2. 首都医科大学附属北京儿童医院胸外科 国家儿童医学中心(北京, 100045);
3. 首都医科大学附属北京儿童医院病理科 国家儿童医学中心(北京, 100045)
2. Department of Thoracic Surgery, National Center of Children's Health, Beijing Children Hospital, Capital Medical University, Beijing 100045, China;
3. Department of Pathology, National Center of Children's Health, Beijing Children Hospital, Capital Medical University, Beijing 100045, China
儿童腹腔内肺隔离症(intra-abdominal extralobar pulmonary sequestration, IEPS)是一种罕见的先天性肺发育畸形,占所有叶外型肺隔离症的8% ~15%[1, 2]。IEPS主要位于左上腹,产前往往通过B超、MRI等检查发现,产后无显著临床症状,需与神经母细胞瘤(neuroblastoma, NB)等疾病进行鉴别,手术切除肿物进行病理检查是早期诊断的唯一方式[3, 4]。因此产前随访、合理诊断,产后评估、正确治疗对于该疾病的预后至关重要。本研究通过回顾性分析首都医科大学附属北京儿童医院收治的4例IEPS患儿的临床资料,并结合近30年相关文献进行分析,探讨该病的临床特征、病理类型、治疗方法及预后情况,为临床制定正确诊疗方案提供依据。
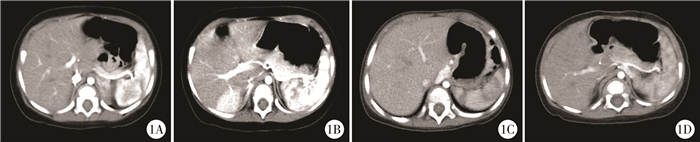
材料与方法 一、临床资料2007年6月至2018年6月首都医科大学附属北京儿童医院共收治IEPS患儿4例,男女比例为1:1,均经产前B超发现“腹腔占位/肾上腺占位”,平均孕龄22.5周,其中最早确诊1例为孕16周。2例产前行MRI检查,诊断“隔离肺/神经母细胞瘤”,建议产后密切随访。4例均为足月产,平均出生体重3.2 kg,无合并其他先天畸形,产后至术前均无显著临床症状,无家族遗传病史。4例术前行彩色多普勒B超及腹部增强CT+大血管重建检查,2例位于左肾上腺区,1例位于右肾上腺区,1例位于降主动脉右侧。2例可疑动脉供血(图 1)。4例均产后随访6个月以上,未见肿物明显变化后行手术治疗,平均手术年龄10个月,拟行腹腔镜手术。3例行腹腔镜中转开腹肿物切除术,2例因腔镜探查未见明确肿物,1例因肿物与周围组织粘连紧密,手术时间平均为188 min,术中出血分别为10 mL、20 mL与80 mL(术中输注红细胞1个单位),切除肿物平均长径2.7 cm。1例行腹腔镜肿物切除术,手术时长180 min,术中出血5 mL,切除肿物长径5.0 cm。术中明确3例肿物供血,主要为腹主动脉及其分支,同时1例肝动脉及门静脉右支供血。患儿术后均恢复良好,平均住院6.5 d。4例IEPS患儿的临床资料见表 1。
|
Download:
|
| 图 1 儿童腹腔内肺隔离症胸/腹部增强CT图 注 1A:提示左侧肾上腺背内侧软组织包块,大小3.0 cm×2.0 cm×1.7 cm; 1B:提示肝右叶后段局限性强化灶,大小约3.0 cm×3.0 cm×2.0 cm,由门脉右支、肝动脉分支及腹主动脉分支供血; 1C:提示膈角降主动脉右旁三角形软组织包块,大小2.0 cm×1.8 cm×1.0 cm,血供丰富; 1D:提示食管右下缘膈下腹膜后软组织包块,大小5.0 cm×5.0 cm×1.0 cm,腹腔干分支供血 Fig. 1 Chest/abdomen contrast-enhanced CT | |
|
|
表 1 首都医科大学附属北京儿童医院收治的IEPS患儿临床资料 Table 1 Clinical data of IEPS children at Beijing Children's Hospital |
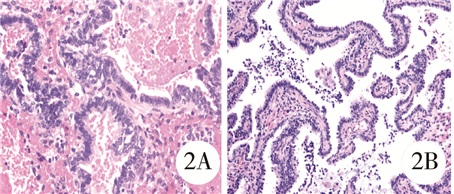
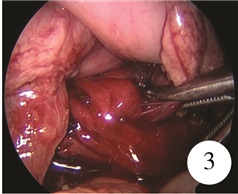
病理检查,肉眼下均为灰红色组织,大小不等,部分被覆暗紫色肺膜,切面肺组织光滑,质软,局部可见灰白色小血管(图 2)。腔镜下所见:①(腹腔)隔离肺并先天性肺气道畸形(Ⅱ型),继发慢性间质炎并充血、出血;②(肝右叶后方)隔离肺并先天性肺气道畸形(Ⅲ型):肺泡内出血并见少量组织细胞浸润,肺组织内有少量厚壁畸形血管;③(腹腔内膈肌角)隔离肺并先天性肺气道畸形(Ⅱ型);④(腹腔)隔离肺并先天性肺气道畸形(Ⅲ型)(图 3)。
|
Download:
|
| 图 2 肺隔离症患儿病理形态学检查(HE染色,×200) 注 2A:(腹腔)隔离肺并先天性肺气道畸形(Ⅱ型),继发慢性间质炎并充血出血;2B:(腹腔)隔离肺并先天性肺气道畸形(Ⅲ型) Fig. 2 Histopathological examination (H & E stain, ×200) | |
|
Download:
|
| 图 3 儿童腹腔内肺隔离症病变组织肉眼观察 Fig. 3 Macroscopic inspection | |
通过检索万方、维普、CNKI、Pubmed、Medline数据库,检索关键词:叶外型肺隔离症/隔离肺(extralobar pulmonary sequestration)、膈下/腹腔内(infradiaphragmatic/intraabdominal)。检索截止日期:2018年6月。剔除成人病例及无法获得全文资料的儿童病例,共有中英文献报道胎儿或儿童膈下/腹腔内肺隔离症43例[5-32]。
结 果 一、本院4例患儿预后本院4例患儿在术后3个月、6个月、3年半、4年随访发现,均无术后并发症,生长发育良好,详见表 1。
二、文献分析文献报道43例胎儿/儿童腹腔内肺隔离症,结合本组4例,共47例患儿,其一般资料见表 2。除18例未报道性别,其余男女比例为21:8。44例产前发现病变平均孕龄为25(IQR:12~37)周,2例(8.5%)未报道病变发现时间,1例产后B超发现,其中病变发现最早者为孕12周。产前彩色多普勒超声均提示患儿腹部肿物或肾上腺区肿物,10例怀疑NB,7例怀疑IEPS,1例怀疑CPAM。5例告知父母相关可能后终止妊娠,尸检病理提示肺隔离症。其余42例患儿全部顺产,其中7例(7/42,16.7%)产后伴发先天畸形(3例合并膈疝;1例合并单纯消化道畸形;1例合并食管裂孔疝;1例合并胃重复囊肿及双侧脉络丛囊肿;1例合并心血管畸形)。产后5例行保守治疗,其中3例因保守过程中肿物增大,遂行手术治疗,共40例患儿行手术治疗。
|
|
表 2 截至2018年6月文献报道的胎儿或儿童IEPS一般资料 Table 2 General profiles of fetal or pediatric IEPS reported in literature prior to June 2018 |
手术治疗的IEPS患儿相关诊疗情况见表 3。除2例诊断方式不详外,术前30例(30/38,78.9%)行B超检查,27例(27/38,71.1%)行胸部/腹部增强CT,15例(15/38,39.5%)行胸部/腹部MRI,其中B超联合增强CT进行术前评估应用最为广泛(10/38, 26.3%),同时结合胸片、骨穿、穿刺活检、MIBG(metaiodoenzylguanidine)检查、骨扫描等辅助检查。40例手术患儿中,11例(11/40, 27.5%)诊断NB,9例(9/40, 22.5%)诊断IEPS,3例(3/40, 7.5%)诊断CPAM,1例(1/40, 2.5%)诊断畸胎瘤。
|
|
表 3 截至2018年6月文献报道的手术治疗儿童IEPS诊疗情况(n=40) Table 3 Diagnosis and treatment of surgical IEPS before June 2018 (n=40) |
40例手术治疗患儿中(1例手术方式不详),25例(25/40, 62.5%)行开腹肿物切除术,11例(11/ 40, 27.5%)行腹腔镜下肿物切除术,3例(3/40, 7.5%)行腹腔镜中转开腹手术(中转开腹原因见表 1)。除6例术时年龄不详外,生后≤6个月行手术治疗患儿25例(25/40, 73.5%),>6个月行手术治疗患儿9例(9/40, 22.5%)。分析所有患儿的辅助检查及手术过程(2例肿物位置不详),发现32例(32/40, 80.0%)肿物位于左腹,5例(5/40, 12.5%)位于右腹,1例(1/40, 2.5%)位于中线区域。切除的病变肿物平均长径约3.0 cm(IQR:2.8~3.9), 但有20例肿物长径不详。肿物供血血管较为集中(19例肿物供血来源不详),其中供血为腹主动脉及其分支16例(16/21,76.2%)、脾动脉2例(2/21,9.5%)、胃相关动脉1例(1/21,4.8%)、肺动脉1例(1/21,4.8%)、肾上腺来源动脉1例(1/21,4.8%),2例(2/21,9.5%)位于右腹部的肿物除腹主动脉外合并肝动脉和门静脉分支或膈下动脉和肾动脉供血。术后病理结果回报40例均为肺隔离症,其中有22例(22/40,55.0%)伴有CPAM(12例CPAM Ⅱ型,2例CPAM Ⅲ型,8例未明确)。40例手术治疗患儿预后良好。2例保守治疗患儿生后随访6~8个月肿物开始缩小,18个月时肿物退化完全,且未行手术治疗。
讨 论肺隔离症(pulmonary sequestration, PS)是一种少见的肺支气管及前原肠畸形疾病,发病率约0.15% ~1.8%[33]。据相关文献报道,PS可能是孕4周时前原肠意外发出异位肺芽,随妊娠进展逐渐接受体循环的血液供应并发展成与正常气道无交通的混乱肺结构,并通过静脉回流至肺静脉或体循环[4, 34]。叶外型肺隔离症(extralobar sequestration, ELS)约占所有PS的25%,其特点是独立于正常肺组织且有完整脏层胸膜覆盖的异常肺组织,很少与呼吸道和胃肠道相通,所以极少出现囊性扩张和感染症状[35, 36]。腹腔内肺隔离症(intra-abdominal extralobar pulmonary sequestration, IEPS)作为叶外型隔离肺的一种,发生率仅占肺隔离症的2.5%,主要发生于左上腹,至今对其发病机制及诊疗方式仍存在较大争议[37, 38]。
Duygulu和Yucel等[31, 39]报道约50% ~60%的叶外型肺隔离症患儿生后伴有膈疝、心血管畸形及肺组织畸形等先天畸形,并伴随相应临床表现,因而超过60%患儿生后6个月内确诊EPS。但回顾以往文献,发现IEPS患儿合并先天畸形比例较其他类型EPS少,合并畸形比例不到20%[32]。本研究也证实这一观点,并且回顾所有文献,发现无一例患儿产后伴随临床表现。同时Conran和Stocker曾报道叶外型肺隔离症约有50%合并先天性肺气道畸形,这可能与二者胚胎发育起源相似有关[40-42]。迄今为止,除我中心收治的2例IEPS合并CPAM Ⅲ型外,其余报道的腹腔内肺隔离症均合并CPAM Ⅱ型。据Nakata[43]报道,CPAM Ⅲ型存在合并心血管畸形的可能,往往胎死腹中,因而出生后进行手术治疗的CPAM Ⅲ型病例少,这要求我们密切随访这2例患儿的预后,观察其是否与合并CPAM Ⅱ型预后存在差异。
绝大多数IEPS患儿于母亲孕中期(13~27周)产检发现,无特异临床表现。目前文献报道最早母亲孕龄为12周[17]。彩色多普勒B超和MRI是主要的产前诊断方式。B超常常表现为均质高回声肿物,伴或不伴囊性结构,但对胎儿是否产生影响无法判断,因此医生往往建议定期随访B超或再行MRI检查进一步明确诊断[32]。B超作为常规产前检查方式,因其对异质肿块的良好空间分辨率及对组织相对运动的动态观察,是产前诊断IEPS的首选方式,尤其是彩色多普勒B超对胎儿肺外大血管供应具有良好的诊断价值[31, 44]。但超声同样存在以下局限性:①探头视野有限,对于羊水过多或过少、过于肥胖及多胎妊娠的孕妇无法清晰显示胎儿胸腹部结构;②对于无大血管供应/多血管供应的IEPS,较难与CPAM相鉴别;③对超声仪器及操作检查者的经验有很高的要求[45, 46]。MRI作为产前诊断较好的补充手段,能够直接显示胎儿肺隔离症的范围和形态,但无法判断与膈肌的位置关系及肿物性质[47]。因此IEPS仍需与神经母细胞瘤、先天性肺气道畸形及畸胎瘤等相鉴别[22]。结合以往流产患儿病例,产前定期随访判断病情对于IEPS的预后至关重要[30]。
与叶内型肺隔离症(intralobar sequestration, ILS)反复感染和支气管阻塞表现不同,IEPS患儿往往无临床表现,目前报道所有患儿产后均无临床表现,因此需进一步随访及综合评估加以鉴别[32, 36, 48]。对于产前怀疑IEPS的患儿,产后无明确临床表现者,需密切随访观察,目前国际上对于IEPS仍没有统一的随访方案,一般随访6~12个月。彩色多普勒B超仍是产后随访的最佳方式[31]。早期超声引导经皮穿刺曾作为良好的辅助诊断方式,但由于肿物位置毗邻腹主动脉、肿物大小不一、组织结构差异等原因,存在穿刺后病理回报不准确的可能,已不作为常规诊断方式[1, 12]。同时产后胸部/腹部增强CT的使用,对肿物的三维结构、具体位置和血液供应有了更进一步的了解[49]。除此以外,为排除恶性肿瘤可能,术前可完善相关肿瘤标志物检查,必要时行MIBG及骨扫描等辅助检查。但回顾本研究所有文献,仍有22.5%的患儿术前明确诊断IEPS。
手术切除病变肿物是明确诊断和治疗的主要方式[1, 2]。回顾以往病例,关于手术治疗主要存在以下几点争议:①无症状IEPS是否需要手术:Chowdhury等[24]报道2例行保守治疗的IEPS患儿,产后定期复查B超6个月后肿物开始退化,随访期间患儿均发育良好,无并发任何疾病,结合所有6个月后行手术治疗的患儿,消退率为28.6%(2/7);虽然报道绝大多数的IEPS随患儿成长无临床表现,但仍有病例报道成人IEPS有并发感染的可能[24, 37]。②最佳手术时间的选择:本研究中73.5%的患儿生后6个月内进行手术(25/34),且术后均无并发症。但由于缺乏长期随访,早期手术(尤其是新生儿期手术)是否有利于患儿剩余肺组织生长,从而尽可能减少对正常肺功能影响尚不清楚。③最佳手术方式的选择:21世纪以来,由于腹腔镜能够对病变进行细致的解剖,同时具有较好识别血管并结扎,手术创伤小,术后恢复快等优点,越来越多的肺隔离症患儿接受腔镜手术,研究也发现无论是叶内型肺隔离症还是叶外型肺隔离症,腔镜手术均较开放手术操作时间短,出血量少[34];但因超过50%的IEPS患儿肿物长径 < 3 cm或位于腹部肝脏深部,邻近脏器较多,腹腔镜手术暴露术野困难,无法明确肿物位置与界限,尤其是术前考虑粘连严重的患儿,腹腔镜手术并非最佳选择。但无论何种术式,因肿物供血血管主要为腹主动脉及其分支,虽位于右上腹的肿物伴有血供复杂等特点,术中对血管的精细解剖并结扎仍是手术的要点及难点之一[5, 28]。
综上所述,腹腔内肺隔离症往往经产前B超于母亲孕中期发现,产前定期复查对其诊断及预后具有重要意义。但因IEPS患儿往往无临床症状及体征,出生后仍需借助多种辅助检查方式加以鉴别,综合评估以选择合适的手术方案。对于行保守治疗的患儿,需定期随访,以明确腹腔内肿物是否完全退化。手术切除肿物是早期诊断IEPS的最主要方式,肿物完整切除的患儿预后良好,目前可作为根治IEPS的最佳方式,需进一步随访研究判断切除病变肿物后是否对患儿肺功能及远期生长发育产生影响。
| 1 |
Costa MR, Costa TR, Leite MS, et al. Atypical presentation of intra-abdominal extralobar pulmonary sequestration detected in prenatal care:a case report[J]. Rev Paul Pediatr, 2016, 34(2): 243-246. DOI:10.1016/j.rpped.2015.10.003. |
| 2 |
Pires CR, Czapkowski A, Júnior EA. Diagnosis of Intra-Abdominal Extralobar Pulmonary Sequestration by means of Ultrasound in a Neonate[J]. Case Rep Pediatr, 2013, 2013: 623102. DOI:10.1155/2013/623102. |
| 3 |
Kim HJ, Kim JH, Chung SK, et al. Coexistent intralobar and extralobar pulmonary sequestration:imaging findings[J]. Can Respir J, 1993, 160(6): 1199-200. DOI:10.2214/ajr.160.6.8498214. |
| 4 |
Laje P, Martinez-Ferro M, Grisoni E, et al. Intraabdominal pulmonary sequestration.A case series and review of the literature[J]. J Pediatr Surg, 2006, 41(7): 1309-1312. DOI:10.1016/j.jpedsurg.2006.03.049. |
| 5 |
Mariona F, Mcalpin G, Zador I, et al. Sonographic detection of fetal extrathoracic pulmonary sequestration[J]. J Ultrasound Med, 1986, 5(5): 283-285. DOI:10.7863/jum.1986.5.5.283. |
| 6 |
Baumann H, Kirkinen P, Huch A. Prenatal ultrasonographic findings in extralobar subdiaphragmatic lung sequestration-a case report[J]. J Perinat Med, 1988, 16(1): 67-69. DOI:10.1515/jpme.1988.16.1.67. |
| 7 |
Davies RP, Ford WD, Lequesne GW, et al. Ultrasonic detection of subdiaphragmatic pulmonary sequestration in utero and postnatal diagnosis by fine-needle aspiration biopsy[J]. J Ultrasound Med, 1989, 8(1): 47-49. DOI:10.7863/jum.1989.8.1.47. |
| 8 |
Brill PW, Winchester P, Kosovsky P, et al. Imaging of prenatally detected intra-abdominal extralobar pulmonary sequestration[J]. Clin Imaging, 1990, 14(2): 152-156. DOI:10.1016/0899-7071(90)90013-2. |
| 9 |
Black MD, Bass J, Martin DJ, et al. Intraabdominal pulmonary sequestration[J]. J Pediatr Surg, 1991, 26(12): 1381-1383. DOI:10.1016/0022-3468(91)91038-Z. |
| 10 |
Brink DA, Balsara ZN. Prenatal ultrasound detection of intra-abdominal pulmonary sequestration with postnatal MRI correlation[J]. Pediatr Radiol, 1991, 21(3): 227. DOI:10.1007/BF02011055. |
| 11 |
Morier J, Foletti GB. Antenatal Detection of Subdiaphragmatic Pulmonary Sequestration:A Case Report[J]. Eur J Pediatr Surg, 1994, 4(3): 173-175. DOI:10.1055/s-2008-1066094. |
| 12 |
White J, Chan YF, Neuberger S, et al. Prenatal sonographic detection of intra-abdominal extralobar pulmonary sequestration:Report of three cases and literature review[J]. Prenat Diagn, 1994, 14(8): 653-658. DOI:10.1002/pd.1970140802. |
| 13 |
Torrelo A, Simal G, Pozo J, et al. Extra-Lobar Pulmonary Sequestration with Prenatal Diagnosis.A Report of 5 Cases and Review of the Literature[J]. Eur J Pediatr Surg, 1995, 5(4): 235-237. DOI:10.1055/s-2008-1066213. |
| 14 |
Curtis MR, Mooney DP, Vaccaro TJ, et al. Prenatal ultrasound characterization of the suprarenal mass:distinction between neuroblastoma and subdiaphragmatic extralobar pulmonary sequestration[J]. J Ultrasound Med, 1997, 16(2): 75-83. DOI:10.7863/jum.1997.16.2.75. |
| 15 |
Morad NA, Almalki T, Etahir M. Intra-abdominal pulmonary sequestration:Diagnostic difficulties[J]. Pathology, 1997, 29(2): 218. DOI:10.1080/00313029700169904. |
| 16 |
Curtis MR, Mooney DP, Vaccaro TJ, et al. Prenatal ultrasound characterization of the suprarenal mass:distinction between neuroblastoma and subdiaphragmatic extralobar pulmonary sequestration[J]. J Ultrasound Med, 1997, 16(2): 75-83. DOI:10.7863/jum.1997.16.2.75. |
| 17 |
Gross E, Chen MK, Lobe TE, et al. Infradiaphragmatic extralobar pulmonary sequestration masquerading as an intra-abdominal, suprarenal mass[J]. Pediatr Surg Int, 1997, 12(7): 529-531. DOI:10.1007/BF01258719. |
| 18 |
Marcelo MF, Laura S, Vickie AF, et al. Minimally invasive resection of prenatally diagnosed thoracic and abdominal pulmonary sequestrations[J]. Pediatric Endosurgery & Innovative Techniques, 2000, 4(2): 137-141. DOI:10.1039/b417588c. |
| 19 |
Chan YF, Oldfield R, Vogel S, et al. Pulmonary sequestration presenting as a prenatally detected suprarenal lesion in a neonate[J]. J Pediatr Surg, 2000, 35(9): 1367-1369. DOI:10.1053/jpsu.2000.9337. |
| 20 |
Pumberger W, Moroder W, Wiesbauer P. Intraabdominal extralobar pulmonary sequestration exhibiting cystic adenomatoid malformation:prenatal diagnosis and characterization of a left suprarenal mass in the newborn[J]. Abdom Imaging, 2001, 26(1): 28-31. DOI:10.1007/s002610000096. |
| 21 |
Danielson PD, Sherman NJ. Laparoscopic removal of an abdominal extralobar pulmonary sequestration[J]. J Pediatr Surg, 2001, 36(11): 1653-1655. DOI:10.1053/jpsu.2001.27942. |
| 22 |
Carrasco R, Castañón M, San VB, et al. Extralobar infradiaphragmatic pulmonary sequestration with a digestive communication[J]. J Thorac Cardiovasc Surg, 2002, 123(1): 188-189. DOI:10.1067/mtc.2002.118040. |
| 23 |
Singal AK, Agarwala S, Seth T, et al. Intra-abdominal extralobar pulmonary sequestration presenting antenatally as a suprarenal mass[J]. Indian J Pediatr, 2004, 71(12): 1137-1139. DOI:10.1007/BF02829832. |
| 24 |
Chowdhury M, Samuel M, Ramsay A, et al. Spontaneous postnatal involution of intraabdominal pulmonary sequestration[J]. J Pediatr Surg, 2004, 39(8): 1273-1275. DOI:10.1016/j.jpedsurg.2004.04.022. |
| 25 |
Zee DCVD, Bax KM. Laparoscopic resection of intra-abdominal extralobar pulmonary sequestration[J]. Pediatr Surg Int, 2005, 21(10): 841. DOI:10.1007/s00383-005-1526-2. |
| 26 |
Alaish SM, Greenspon J, Strauch ED, et al. Intraabdominal pulmonary sequestration presenting with elevated urinary normetanephrine levels[J]. J Pediatr Surg, 2009, 44(3). DOI:10.1016/j.jpedsurg.2008.11.040. |
| 27 |
刘炜, 蔡爱露, 赵丹. 产前超声诊断胎儿隔离肺1例[J]. 中国临床医学影像杂志, 2008, 19(6): 456-456. DOI:10.3969/j.issn.1008-1062.2008.06.034. Liu W, Cai AL, Zhao D. Prenatal ultrasonography in the diagnosis of fetal pulmonary sequestration:report of one case[J]. J Chin Clin Med Imag, 2008, 19(6): 456-456. DOI:10.3969/j.issn.1008-1062.2008.06.034. |
| 28 |
Adaletli I, Uludag S. Intraabdominal extrapulmonary sequestration diagnosed by color doppler ultrasound at 22 weeks' gestation[J]. J Clin Ultrasound, 2013, 41(4): 251-254. DOI:10.1002/jcu.21924. |
| 29 |
Chouikh T, Berteloot L, Revillon Y, et al. Extralobar pulmonary sequestration with combined gastric and intradiaphragmatic locations[J]. Pediatr Pulmonol, 2014, 49(5): 512-514. DOI:10.1002/ppul.22891. |
| 30 |
He W, Luo S J, Chu L. Extralobar pulmonary sequestration in the abdominal cavity:an ultrasound case report[J]. Quant Imaging Med Surg, 2013, 3(1): 59-60. DOI:10.3978/j.issn.2223-4292.2013.02.02. |
| 31 |
Duygulu G, Cebeci H, Ozer T, et al. Intraabdominal extrapulmonary sequestration in an infant diagnosed by color Doppler ultrasound[J]. J Pediatr Surg Case Rep, 2015, 3(6): 249-251. DOI:10.1016/j.epsc.2015.04.005. |
| 32 |
徐赣琼, 周启昌, 周嘉炜, 等. 胎儿腹腔内隔离肺的产前超声诊断及临床价值[J]. 中华超声影像学杂志, 2017, 26(2): 132-137. DOI:10.3760/cma.j.issn.1004-4477.2017.02.011. Xu GQ, Zhou QC, Zhou JW, et al. Prenatal diagnosis of intraabdominal extralobar pulmonary sequestration by ultrasound[J]. Chin J Ultrasonogr, 2017, 26(2): 132-137. DOI:10.3760/cma.j.issn.1004-4477.2017.02.011. |
| 33 |
Zhang H, Tian J, Chen Z, et al. Retrospective study of prenatal diagnosed pulmonary sequestration[J]. Pediatr Surg Int, 2014, 30(1): 47. DOI:10.1007/s00383-013-3434-1. |
| 34 |
张娜, 曾骐, 陈诚豪, 等. 胸腔镜手术与开胸手术对不同类型小儿肺隔离症的适应性研究[J]. 临床小儿外科杂志, 2018, 17(5): 336-340. DOI:10.3969/j.issn.1671-6353.2018.05.005. Zhang N, Zeng Q, Chen CH, et al. Comparative study of outcomes for thoracoscopic versus open resection of pulmonary sequestration at a single pediatric institution:a report of 208 cases[J]. J Clin Ped Sur, 2018, 17(05): 336-340. DOI:10.3969/j.issn.1671-6353.2018.05.005. |
| 35 |
Lee JH, Kim MJ. Intra-diaphragmatic extralobar pulmonary sequestration in adult[J]. J Cardiothorac Surg, 2014, 20(9): 112. DOI:10.1186/1749-8090-9-112. |
| 36 |
Kim HK, Choi YH, Ryu SM, et al. Infected Infradiaphragmatic Retroperitoneal Extralobar Pulmonary Sequestration:A Case Report[J]. J Korean Med Sci, 2005, 20(6): 1070-1072. DOI:10.3346/jkms.2005.20.6.1070. |
| 37 |
Moreno-Sanz C, Herrero Bogajo ML, Picazo-Yeste J, et al. Intra-abdominal pulmonary secuestration as an exceptional cause of abdominal mass in the adult[J]. Int J Surg Case Rep, 2013, 4(11): 997-999. DOI:10.1016/j.ijscr.2013.08.019. |
| 38 |
Ulys A, Samalavicius NE, Cicenas S, et al. Extralobar pulmonary sequestration[J]. Int Med Case Rep J, 2008, 105(6): 833-834. DOI:10.1016/j.surg.2007.06.012. |
| 39 |
Yucel O, Gurkok S, Gozubuyuk A, et al. Diagnosis and surgical treatment of pulmonary sequestration[J]. Thorac Cardiovasc Surg, 2008, 56: 154-157. DOI:10.1055/s-2007-965572. |
| 40 |
Conran RM, Stocker JT. Forensic Pathology of Infancy and Childhood[M]. Springer New York, 2014: 59-80.
|
| 41 |
Conran RM, Stocker JT. Extralobar sequestration with frequently associated congenital cystic adenomatoid malformation, type 2:report of 50 cases[J]. Pediatr Dev Pathol, 1999, 2(5): 454-463. DOI:10.1007/s100249900149. |
| 42 |
Mclean SE, Pfeifer JD, Siegel MJ, et al. Congenital cystic adenomatoid malformation connected to an extralobar pulmonary sequestration in the contralateral chest:common origin?[J]. J Pediatr Surg, 2004, 39(8). DOI:10.1016/j.jpedsurg.2004.04.044. |
| 43 |
Nakata M, Yoshida S, Saito T, et al. Hybrid video-assisted thoracoscopic surgery lobectomy of fissureless congenital cystic adenomatoid malformation:a case report[J]. J Med Case Rep, 2015, 9(1): 1-4. DOI:10.1186/1752-1947-9-23. |
| 44 |
Brink DA, Balsara ZN. Prenatal ultrasound detection of intra-abdominal pulmonary sequestration with postnatal MRI correlation[J]. Pediatr Radiol, 1991, 21(3): 227-227. DOI:10.1007/BF02011055. |
| 45 |
刘锋, 关键, 刘树学, 等. 胎儿肺隔离症的MRI诊断[J]. 放射学实践, 2014, 29(5): 560-563. Liu F, Guan J, Liu SX. MR imaging of bronchopulmonary sequestration in the fetus[J]. Radiol Practice, 2014, 29(5): 560-563. |
| 46 |
叶志球, 邓志真, 陈文俊, 等. MRI与超声对胎儿肺囊性疾病的诊断价值对照[J]. 实用放射学杂志, 2015, 31(7): 1171-1174. DOI:10.3969/j.issn.1002-1671.2015.07.028. Ye ZQ, Deng ZZ, Chen WJ, et al. Diagnostic value of MR imaging in congenital cystic lung disease:comparative study with ultrasound[J]. J Pract Radiol, 2015, 31(7): 1171-1174. DOI:10.3969/j.issn.1002-1671.2015.07.028. |
| 47 |
Hill BJ, Joe BN, Qayyum A, et al. Supplemental value of MRI in fetal abdominal disease detected on prenatal sonography:preliminary experience[J]. AJR Am J Roentgenol, 2005, 184(3): 993-998. DOI:10.2214/ajr.184.3.01840993. |
| 48 |
Al-Salem, Ahmed H. An Illustrated Guide to Pediatric Surgery[M]. Springer International Publishing, 2014: 365-372.
|
| 49 |
Saeed A, Kazmierski M, Khan A, et al. Congenital lung lesions:preoperative three-dimensional reconstructed CT scan as the definitive investigation and surgical management[J]. Eur J Pediatr Surg, 2013, 23(1): 53-56. DOI:10.1055/s-0033-1333890. |
 2019, Vol. 18
2019, Vol. 18


