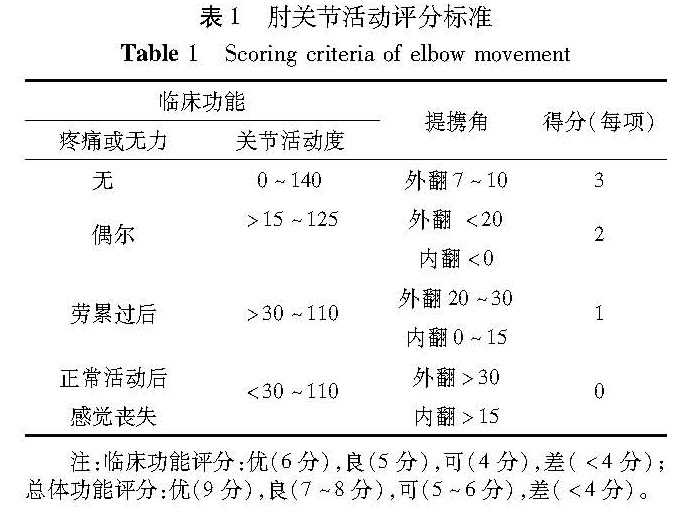
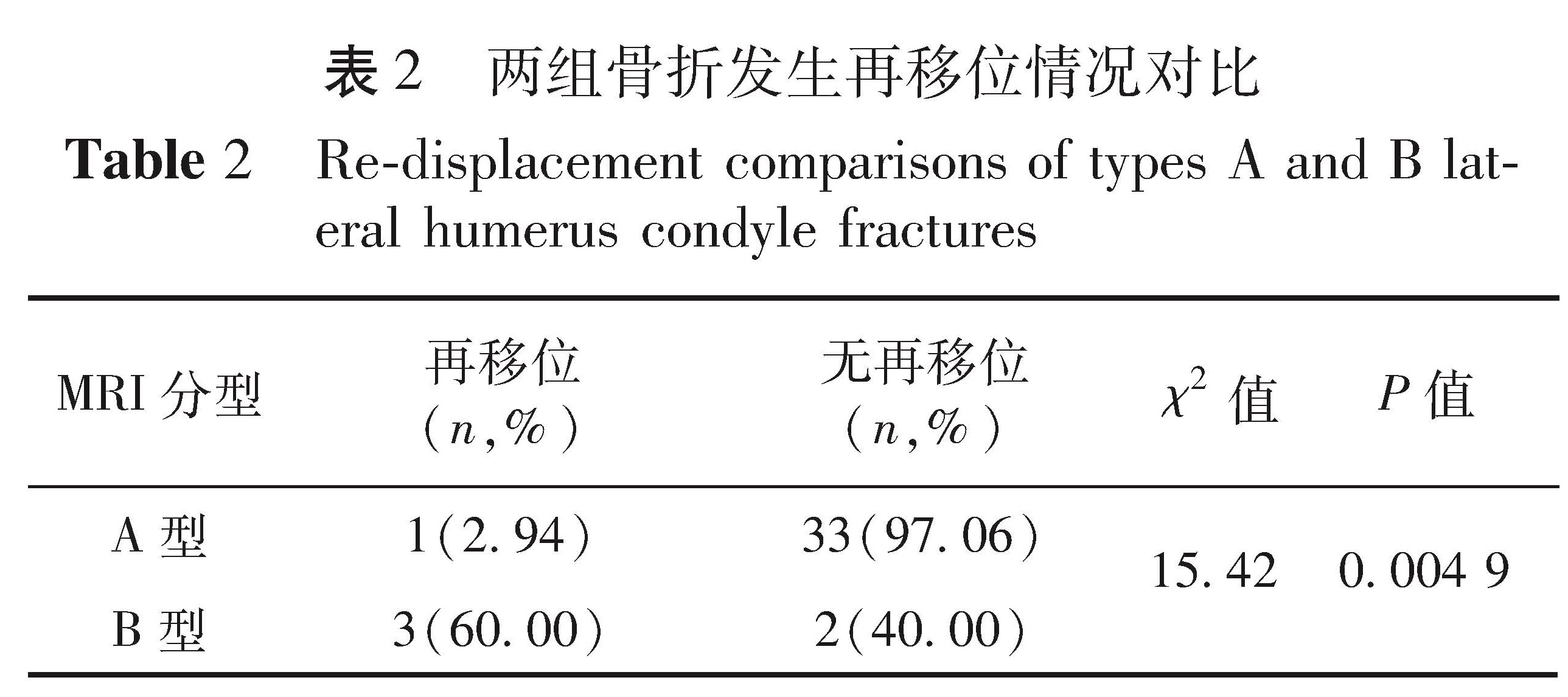
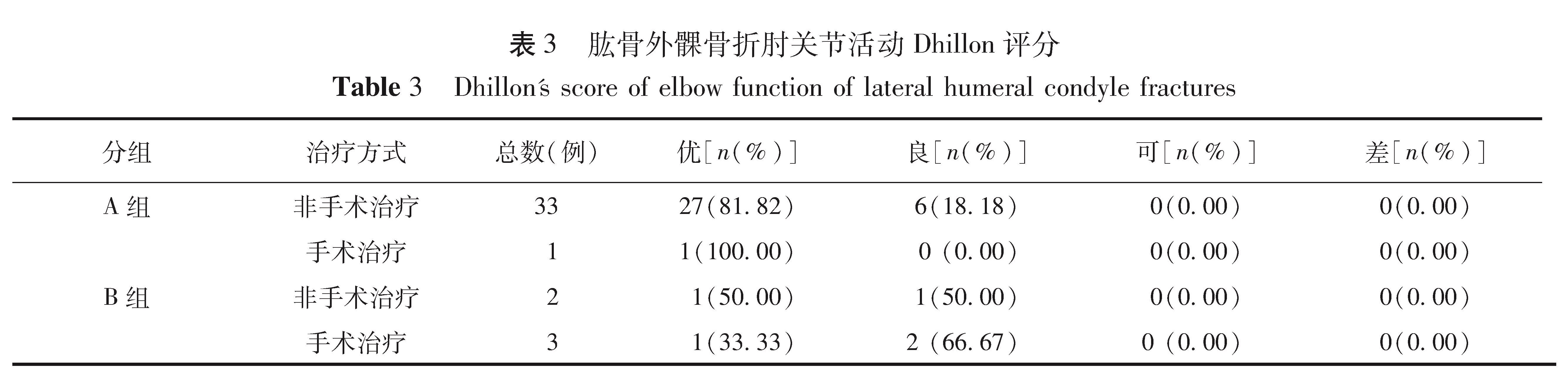
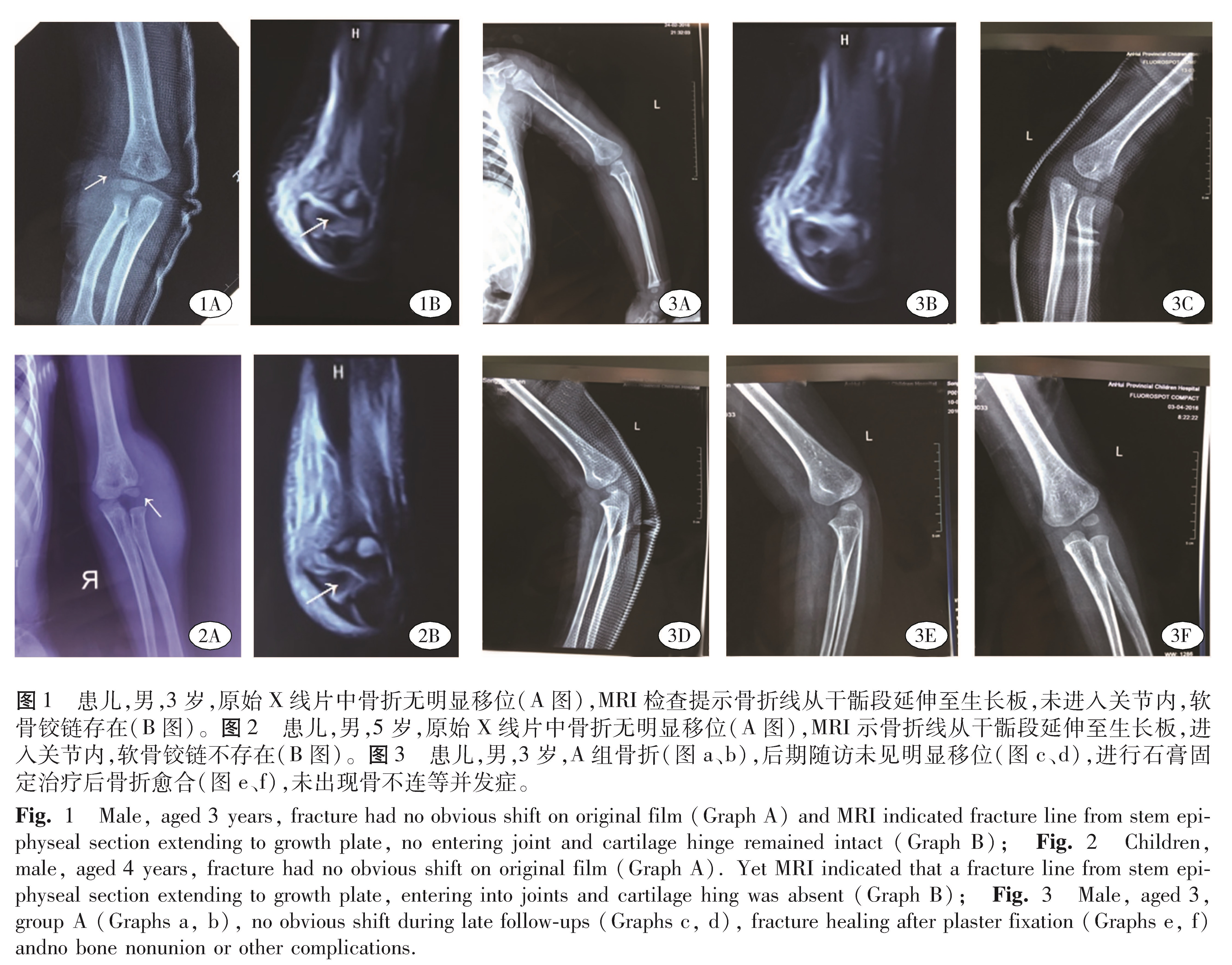
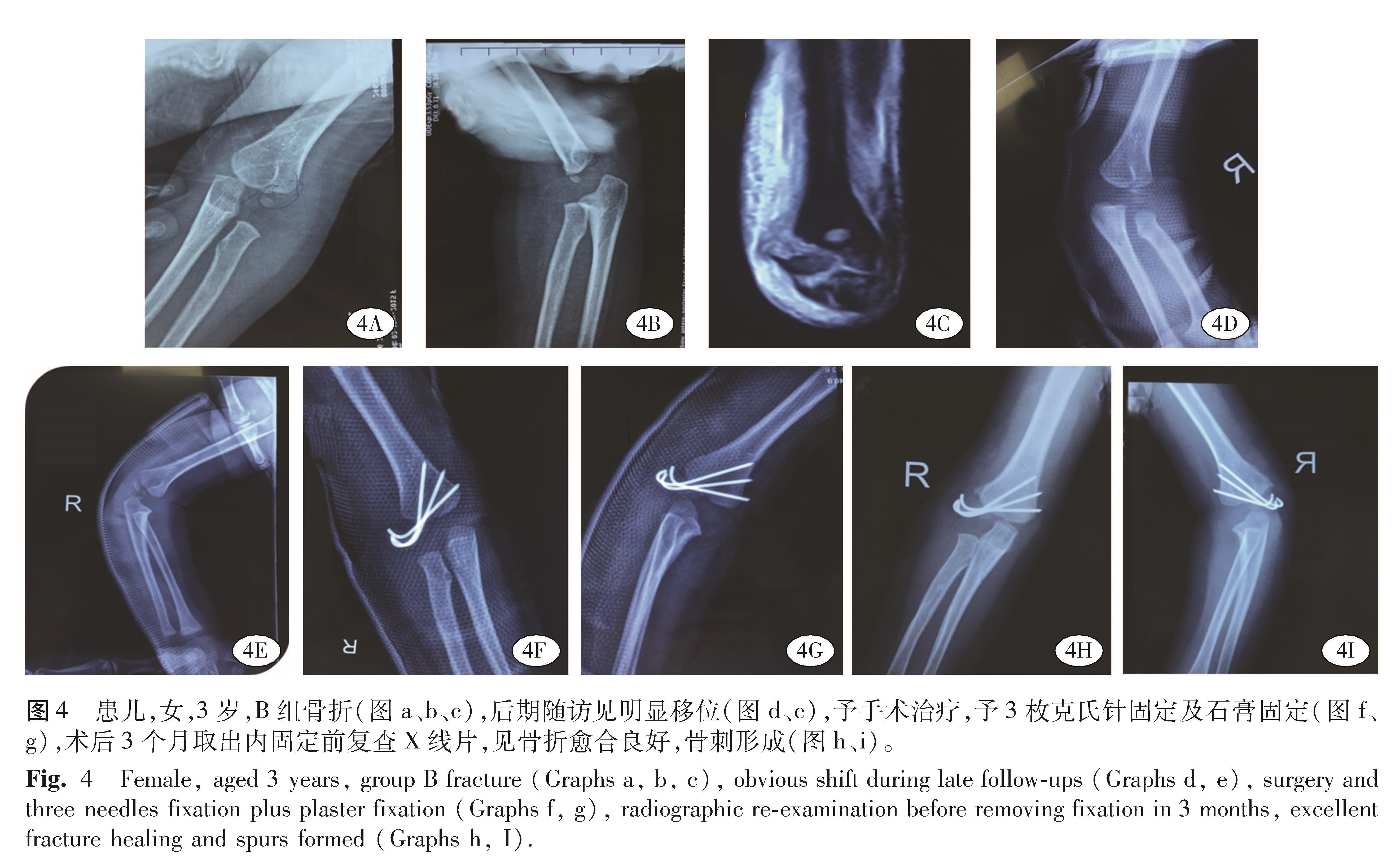
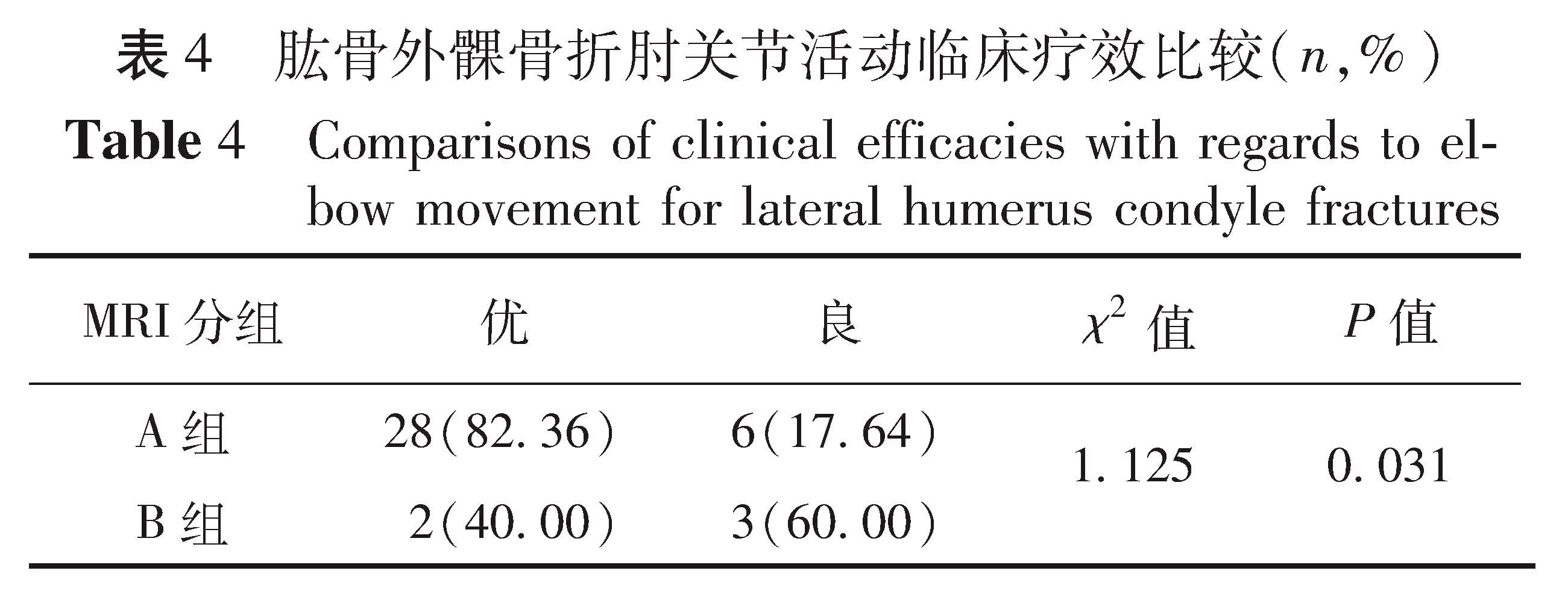
目的 探讨通过影像学磁共振技术(MRI)判定JacobⅠ型肱骨外髁骨折患儿骨折的稳定性,并指导其治疗方案的选择。 方法 选取2015年10月至2016年9月于本院就诊且资料完整的JacobⅠ型肱骨外髁骨折病例39例。根据MRI检查结果将其分为两组:A组——骨折线从干骺端至生长板,未穿过生长板,关节面完整,软骨铰链存在; B组——骨折线穿过生长板,延伸至关节面,软骨铰链不存在。A、B两组骨折均先予石膏固定,定期随访; 对随访中无再移位病例继续予以石膏固定; 对随访中移位明显加重者予手术治疗。治疗后期依据Dhillon评分,比较所有患儿骨折愈合及肘关节功能情况。 结果 A组有33例无再移位,1例再移位明显加重者予手术治疗; B组有2例无再移位,3例再移位明显加重者予手术治疗。A组骨折再移位率为2.9%,B组骨折再移位率为60%,与A组比较,B组骨折经非手术治疗后再移位的发生率明显增加( χ2= 15.42,P=0.004 9),且B组骨折预后评分占优率明显降低( χ2= 1.125,P=0.013)。 结论 关于JacobⅠ型肱骨外髁骨折的稳定性与治疗方案,仅依靠X线平片检查结果是不够的,MRI更容易显示儿童JacobⅠ型肱骨外髁骨折的稳定性,这为临床治疗儿童JacobⅠ型肱骨外髁骨折提供了理论依据。
Objective To explore the stability and choice of treatment in children's Jacob typeⅠ lateral humeral condyle fracture by magnetic resonance imaging(MRI). Methods From October 2015 to September 2016, 29 children with Jacob typeⅠlateral humeral condyle fractures received MRI plus plaster immobilization and their medical data were collected. The fractures were classified into groups A(n=34)and B(n=5)by the extent of fracture line on MRI. In group A, the line coursed from lateral metaphysis to growth plate but not through it and cartilage hinge remained intact. In group B, the line crossed growth plate to enter joint space and cartilage hinge was absent. Regular follow–ups were conducted by plain radiograph. Based upon the Dhillon rating, healing of fractures and elbow function were compared. Results In group A, there were non-re-displacement(n=33)and re-displacement(n=1). In group B, non-re-displacement(=2)and re-displacement(n=3). Non-re-displaced cases discontinued plaster immobilization and significantly aggravated re-displaced ones were re-operated. And 2.9% group A and 60% group B underwent re-displacement. Compared to group A, group B re-displaced more significantly(P<0.01)and the prognostic score of group B decreased obviously(P<0.05). Conclusion s Plain radiograph is insufficient for making an accurate decision regarding stability and choice of treatment. And MRI can distinguish potentially unstable fractures. It provides theoretical rationales for treating Jacob typeⅠhumerus lateral condyle fracture in children.