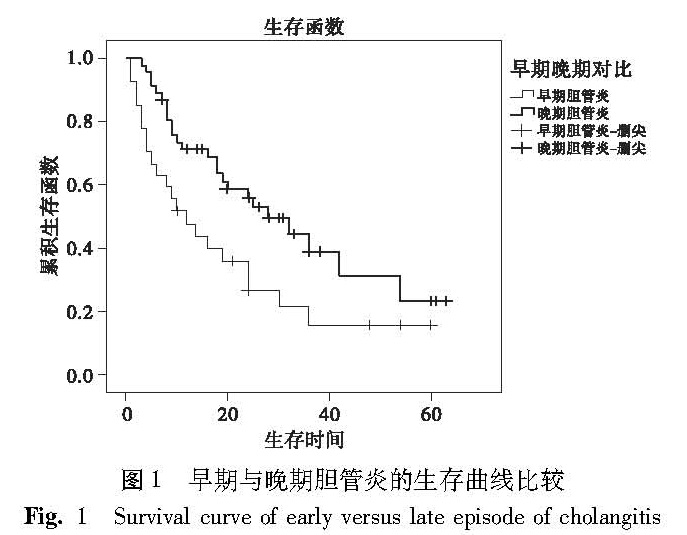
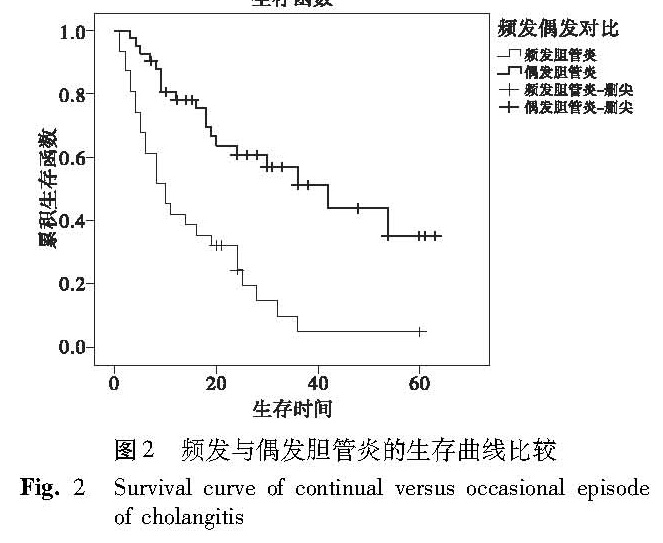
目的 分析102例胆道闭锁Kasai术后胆管炎的发生情况,探讨其与预后的关系,以加强对胆道闭锁Kasai术后胆管炎的诊治。 方法 对2009年1月至2016年6月山西省儿童医院行Kasai手术并统一术后治疗方案的102例胆道闭锁患儿进行随访,随访内容包括Kasai术后胆管炎发作的时间、次数及频率,术后是否遵嘱服药、治疗情况及疗效等,分析胆管炎与自体肝存活率、黄疸消退率及肝功能恢复等预后情况的关系。 结果 术后未发生胆管炎组及胆管炎发作组2年累计自体肝存活率分别为65.5%和41.1%(P=0.030)。早期胆管炎发作组和晚期胆管炎发作组其2年累计自体肝存活率分别为22.2%和52.2%(P=0.013)。早期胆管炎发作组和晚期胆管炎发作组的黄疸消退率分别为33.3%和67.4%(P=0.007)。早期胆管炎发作组和晚期胆管炎发作组的肝功恢复良好率为44.4%和73.9%(P=0.023)。频发胆管炎组与偶发胆管炎组的2年自体肝生存率分别为19.4%和57.1%(P=0.002),频发胆管炎组和偶发胆管炎组的黄疸消退率分别为38.7%和66.7%(P=0.001),频发胆管炎组和偶发胆管炎组的肝功能恢复良好率分别为45.2%和76.2%(P=0.008)。 结论 胆管炎尤其早期、频发胆管炎影响自体肝存活率、黄疸消退率及肝功能恢复,最终影响胆道闭锁预后。提高医患双方对胆道闭锁术后胆管炎的认识,加强对胆管炎的防治,对提高胆道闭锁生存率有重要意义。
Objective To explore the characteristics of cholangitis in patients with biliary atresia after Kasai operation and seek measures of improving the survival rate. Methods A retrospective review was conducted for 102 patients undergoing Kasai operation between January 2009 and June 2016. Results The 2-year survival rates of cholangitis attack or not were 41.1% and 65.5%(P=0.030). The 2-year survival rates of early episode of cholangitis group(EC)and late episode of cholangitis(LC)group were 22.2% and 52.2%(P=0.013). In EC and LC groups, jaundice subsiding rates were 33.3% and 67.4%(P=0.007)and liver function recovery rates 44.4% and 73.9% respectively(P=0.023). The 2-year survival rates of continual episode of cholangitis group(CC)and occasional episode of cholangitis(OC)group were 19.4% and 57.1%(P=0.002). In CC and OC groups, jaundice subsiding rates were 38.7% and 66.7%(P=0.001)and liver function recovery rates 45.2% and 76.2% respectively(P=0.008). Conclusion s The stage and frequency of cholangitis have statistically significant differences in the outcomes after Kasai operation. It is vital for surgeons to enhance the cognition and strengthen the prevention and treatment of cholangitis after Kasai operation. Then it is feasible to improve the survival rate of biliary atresia.
![表1 Kasai术后胆管炎与预后[n(%)]<br/>Table 1 Clinical data of 102 cases with BA after Kasai operation](2017年02期/pic15.jpg)