通信作者:孙晓毅,E-mail:xysun@tjh.tjmu.edu.cn
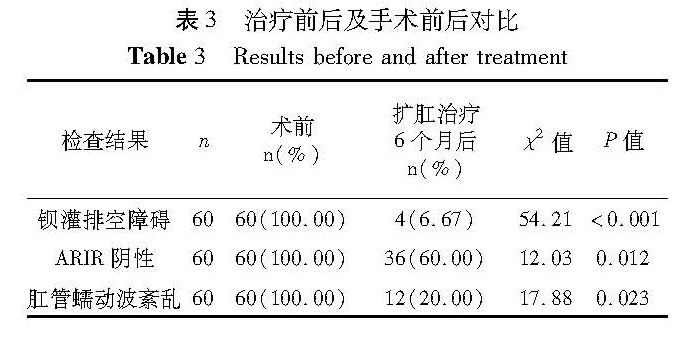
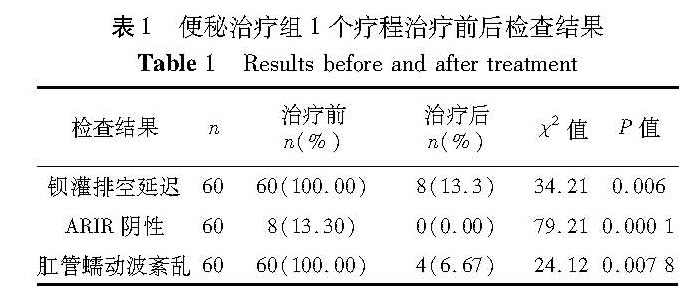
目的 评估扩肛治疗在婴幼儿便秘以及巨结肠根治术后处理中的疗效。 方法 对60例功能性便秘婴幼儿(为便秘治疗组)和60例经肛门巨结肠根治术后1个月的患儿(经肛门巨结肠根治术组)运用本院专利扩肛器分别行扩肛治疗,并进行排便功能问卷调查、结肠钡灌肠和肛门直肠测压检查,对扩肛前后肛肠功能进行综合评价。 结果 便秘治疗组60例经过扩肛治疗后,50例便秘消失(每日均排大便); 8例便秘好转(偶有停止排便2~3 d,干预后恢复); 2例无效; 复查结肠钡灌排空延迟,RAIR阴性率、肛管蠕动波紊乱较扩肛前明显减少(P<0.01)。经肛门巨结肠根治术(Soave)组60例于术后1个月行扩肛治疗,随访6个月后,42(70%)例排便次数逐渐减少至每日1~2次,复查钡灌排空延迟,RAIR阴性率、肛管蠕动波紊乱较扩肛前明显减少(P<0.05)。 结论 扩肛治疗对于婴幼儿功能性便秘而言,可以建立反射,刺激便意; 促进蠕动,缓解肛压; 阻断肠神经元病变的继续发展。对于巨结肠根治术后患儿而言,可以扩开瘢痕,使排便通过无阻力; 促进新建直肠顺应性恢复; 促进直肠肛管抑制反射建立; 促进蠕动,缓解肛压,减少肠炎发生,最终使肛管直肠排控便机制达到正常。
Objective To explore the efficacies of anal dilatation in the treatment of constipation and post-operation of Hischsprung's disease in children. Methods Sixty functional constipation infants and 60 children undergoing transanal one-stage pull-through operation for Hirschsprung's disease were selected for using our self-patented anal dilating device. During a follow-up period of at least 6 months, their stooling patterns were examined with the informed parental questionnaire. Barium enema, defecography and anorectal manometry were performed for evaluating stooling patterns, colonic motility and sphincter function. Results In the functional constipation group, stooling patterns were generally fine after anal dilatation. Occasional constipation in 8 cases was relieved after interventions and constipation persisted another 2 cases. The rate of colonic delayed emptying in post-treatment was significantly lower than that in pre-treatment(P<0.01). The negative rate of rectal anal inhibitory reflex(RAIR)and disturbance of anal peristaltic wave were also significantly lower post-treatment than that prior-treatment(P<0.01). In the postoperative group, the pattern of stooling decreased to once daily by anal dilatation for 6 months. The rate of colonic delayed emptying, negative rate of RAIR and disturbance of anal peristaltic wave post-treatment were significantly lower than that prior-treatment(P<0.01). Conclusion s Satisfactory outcomes of stooling function, colonic motility and sphincter performance may be obtained with anal dilatation in both functional constipation and postoperative groups.
![表2 患儿术后6个月时排便情况[n(%)]<br/>Table 2 Postoperative defecation frequency[n(%)]](2017年02期/pic19.jpg)