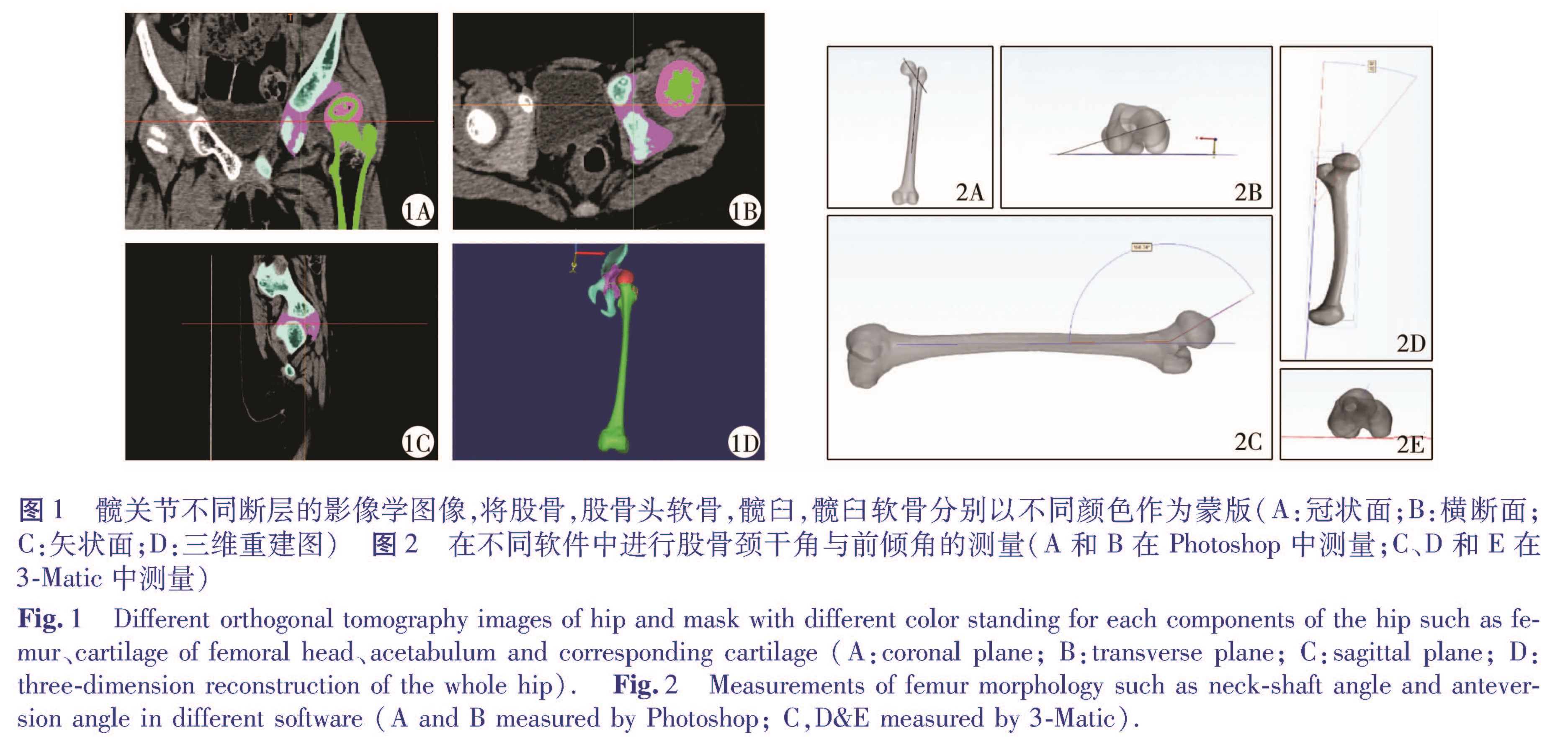
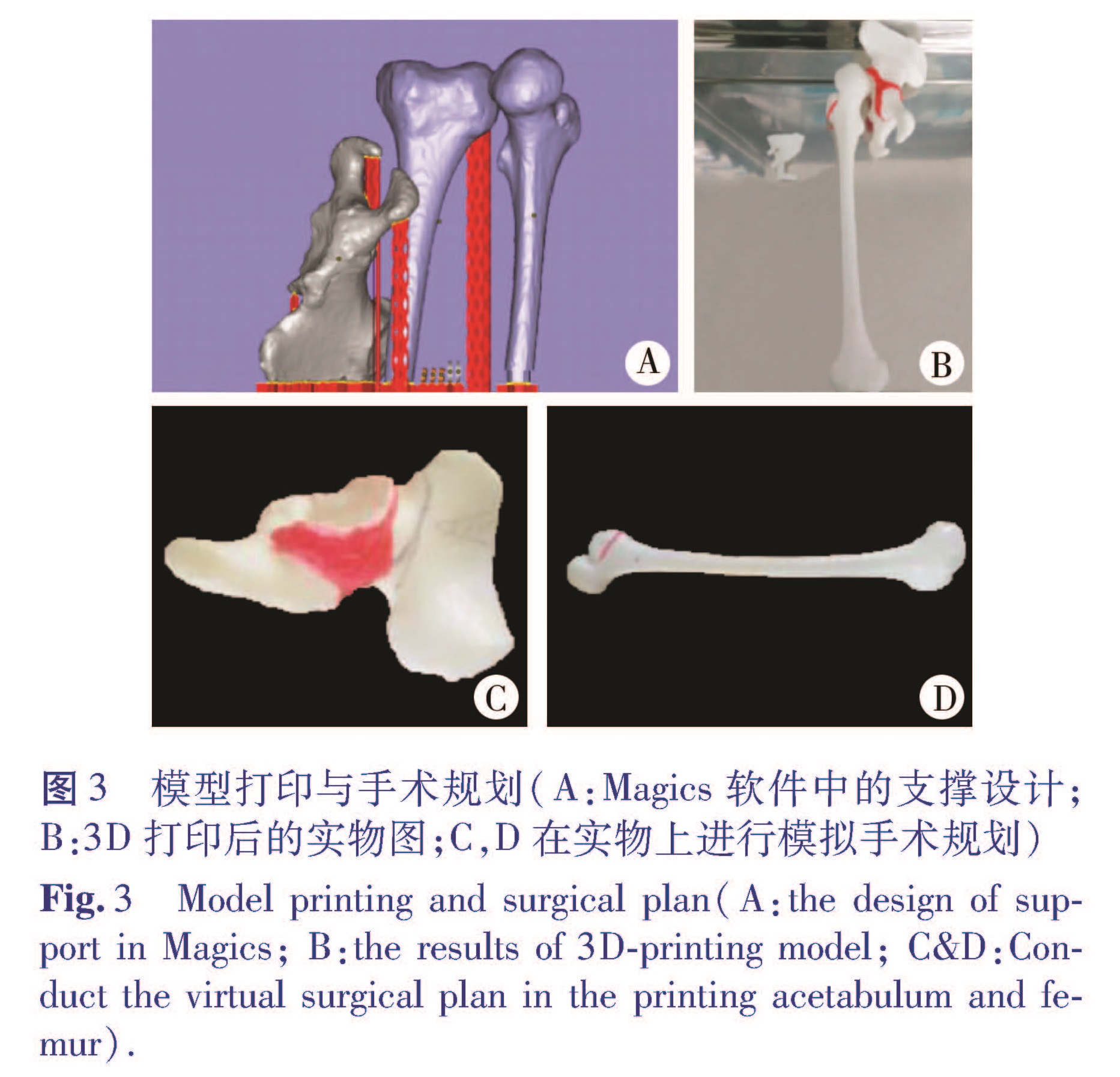
目的 探讨3D打印技术在儿童发育性髋关节脱位手术策略中的应用价值。方法 将2015年1月到2015年12月间由本院收治的18例发育性髋关节脱位患儿随机分组成3D打印组(n=8)和常规组(n=10)。3D打印组通过3D打印技术制作仿真模型以及手术导板,制定个体化手术方案。测量数字模型与打印模型在形态学上的差异。分析两组手术时间、出血量、辐射次数以及住院费用等情况。术后随访采用Mackay和Severin评分标准进行评价。结果 测量3D数字模型获得颈干角153.7°±10.9°; 前倾角45.3°±7.3°; 髋臼长轴(47.7±7.79)mm; 短轴(39.7±7.14)mm; 髋臼面积(1932±723)mm2; 髋臼体积(6569±738)mm3; 打印模型颈干角157.3°±7.4°; 前倾角51.2°±3.7°; 髋臼长轴(46±8.24)mm; 短轴(40.2±6.06)mm; 髋臼面积(1751±421)mm2; 髋臼体积(6 233±506)mm3; 与数字模型相比差异无统计学意义(P>0.05)。3D打印组中4例Salter联合截骨; 2例Pemberton联合截骨; 1例Dega联合截骨; 1例Chiari内移截骨; 常规组中5例Salter截骨联合截骨,3例Pemberton截骨,2例Dega截骨。3D打印组平均手术时间(2.82±0.42)h,出血量(285±40)mL,术中透视次数(5.7±1.0)次。常规组手术时间(3.4±0.48)h,出血量(355±57)mL,术中透视次数(14±2.9次)。3D打印组较常规组手术时间有缩短,出血量和术中透视次数也减少,差异有统计学意义(P<0.01)。,3D打印组为(27 686±1401)元; 常规组为(26 934±2 893)元,患儿总治疗费用并无增加(t=0.685,P=0.501)。两组患儿术后均获得随访,平均随访时间0.6年。Mackay评分优良率:3D打印组为87.5%(7/8),常规组90%(9/10); 两组比较无统计学差异(χ2=0.028,P=0.867)。Severin评分优良率:3D打印组为100%(8/8),常规组90%(9/10),两组比较无统计学差异(χ2=0.847,P=0.357)。结论 3D打印与计算机辅助导板设计技术为儿童髋关节发育不良的个体化手术规划策略提供了良好的辅助工具,具有较好的临床应用价值。
Objective To explore the application of 3D printing in surgical plan of developmental dislocation of hip(DDH)in children. Methods 18 children of DDH from 2015 Jan to Dec were randomly divided into two groups: 3D printing group and normal group. Simulation model and guided template were made by 3D printing for individualized surgical plan. The variance between digital model and entity were measured via neck shaft angle, anteversion angle, axis of acetabulum, volume and surface of acetabulum. The surgical time, amount of blooding, radiation and hospitalization expense were analyzed. The score of Mackay and Severin criterion were applied to evaluate the affected hip function. P<0.05 was regarded as statistically significant. Results Neck shaft angle and anteversion angle in digital model were 153.7°±10.9° and 45.3°±7.3° respectively, which in entity were 157.3°±7.4° and 51.2°±3.7° respectively. Long axis was(47.7±7.79)mm while short axis was(39.7±7.14)mm in digital model. Meanwhile, long axis was(46±8.24)mm with short axis(40.2±6.06)mm in entity. There was no significant difference between the two results. Moreover, the volume and surface of digital model was(6 569±738)mm3 and(1 932±723)mm2 respectively, whereas the entity was(6 233 ± 506)mm3 and(1 751 ± 421)mm2 in volume and surface. During 3D printing group, 4 cases were undergoing combined salter osteotomy, 2 cases combined Pemberton osteotomy, 1 case combined Dega osteotomy and 1 case Chiari osteotomy. In normal group, 5 cases underwent combined salter osteotomy, 3 cases Pemberton osteotomy and 2 cases osteotomy. In normal group, the mean surgical time was 3.4±0.48 h, with mean amount of blooding(355±57)mL and mean radiation(14±2.9)times.meanwhile, in 3D printing group, the mean surgical time was(2.82±0.42)h, mean amount of blooding 2 was(85±40)mL and mean radiation was(5.7±1.0)times, which apparently shorter than the normal group(P<0.01). The cost of 3D printing group was ¥2 768±1 401, Meanwhile, the cost of normal group was ¥26 934±2 893, which was no significant variance(t=0.685,P>0.05). All cases were followed-up to 0.6 years. The excellent-good ratio with Mackay criterion in 3D printing group was 87.5% while 90% in normal group, there was no obviously difference between two groups(χ2=0.028,P=0.867). Meanwhile, the excellent-good ratio with Severin criterion in 3D printing group was 100% while 90% in normal group, there was no significant difference between the two groups either(χ2=0.847,P=0.357). Conclusion 3D printing and computed aided guided template provided a good method for individualized surgical plan of developmental dislocation of hip in children.



![表3 两组的临床与影像学评定标准的比较[n(%)]<br/>Table 3 Comparison of Mackay and Severin criterionbetween 3D printing and normal group[n(%)]](2018年04期/pic06.jpg)