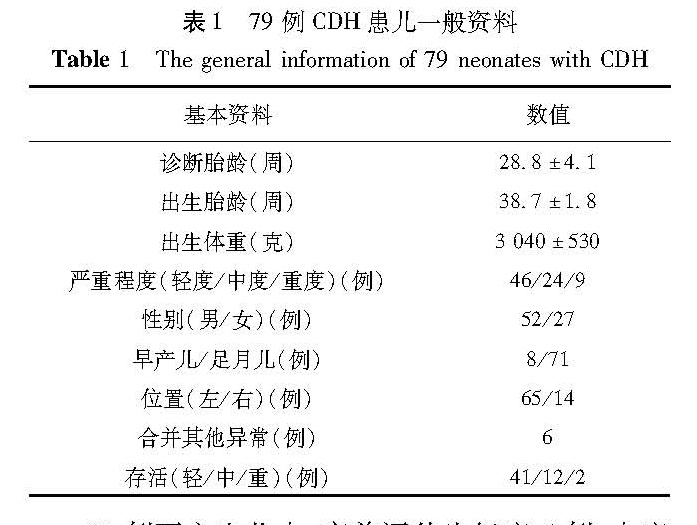
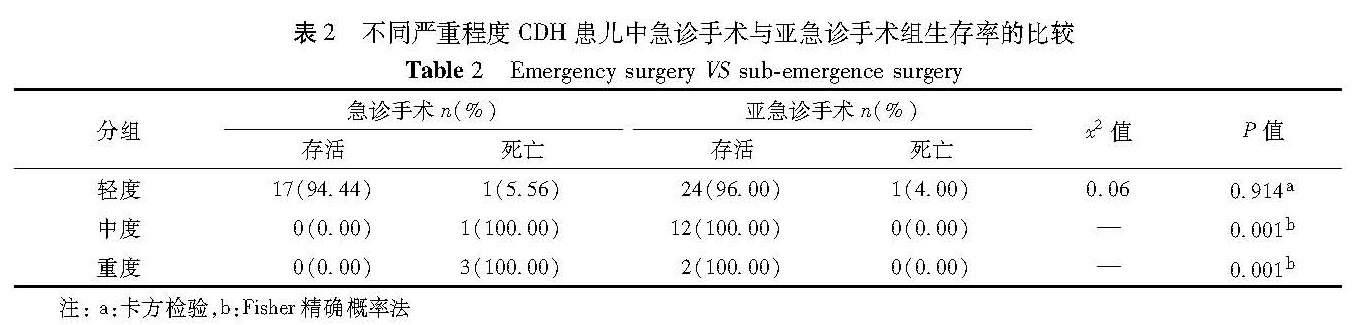
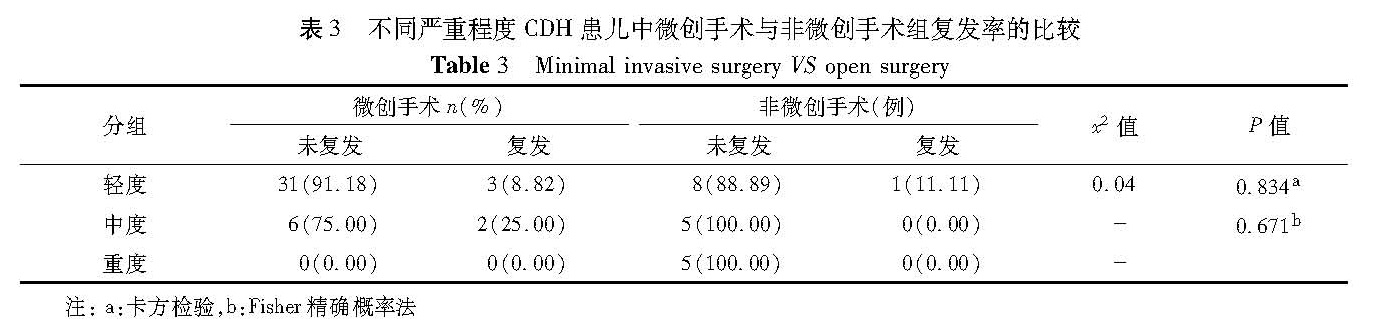
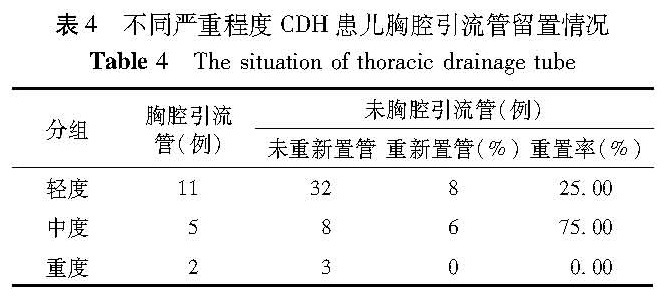
目的 总结先天性膈疝的围手术期管理经验,探讨产前诊断先天性膈疝的手术治疗时机、手术方法与临床疗效。 方法 2014年1月至2016年11月通过产前诊断确诊为先天性膈疝患儿79例。根据LHR、O/E LHR以及肝脏位置将患儿分为轻、中、重度三组,对比分析各组手术时机、手术方法以及胸腔引流管放置情况。依据手术时机分为急诊手术组和亚急诊手术组; 依据手术方法分为非微创组(经腹或经胸膈肌修补术)和微创组(胸腔镜下膈肌修补术)。 结果 79例患儿中,产前评估轻度46例,中度24例,重度9例。产前诊断评估与出生后评估结果Kappa值为0.695,具有较好一致性。治愈55例,死亡24例。比较轻度CDH患儿急诊手术和亚急诊手术,两组存活率差异无统计学意义(x2 =0.06,P=0.914); 分别比较中度、重度CDH患儿急诊手术和亚急诊手术,两组存活率差异有统计学意义(P=0.001); 79例CDH患儿中,轻、中度患儿复发率差异无统计学意义(P>0.05)。32例未留置胸腔引流管的轻度CDH患儿中,8例在后期因胸腔积液行胸腔闭式引流; 13例手术治疗的中度CDH患儿,8例未留置胸腔引流管; 中度CDH患儿6例在后期因胸腔积液行胸腔闭式引流,1例术后死亡; 5例手术治疗的重度CDH患儿,3例未留置胸腔引流管,术后死亡。 结论 手术时机对于轻度CDH预后无影响; 对于中重度CDH,呼吸循环功能稳定后延期手术可以提高存活率; 微创手术是一种安全、可行的手术方法; 中重度CDH术后需留置胸腔引流管。
Objective o summarize the experience of the perioperative management of congenital diaphragmatic hernia(CDH)in neonate who diagnosed in utero. Methods 79 patients with CDH were diagnosed in utero and treated on between January 2014 and November 2016 at our institution were retrospectively reviewed. They were divided into mild, moderate and severe groups according to LHR, O/E LHR and liver location. Operation time were divided into emergency operation and sub-emergency operation. Surgical modalities included mini-invasive and open surgery. Results Among 79 patients, there were 46 mild cases, 24 moderate cases and 9 severe cases during prenatal evaluation. For mild cases, no significant difference existed in operative timing or approach. For moderate and severe patients, there were statistically significant between operation timing(P=0.001). For moderate cases, there was no statistical difference in recurrence rate. Among 32 mild non-draining CDH cases, 8 of them required closed thoracic drainage due to pleural effusion. Among 8 moderate non-draining CDH cases, 6 of them underwent closed thoracic drainage due to pleural effusion and one case died after surgery. Among 5 severe cases, 3 non-draining cases died. Conclusion s For moderate and severe CDH, the survival rate could be improved when surgery were operated after circulatory and respiratory function on stability level, and chest drainage should be placed. Mini-invasive surgery is a technically feasible and safe procedure.