ⅲ[n(%)] |
2岁以下DDH的首选治疗方案是闭合复位人类位石膏固定术,对预防术后再脱位和股骨头缺血性坏死,获取满意的复位质量有重要意义[1, 2, 7, 8]。但是,评估闭合复位质量的方法和标准尚不统一,评估方法有临床查体、安全区测定、关节造影、核磁共振等[3, 4]。
Severin[9]于1941年提出采用术中关节造影评估复位质量,现已被广泛应用。目前,常采用Bowen标准和内侧造影池(medial dye pool, MDP)来评价关节造影[6]。Bowen标准已在方法中详细描述。Drummond等[10]报道正常髋关节中MDP<2 mm。Lonnerholm[11]认为MDP<4 mm属于稳定性复位。Race[12]认为MDP处于2~7 mm,无软组织嵌入,不需要极度体位维持属于可接受的复位标准。但是,术中准确测量MDP较为困难,测量结果容易受体位、透视角度、造影剂量及X线图像放大率等多种因素的影响,误差较大。因此,已有学者提出新的评价标准,比如贾国强等[13]提出术中造影“安全带征”可作为2岁以内DDH患儿的闭合复位指标。
本组105髋治疗过程中均行关节造影,并采用Bowen标准选择复位方式,93髋全脱位中有7髋发生再脱位。回顾性分析术中髋关节造影片发现,正常髋关节的股骨头软骨内缘应与坐骨外缘相重叠。本研究中髋臼发育不良和半脱位患儿的IOS均为Ⅰ度,可以间接证实该观点。对于全脱位的髋关节,IOS可以分为重叠、相接、分离3种情况,7髋术后再脱位者均为Ⅲ度,进一步分析表明IOS与DDH术后再脱位有关。
关于IOS为Ⅲ度的髋关节如何选择复位方式,本组IOS为Ⅲ度的40髋中再脱位发生率为17.5%,其中闭合复位的再脱位发生率高达35.29%,切开复位占4.35%,差异有统计学意义。该结果表明IOS为Ⅲ度时,应谨慎选择闭合复位。另外,7髋再脱位中有4髋既往曾行保守治疗,虽然没有发现再脱位与既往治疗有关,但本研究认为对于IOS为Ⅲ度且有既往治疗的髋关节,建议行切开复位。
IOS所代表的是髋关节复位后的内侧间隙,与MDP不同,属于定性指标,不受造影图像放大倍数的影响。结合本组不同病理类型DDH的IOS分度情况,可认为:Ⅰ度为同心圆复位,Ⅱ度和Ⅲ度为非同心圆复位。从预防再脱位的角度来看,Ⅰ度和Ⅱ度的髋关节能够采用闭合复位,Ⅲ度的髋关节应谨慎选择闭合复位。
本组有1例15月龄患儿采用切开复位石膏固定术,IOS为Ⅲ度,术后也发生了再脱位。回顾手术记录发现,该患儿髋臼发育差,切开复位后仍不稳定,股骨头外上方覆盖不足,因此单纯石膏固定没能维持复位。对于这类患儿,术中需根据髋臼形态决定是否行骨盆截骨,以改善股骨头覆盖,增加髋关节稳定性[14, 15]。这一特殊病例表明,DDH术后再脱位的影响因素很复杂,难以用单一指标将再脱位发生率降低至零,临床中应结合多种标准进行综合评估,选择最佳治疗方案。
本研究存在以下不足之处:①作为回顾性研究,本文虽能说明IOS与DDH再脱位有关,但是未能证明二者存在因果关系。Ⅲ度IOS是否一定会引起再脱位还需前瞻性研究来证实。②切开复位的病例,因术中切开关节囊,影响造影效果,未再次造影观察IOS的改善情况。
综上所述,IOS与DDH术后再脱位有一定关系,IOS为Ⅲ度的髋关节如行闭合复位,再脱位的风险较高。IOS属于定性指标,与其他造影标准相比,有易于判定的优势,便于临床推广应用。临床实际操作中,可结合其他标准综合判定,以提高DDH复位成功的概率,降低术后再脱位的发生率。
| 1 |
Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip:functional and radiographic results after an average of thirty years[J]. J Bone Joint Surg Am, 1994, 76(12): 1777-17792. DOI:10.2106/00004623-199412000-00004. |
| 2 |
中华医学会小儿外科分会骨科学组, 中华医学会骨科学分会小儿创伤矫形学组. 发育性髋关节发育不良临床诊疗指南(0~2岁)[J]. 中华骨科杂志, 2017, 37(11): 641-650. DOI:10.3760/cma.j.issn.0253-2352.2017.11.001. Pediatric Orthopedic Group of Surgery Branch and Pediatric Trauma & Orthopedic Group. Chinese Medical Association:Detection and treatment of pediatric developmental dysplasia of the hip in children aged up to two year:clinical practice guideline[J]. Chin J Orthop, 2017, 37(11): 641-650. DOI:10.3760/cma.j.issn.0253-2352.2017.11.001. |
| 3 |
Gornitzky AL, Georgiadis AG, Seeley MA, et al. Does perfusion MRI after closed reduction of developmental dysplasia of the hip reduce the incidence of avascular necrosis?[J]. Clin Orthop Relat Res, 2016, 474(5): 1153-1165. DOI:10.1007/s11999-015-4387-6. |
| 4 |
Shirai Y, Wakabayashi K, Wada I, et al. Magnetic resonance imaging evaluation of the labrum to predict acetabular development in developmental dysplasia of the hip:A STROBE compliant study[J]. Medicine (Baltimore), 2017, 96(21): e7013. DOI:10.1097/MD.0000000000007013. |
| 5 |
Gans I, Sankar WN. The medial dye pool revisited:correlation between arthrography and MRI in closed reductions for DDH[J]. J Pediatr Orthop, 2014, 34(8): 787-790. DOI:10.1097/bpo.0000000000000187. |
| 6 |
Forlin E, Choi IH, Guille JT, et al. Prognostic factors in congenital dislocation of the hip treated with closed reduction.The importance of arthrographic evaluation[J]. J Bone Joint Surg Am, 1992, 74(8): 1140-1152. DOI:10.2106/00004623-199274080-00003. |
| 7 |
李天友, 王延宙, 张敏刚, 等. "三线一点"法在发育性髋关节脱位X线分型中的应用探讨[J]. 中华小儿外科杂志, 2017, 38(7): 516-520. DOI:10.3760/cma.j.issn.0253-3006.2017.07.007. Li TY, Wang YZ, Zhang MG, et al. A new radiographic classification of 'three lines & one point' for developmental dysplasia of the hip[J]. Chin J Pediatr Surg, 2017, 38(7): 516-520. DOI:10.3760/cma.j.issn.0253-3006.2017.07.007. |
| 8 |
Ramsey PL, Hensinger RN. Congenital dislocation of the hip associated with central core disease[J]. J Bone Joint Surg Am, 1975, 57(5): 648-651. DOI:10.2106/00004623-197557050-00011. |
| 9 |
Severin E. Contributions to the knowledge of congenital dislocation of the hip joint.Late results of closed reduction and arthrographic studies of recent cases[J]. Acta Chir Scand, 1941(84): 1-142. |
| 10 |
Drummond DS, O'Donnell J, Breed A, et al. Arthrography in the evaluation of congenital dislocation of the hip[J]. Clin Orthop Relat Res, 1989(243): 148-156. |
| 11 |
Lonnerholm T. Arthrography of the hip in children:technique, normal anatomy and findings in unstable hip joints[J]. Acta Radiol Diagn (Stockh), 1980, 21(2): 279-292. |
| 12 |
Race C, Herring JA. Congenital dislocation of the hip:an evaluation of closed reduction[J]. J Pediatr Orthop, 1983, 3(2): 166-172. DOI:10.1097/01241398-198305000-00004. |
| 13 |
贾国强, 孙军, 王恩波. "安全带征"在2岁以内发育性髋关节脱位治疗方式的应用探讨[J]. 中华小儿外科杂志, 2018, 39(4): 290-295. DOI:10.3760/cma.j.issn.0253-3006.2018.04.011. Jia GQ, Sun J, Wang EB. Application of "safety belt sign" in the treatment of developmental dysplasia of the hip in children aged under 2 years[J]. Chin J Pediatr Surg, 2018, 39(4): 290-295. DOI:10.3760/cma.j.issn.0253-3006.2018.04.011. |
| 14 |
姜海, 苗武胜, 吴革, 等. 发育性髋关节发育不良儿童髋臼形态学病理分型的探讨[J]. 临床小儿外科杂志, 2016, 15(2): 179-182. DOI:10.3969/j.issn.1671-6353.2016.02.021. Jiang H, Miao WS, Wu G, et al. Analysis of acetabular morphological pathology types in developmental dysplasia of the hip in children[J]. J Clin Ped Sur, 2016, 15(2): 179-182. DOI:10.3969/j.issn.1671-6353.2016.02.021. |
| 15 |
张立军, 吉士俊, 李连永. 发育性髋关节发育不良的诊治策略[J]. 临床小儿外科杂志, 2012, 11(3): 161-165. DOI:10.3969/j.issn.1671-6353.2012.03.001. Zhang LJ, Ji SJ, Li LY. Diagnostic and therapeutic strategies of developmental dysplasia of the hip[J]. J Clin Ped Sur, 2012, 11(3): 161-165. DOI:10.3969/j.issn.1671-6353.2012.03.001. |
 2020, Vol. 19
2020, Vol. 19


