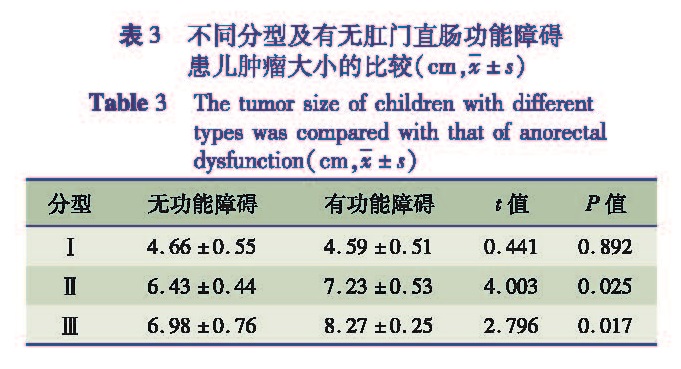
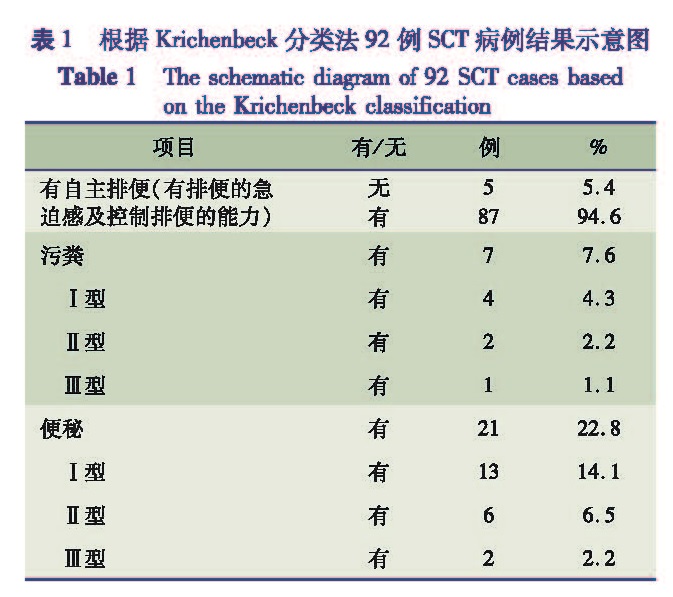
目的 评估新生儿骶尾部畸胎瘤术后的肛门直肠功能。 方法 对2008年2月至2014年1月在南京医科大学附属儿童医院新生儿外科手术治疗的新生儿骶尾部畸胎瘤患儿进行肛门直肠功能随访。记录资料包括:入院时年龄、症状和体征、手术方式、Altman分型和组织病理学分类。依据Krickenbeck分类法评估肛门直肠功能:有无自主排便、粪污等级和便秘等级。 结果 共计92例患儿(男/女=21/71)纳入本次研究,平均入院年龄(18.5 ± 6.6)d(1 ~ 25 d),Altman分型Ⅰ型57例(62.0%),Ⅱ型25例(27.1%),Ⅲ型10例(10.9%)。全部患者均手术切除肿瘤及尾骨。依据Krickenbeck分类法共28例(30.4%)患儿存在肛门直肠功能障碍,其中21例(22.8%)便秘(Ⅰ型13例,Ⅱ型6例,Ⅲ型2例),7例(7.6%)污粪(Ⅰ型4例,Ⅱ型2例,Ⅲ型1例)。不同性别、组织病理学分类、手术方式患儿术后肛门直肠功能障碍的发生率存在差异,但差异无统计学意义(χ2=3.795, P=0.051; χ2=3.341, P=0.188; χ2=1.737, P=0.187)。Ⅰ型、Ⅱ型和Ⅲ型患儿肛门直肠功能障碍发生率无统计学差异(χ2=0.040, P=0.980)。Ⅱ型和Ⅲ型患儿术后出现肛门直肠功能障碍和未发生肛门直肠功能障碍者肿瘤大小比较,差异有统计学意义(t=4.003,P=0.025; t=2.796,P=0.017)。 结论 新生儿骶尾部畸胎瘤患儿术后可能并发肛门直肠功能障碍,其中便秘最常见,小部分患儿存在污粪。
Objective Evaluate the neonates anorectal function after undergoing SCT resection. Methods A retrospective review of anorectal functional with SCT patients in our center(Department of Neonatal Surgery, Children's Hospital of Nanjing Medical University)was performed. Materials were recorded as follows: age at admission, symptoms and signs, surgical procedures, classification of Altman's, classification of histopathology. The anorectal function of the patients was followed-up with Krickenbeck's classification, focusing on free defecation, fecal contamination levels and constipation levels. Results A total of 92 SCT neonates were included in this study from February 2008 to January 2014. 21 boys and 71 girls with a mean age of 18.5±6.6 days(range 1d-25d)underwent excision of SCT in the neonatal period. With the Altman's classification system, 57 patients(62.0%)were classified as type Ⅰ, 25 cases(27.1%)type Ⅱ and 10 cases(10.9%)type Ⅲ. In all cases, 28 patients(30.4%)had anorectal dysfunction, including 7 cases(7.6%)of soiling(4 cases type Ⅰ, 2 cases type Ⅱ and 1 case type Ⅲ), and 21 cases(22.8%)of constipation(13 cases type Ⅰ, 6 cases type Ⅱ and 2 cases type Ⅲ). The incidence of postoperative anorectal dysfunction was not significantly difference with sex, histopathological classification, and surgical approaches(χ2=3.795, P=0.051; χ2=3.341, P=0.188; χ2=1.737, P=0.187). There is no significantly difference among type Ⅰ, type Ⅱ or type Ⅲ(χ2=0.040, P=0.980). There are significantly difference in the size of SCT among type Ⅱ or type Ⅲ(t=4.003,P=0.025; t=2.796,P=0.017). Conclusion Functional results after resection of neonatal(type Ⅰ,Ⅱ,Ⅲ)of SCT are excellent. Constipation is relatively common, with only a small number of patients reporting problems with fecal.
![表2 术后肛门直肠功能障碍的发生率与性别、组织病理学分类、手术方式的比较[n(%)]<br/>Table 2 The incidence of postoperative anorectal dysfunc-tion was compared with sex, histopathological classification, and surgical approaches [n(%)]](2018年01期/pic02.jpg)