基金项目:四川省教育厅基金重点资助项目(12ZA052) 通信作者:王城,E-mail:wangchengemail@126.com
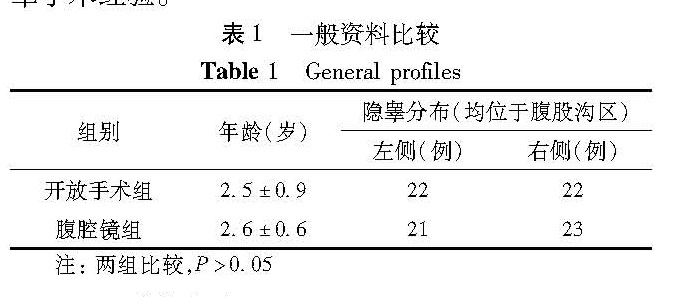
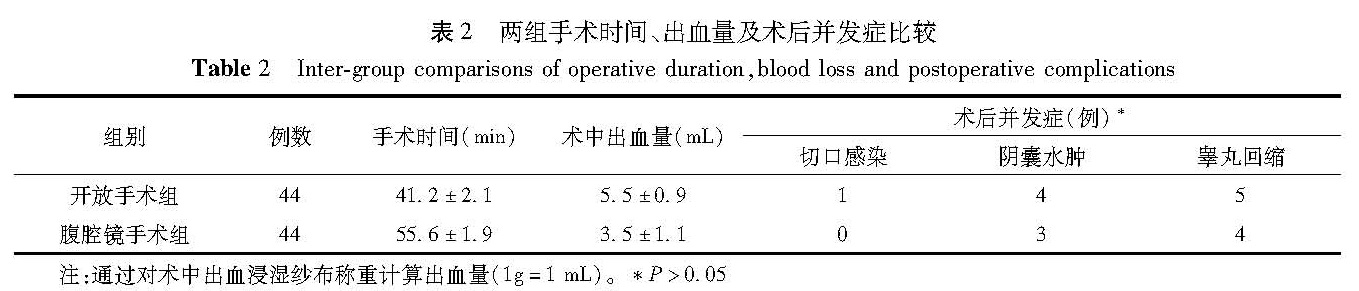
目的 比较腹股沟横行小切口与腹腔镜下睾丸下降固定术在腹股沟区隐睾中应用的优缺点。 方法 选择川北医学院附属医院小儿外科自2014年3月至2015年9月明确诊断为腹股沟区隐睾症的患儿88例,年龄1.2~4岁,平均年龄2.6岁; 按随机分组原则采取两种手术方式:开放手术组采用腹股沟横行小切口经腹膜外游离下降睾丸,阴囊小切口固定; 腹腔镜手术组采用腹腔镜下腹腔内游离睾丸,阴囊小切口固定; 分别对两组手术时间、睾丸下降后位置、术后并发症、手术前及术后半年双侧睾丸超声随访结果进行对比分析。 结果 开放手术组平均手术时间为(41.2±2.1)min,腹腔镜组为(55.6±1.9)min。腹腔镜手术组患儿术中出血量较开放组少,经统计学分析差异有意义。术后7 d及6个月查两组患侧睾丸下降位置发现:开放手术组44例睾丸均可降至阴囊内,其中5例位于阴囊入口处; 腹腔镜手术组44例睾丸均可降至阴囊内,其中4例位于阴囊入口处; 术后6个月患侧睾丸超声显示患侧睾丸发育较对侧稍差。 结论 在腹股沟区隐睾患儿中,腹腔镜下睾丸下降术在手术时间及术后效果上并无明显优势。建议对于腹股沟区隐睾应严格掌握腹腔镜手术指征,对于内环口及以上部位隐睾首选腹腔镜探查及腹腔镜下隐睾下降术。
Objective To compare the clinical advantages and disadvantages of transverse groin mini-incision versus laparoscopic orchiopex. Methods From March 2014 to September 2015,a definite diagnosis of inguinal cryptorchidism was made for 88 children with a mean age of 2.6(1.2~4)years. They were randomized into two groups of open surgery and laparoscopy(n=44 each). A small transverse groin incision was adopted for open surgery. Unilateral testicles were liberated and fixed with a small scrotum incision. Inter-group comparisons were made with regards to operative duration,testicular descent position,postoperative complications and ultrasonic results of bilateral testicles at pre-operation and 6 months. Results The average operative duration was shorter in open surgery group than that in laparoscopic group(41.2 vs 55.6 min). The number of intraoperative blood loss in the laparoscopic group was significantly lower than in the open surgery group.At Day 7,re-examinations of testicular descent indicated 44 vs 44 testis in scrotum and 5 vs 4 below scrotum inlet in open surgery versus laparoscopic group. At 6 months,bilateral testicular ultrasound showed ipsilateral slightly worse testicular development than contralateral organ. And there was no inter-group statistical significance. Conclusion s For Inguinal cryptorchidism,laparoscopy has no obvious advantage of operative duration and postoperative outcomes.Surgical indications should be should be strictly controlled for laparoscopic inguinal cryptorchidism. Laparoscopic orchidopexy is reserved for cryptorchidism above inner mouth.